Abstract
Background
Prescription opioids were a major initial driver of the opioid crisis. States have attempted to reduce overprescribing by enacting policies that limit opioid prescriptions, but the impacts of such policies on new prescribing and subsequent transitions to long-term use are not fully understood.
Objective
To examine the association of implementation of a state prescribing limits policy with opioid prescribing and transitions to long-term opioid use.
Design
Interrupted time series analyses assessing trends in new opioid prescriptions and long-term use before and after policy implementation.
Patients
A total of 130,591 New Jersey Medicaid enrollees ages 18–64 who received an initial opioid prescription from January 2014 to December 2019.
Interventions
New Jersey’s opioid prescribing limit policy implemented in March 2017.
Main Measures
Total new opioid prescriptions, percentage of new prescriptions with >5 days’ supply, and transition to long-term opioid use, defined as having opioid supply on day 90 after the initial prescription.
Key Results
Policy implementation was associated with a significant monthly increase in new opioid prescriptions of 0.86 per 10,000 enrollees, halving the pre-policy decline in the prescribing rate. Among new opioid prescriptions, the percentage with >5 days’ supply decreased by about 1 percentage point (−0.76 percentage points, 95% CI −0.89, −0.62) following policy implementation. However, policy implementation was associated with a significant monthly increase in the rate of initial prescriptions with supply on day 90 (9.95 per 10,000 new prescriptions, 95% CI 4.80, 15.11) that reversed the downward pre-implementation trend.
Conclusions
The New Jersey policy was associated with a reduction in initial prescriptions with >5 days’ supply, but not with an overall decline in new opioid prescriptions or in the rate at which initial prescriptions led to long-term use. Given their only modest benefits, policymakers and clinicians should carefully weigh potential unintended consequences of strict prescribing limits.
Similar content being viewed by others
INTRODUCTION
Prescription opioids are widely viewed as a main initial driver of the opioid overdose epidemic.1 Although rates of progression to opioid use disorder (OUD) among those who initiate prescribed opioids are low,2,3 a range of policies have emerged to restrict opioid prescribing.4,5 These policies aim to lessen exposure to opioids and prevent progression from use for short-term pain relief to long-term, chronic use, which has been criticized as risky and potentially ineffective.6,7,8,9 In March 2017, New Jersey implemented restrictions that limit initial opioid prescriptions for acute pain to a 5-day supply of the lowest effective dose.10,11 For subsequent prescriptions, the policy also requires providers to discuss prescription opioid risks and alternative treatments; develop and periodically review pain management contracts; assess development of dependence; use the state PDMP; and decrease opioid prescribing or transition to alternative pain management strategies.11
Prior research has shown mixed findings on the association of opioid prescribing policies with prescribing practices and related outcomes. While some studies found associations between prescribing restrictions and reductions in initial days’ supply,12,13,14,15,16,17 others showed no or limited effects on other prescription characteristics, including dosage,13,18 opioids distributed,13,19 proportion of patients receiving opioid prescriptions, and average prescription duration and dose.20 Effects vary across states and outcomes; for example, two studies found that prescription limits were associated with shorter initial prescription duration in Massachusetts but not Connecticut, and lower opioid dose in Connecticut but not Massachusetts.14,21 This heterogeneity highlights the need for evidence that accounts for unique policy provisions and the timing and context of implementation. Furthermore, prior research has largely focused on initial prescriptions without examining the association of prescribing limits with longer-term outcomes that are critical to evaluate policy implications. To address these gaps, this study examines the impact of NJ’s legislation on prescribing and outcomes among Medicaid beneficiaries, a population with high pain prevalence and elevated rates of opioid prescribing. The aims were to assess the impact of the NJ policy on (1) rates of initial opioid prescriptions; (2) the proportion of initial prescriptions with 5 or more days’ supply; and (3) transitions to long-term prescribed opioid use.
METHODS
Data and Sample
We analyzed de-identified NJ Medicaid claims data from January 2013 to March 2020 among individuals aged 18–64 who were not dually eligible for Medicare. We examined initial opioid prescriptions from January 2014 through December 2019, prior to the onset of pandemic-related health care disruptions. We restricted the sample to individuals with continuous Medicaid enrollment for 365 days prior to opioid prescriptions to identify initial prescriptions as defined in the legislation, which apply to patients with no opioid prescriptions in the prior year. For the long-term use outcome only, we required continuous enrollment for 90 days following the initial prescription. As specified in the policy exemptions, we excluded enrollees receiving hospice or palliative care, long-term care facility residents, and those with active cancer treatment (i.e., diagnoses for cancers commonly treated with opioids) in the 180 days prior to the initial prescription and in the 90 days after initial prescription for the long-term use outcome.
Pharmacy claims were linked with the First Databank MedKnowledge database22 by National Drug Codes to identify opioid prescriptions, excluding drugs for OUD treatment (Appendix Table A1). We used days’ supply on pharmacy claims to identify initial prescription duration and assess transitions to long-term use.
Outcomes
To assess the direct impact of the policy requirement to limit initial opioid prescriptions to 5 days’ supply, we calculated the monthly rate of new opioid prescriptions per 10,000 enrollees, overall and stratified by ≤5 or >5 days’ supply, and the percentage of new prescriptions with >5 days’ supply. We assessed the policy impact on transitions to long-term use, defined as the monthly rate per 10,000 new prescriptions with opioid supply on day 90 after the initial prescription, overall and stratified by ≤5 or >5 days’ supply. This measure aligned with the CDC definition of long-term use as 3 or more months7 and with the NJ law’s requirement to review opioid prescribing every 3 months.11 We attributed the outcome to the month of the initial prescription. In a sensitivity analysis, we tested an alternative measure of long-term use, calculated as the monthly rate per 10,000 initial prescriptions that resulted in 80%+ days’ supply in the first 90 days after the initial prescription.
Analysis
To evaluate policy effects, we used interrupted time series models to compare trends in opioid prescribing and transitions to long-term use after the policy was implemented to the pre-policy period.
To assess outliers, autocorrelation, and seasonality, we first plotted the unadjusted outcomes over time and their autocorrelation and partial autocorrelation functions. We performed Augmented Dickey-Fuller and KPSS tests to evaluate stationarity and accounted for autocorrelation and seasonality using auto-regressive integrated moving average (ARIMA) models. Models also adjusted for demographics by including monthly indicators of mean age, percentage of White, non-Hispanic patients, and percentage of female patients. We used the Census Bureau’s X-13-ARIMA-SEATS program23 integrated into the seasonal R package24 to automatically detect the best-fitting ARIMA model (Appendix Table A2). To confirm the absence of additional autocorrelation in final models, we plotted and examined model residuals and performed Ljung-Box tests.25
Using ARIMA-adjusted time series, we performed segmented regression with terms to estimate outcome trends over time (months), outcome levels in the pre-policy (January 2014–February 2017) and post-policy (March 2017–December 2019) periods, and an interaction of these terms to obtain estimates of the changes attributable to policy implementation, including immediate changes at the time of implementation and changes in outcome trends over time after implementation. For long-term use analyses, we excluded the 3 months before policy implementation because the 90-day follow-up period crossed the pre- and post-policy period.
We performed sensitivity analyses to assess robustness of findings to alternate specifications. For all outcomes, we estimated models with 12-month policy implementation lags to assess potential delays in effects, which categorized data between March 2017 and March 2018 in the pre-policy period. For new prescription rates and the percentage of new prescriptions with >5 days’ supply, we performed controlled interrupted time series analyses26,27,28 to assess trends for opioid relative to benzodiazepine and stimulant prescriptions. We selected these comparison medications due to their status as controlled substances and assessed whether findings were specific to opioid medications and whether similar policy effects existed for medications not subject to the policy. Analyses were conducted using SAS Enterprise Guide Version 8.3 and R Version 4.1.0. All study procedures were reviewed and approved by the Rutgers University Institutional Review Board.
RESULTS
We identified 158,143 new opioid prescriptions meeting study criteria from January 2014 through December 2019. The number of unique enrollees was 130,591, of whom 25,038 had more than one initial opioid prescription during the study period. Enrollees had a median age of 42.1, 67.2% were female, 30.1% were non-Hispanic Black, 37.0% non-Hispanic White, 18.6% Hispanic, and 14.3% non-Hispanic Other race.
Association of prescribing limits with changes in initial opioid prescriptions
Table 1 and Figure 1 present estimates of the association between policy implementation and new opioid prescribing rates per 10,000 Medicaid enrollees. New prescriptions were decreasing at a monthly rate of −1.62 per 10,000 (95% CI −1.80, −1.45) before policy implementation. While new prescriptions per 10,000 Medicaid enrollees continued to decrease at a rate of −0.76 (95% CI −0.96, −0.55) after policy implementation, this represents an attenuation in the pre-policy trend of 0.86 new prescriptions per 10,000 (95% CI 0.60, 1.13). Stratified analyses showed that post-implementation trend increases were driven by new prescriptions with ≤5-days’ supply, which increased by 0.67 (95% CI 0.57, 0.76) compared to an increase of 0.18 (95% CI 0.01, 0.36) for prescriptions with >5-days’ supply. Lagged sensitivity analyses produced similar results to primary models (Appendix Table A3, Figure A1). Sensitivity analyses comparing trends in new opioid prescription rates to those of benzodiazepines and stimulants similarly showed a positive trend change for opioids relative to the other medications (Appendix Table A4, Figures A2-A3).
The percentage of initial opioid prescriptions with >5 days’ supply increased at a modest rate in the pre-policy period (0.25%, 95% CI 0.16, 0.34), but implementation was associated with a significant trend decrease of −0.76% (95% CI −0.89, −0.62), resulting in a declining rate of opioid prescriptions with >5 days’ supply in the period after policy implementation (−0.51, 95% CI −0.61, −0.40) (Table 2, Fig. 2). Sensitivity analyses comparing trends in the percentage of new opioid prescriptions with >5 days’ supply to those of benzodiazepines and stimulants similarly found an association of the policy with a decreasing monthly trend for opioids relative to the other medications (Appendix Table A4, Figures A3-A4).
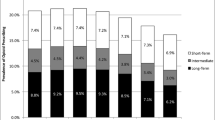
Association of prescribing limits with transitions to long-term receipt of prescribed opioids
Table 3 and Figure 3 show estimates of the policy’s association with the number of new prescriptions per 10,000 that progress to long-term receipt of opioids, defined as supply on day 90 after the initial prescription. The policy was associated with a significant monthly increase in prescriptions progressing to long-term use of 9.95 per 10,000 (95% CI 4.80, 15.11), reversing the pre-policy trend (−5.29, 95% CI −8.85, −1.73) to a monthly increase of 4.66 per 10,000 new prescriptions (95% CI 0.94, 8.38). These trends resulted in similar rates of approximately 1000 per 10,000 new prescriptions progressing to long-term use at the start (January 2014) and end of the observation period (December 2019). Stratified analyses showed that the policy was associated with an increase in the monthly rate of ≤5-day prescriptions progressing to long-term use of 10.05 per 10,000 new prescriptions (95% CI 5.71, 14.39) following a flat trend during the pre-policy period (1.00, 95% CI −1.81, 3.80), nearly doubling the number of new ≤5-day prescriptions resulting in long-term use from the pre-policy period (~500 per 10,000) to the end of the observation period (~1,000 per 10,000). Trends for new >5-day new prescriptions were similar to those for all new prescriptions.
Association of implementation of New Jersey prescribing limits policy with initial opioid prescriptions leading to long-term use, defined as opioid supply on day 90. Points represent ARIMA-adjusted monthly observations. Light shaded area is the 3-month washout period before policy implementation. Dark shaded area is the period after the policy was implemented.
Results of sensitivity analyses with a 12-month implementation lag were similar (Appendix Table A6, Figure A5). In the sensitivity analysis measuring long-term use as the monthly rate per 10,000 initial prescriptions with at least 80% days’ supply in the first 90 days, there was no association of the policy with an immediate change in long-term use rates at implementation and the post-policy trend flattened (Appendix Table A7, Figure A6).
DISCUSSION
Analyses of opioid prescribing in NJ Medicaid showed that implementation of a state law limiting initial days’ supply was associated with a reduction in the proportion of new prescriptions with >5 days’ supply, but not with an overall decline in new opioid prescriptions. In fact, while initial opioid prescriptions were declining before policy implementation, the policy was associated with a small increase that slowed the prior rate of decline. While the findings align with the policy goal to limit the duration of initial prescriptions, overall changes were relatively modest and may not have had a meaningful impact on opioid prescribing trends.
Prior studies of prescribing limits have also generally shown an association with shorter initial prescription duration12,13,14,15 but not overall prescribing trends.13,18,19,20 One possible explanation for the policy’s minimal effect on overall prescribing, as suggested by Sacks et al.,13 is that it defined a “reference point” (i.e., 5 days) signaling a safe threshold for initial opioid prescriptions, contributing to increases in initial short duration prescriptions after policy implementation with no impact on the rate of higher-risk, longer duration prescriptions. In other contexts, including diabetes treatment29,30 and childbirth,31 clinical guidelines with defined thresholds have had significant impacts on service delivery and may have led to unintended consequences, including increased health care use.32
This study extends findings of previous research on prescribing restrictions to downstream effects that are key to addressing the opioid epidemic. Policy implementation was associated with an immediate decline in new prescriptions resulting in long-term use, but increasing post-policy trends reversed this effect, resulting in no overall reduction in transitions to long-term use. We observed a lag in the trend reversal, which may be explained by policy elements related to long-term use (e.g., need for pain management contracts, requirement for periodic review of pain management plan) that deterred long-term prescribing immediately after implementation, with later increases in longer-term prescribing as providers became familiar with policy requirements. Trends also differed depending on initial days’ supply. For initial >5-day prescriptions, there was a decreasing pre-policy trend that became marginally positive after about a 115% increase following implementation, but to a lesser degree than ≤5-day prescriptions, which increased by over 1000% and nearly doubled the rate of ≤5-day prescriptions that had supply on day 90 by the end of the study period. One explanation for this shift is that the law required prescribers to issue ≤5-day prescriptions for patients with longer-term pain management needs, who, before the law, would have likely been issued >5-day prescriptions. Few other studies have examined transition to long-term use after initial opioid prescriptions, but one study similarly found that prescribing limits policies were not associated with decreases in opioid prescriptions in the 90 and 270 days following the initial prescription.13
Since 2016, more than 39 states have implemented prescribing limits policies,5 but growing evidence suggests these policies on their own had a minimal impact on opioid prescribing and, therefore, even less impact on the overall trajectory of the opioid crisis. While some estimates suggest that reductions in prescribing have averted many thousands of deaths,33 these changes may be more attributable to pain management guidelines and broader education efforts targeting prescribers.34,35,36 Indeed, prescribing guidelines issued by the CDC7 are similar to but predate state policies, and may explain why policies implemented later have had limited additional benefit. It is possible that although short-term policy impacts are limited, there may be long-term benefits of codifying guidelines consistent with those from the CDC into law, improving evidence-based opioid prescribing.
Concerns have been raised that prescribing limits may have adverse consequences offsetting their benefits, particularly for patients who are not the intended targets of the policy. By design, prescribing limits do not account for heterogeneity in the pain management needs of individual patients,37 and more-flexible guidelines accounting for patient circumstances and allowing for provider discretion may be needed. Qualitative studies with patients and providers have suggested that prescribing limits policies impose substantial requirements on prescribers that risk transforming pain management into an administrative task that reduces autonomy and interferes with shared clinician-patient decision making,38,39 complicating individualized pain management. While the trend in overall new prescriptions was not reduced, qualitative reports indicate that some individual prescribers may have reduced or discontinued prescribing opioids irrespective of individual patient needs in response to increasing complexity of opioid analgesic prescribing.40,41 The increased administrative burdens (e.g., requirements for regular review of pain management contracts), as well as concerns over enforcement by regulatory agencies, may disincentivize prescribers from using opioids to treat pain and result in undertreatment.42,43 For patients with inadequate pain management, many of whom report substantial difficulty obtaining needed medication,38,44 policy restrictions could contribute to transitions to more dangerous illicit opioids.43,45 Prescribing limitations may also prompt some prescribers to prematurely discontinue opioid treatment, which has been linked with catastrophic outcomes including suicide and overdose.46,47,48,49 Additional research is needed to better understand whether the modest benefits of laws that limit opioid prescribing outweigh the potential unintended consequences, including spillover effects for chronic pain patients and others who could benefit from treatment beyond legal limits. Data is lacking on the impact of prescribing policies on patient satisfaction and quality of life, appropriate prescriber application of policy provisions, practice changes due to administrative burdens and concerns over sanctions, and treatment delays or premature discontinuation. Future research might also examine the role of pharmaceutical manufacturers and others with financial interests in designing prescribing limits policies, given their prior influence on opioid-related policies50 and the possibility that support of prescribing limitations could limit their liability in future court filings. Opioid prescribing guidelines, including those issued by the CDC, have often been characterized as excessively rigid and misapplied.51 These concerns and recent evidence on safe and effective pain management have prompted the CDC to update its 2016 opioid prescribing guidelines, with less emphasis on defined prescriptions limits and more flexibility for clinicians and patients to determine the best course of treatment.52
Although well-designed prescribing policies may be important for combatting the opioid crisis, the evidence to date indicates they are largely insufficient. Additional research is needed to inform and refine policies in conjunction with comprehensive solutions that focus on treatment for OUD and harm reduction strategies with demonstrated effectiveness, such as increased access to medications and other evidence-based OUD treatments, naloxone distribution, and syringe exchange programs.43,53 Policies and interventions targeting upstream social determinants of addiction, such as stigma/discrimination and socioeconomic conditions, are likely also needed as part of a comprehensive approach.54
Limitations
Results from this study of NJ Medicaid enrollees may not generalize to populations with different or no insurance coverage, or to other state contexts and policies. Because diagnoses for acute and chronic pain often overlap, some individuals to whom the policy does not apply may have been included in analyses, which could reduce the magnitude of estimated policy effects. However, findings are consistent with studies of prescribing for acute pain associated with surgical procedures.21,37 Although interrupted time series is widely used in policy evaluations and sensitivity analyses including comparison medications showed similar results, additional confounding due to contemporaneous events or co-interventions cannot be entirely ruled out under this study design.
Conclusion
The New Jersey policy was associated with a reduction in initial prescriptions with >5 days’ supply, but not with an overall decline in new opioid prescriptions or in the rate at which initial prescriptions led to long-term use. The impacts of the policy on opioid prescribing, and consequently its downstream effects on the overall trajectory of the opioid crisis, are likely limited. With only modest benefits at best, future research is needed to build evidence regarding potential unintended consequences, including inadequate pain treatment and greater administrative burdens on providers and patients.
References
Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183-188. https://doi.org/10.1016/j.drugpo.2019.01.010
Minozzi S, Amato L, Davoli M. Development of dependence following treatment with opioid analgesics for pain relief: a systematic review. Addiction. 2013;108(4):688-698. https://doi.org/10.1111/j.1360-0443.2012.04005.x
Hadland SE, Bagley SM, Gai MJ, et al. Opioid use disorder and overdose among youth following an initial opioid prescription. Addiction. 2021;116(10):2790-2800. https://doi.org/10.1111/add.15487
Heins SE, Frey KP, Alexander GC, Castillo RC. Reducing high-dose opioid prescribing: state-level morphine equivalent daily dose policies, 2007–2017. Pain Med. 2019;21(2):308-316. https://doi.org/10.1093/pm/pnz038
Davis CS, Lieberman AJ. Laws limiting prescribing and dispensing of opioids in the United States, 1989-2019. Addiction. 2020;116(7):1817-1827. https://doi.org/10.1111/add.15359
Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349(20):1943-1953. https://doi.org/10.1056/NEJMra025411
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. https://doi.org/10.1001/jama.2016.1464
Tori ME, Larochelle MR, Naimi TS. Alcohol or benzodiazepine co-involvement with opioid overdose deaths in the United States, 1999-2017. JAMA Netw Open. 2020;3(4):e202361. https://doi.org/10.1001/jamanetworkopen.2020.2361
Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17(1):85-98. https://doi.org/10.1111/PME.12907
New Jersey Division of Consumer Affairs. Limitations on Prescribing, Administering, or Dispensing of Controlled Dangerous Substances, and Special Requirements for Management of Acute and Chronic Pain: Physicians, Podiatrists, Physician Assistants, and Certified Nurse Midwives. Published March 20, 2017. Accessed December 28, 2022. https://www.njconsumeraffairs.gov/Proposals/Pages/03202017-bme-proposal.aspx
New Jersey Substance Use Disorder Law. Chapter 28 P.L. 2017. Accessed December 28, 2022. https://nj.gov/treasury/pensions/documents/laws/chapter28-2017.pdf
Stein BD, Sheng F, Taylor EA, Dick AW, Sorbero M, Pacula RL. The effect of state policies on rates of high-risk prescribing of an initial opioid analgesic. Drug Alcohol Depend. 2022;231:109232. https://doi.org/10.1016/j.drugalcdep.2021.109232
Sacks DW, Hollingsworth A, Nguyen T, Simon K. Can policy affect initiation of addictive substance use? Evidence from opioid prescribing. J Health Econ. 2021;76:102397. https://doi.org/10.1016/j.jhealeco.2020.102397
Dave CV, Patorno E, Franklin JM, et al. Impact of state laws restricting opioid duration on characteristics of new opioid prescriptions. J Gen Intern Med. 2019;34(11):2339-2341. https://doi.org/10.1007/s11606-019-05150-z
Hincapie-Castillo JM, Goodin A, Possinger MC, Usmani SA, Vouri SM. Changes in opioid use after Florida’s restriction law for acute pain prescriptions. JAMA Netw Open. 2020;3(2):e200234. https://doi.org/10.1001/jamanetworkopen.2020.0234
Hincapie-Castillo JM, Easey T, Hernandez C, et al. Changes in quantity of opioids dispensed following Florida’s restriction law for acute pain prescriptions. Pain Med. 2021;22(8):1870-1876. https://doi.org/10.1093/pm/pnab017
Valdes IL, Possinger MC, Hincapie-Castillo JM, et al. Changes in prescribing by provider type following a state prescription opioid restriction law. J Gen Intern Med. 2021;37(8):1838-1844. https://doi.org/10.1007/s11606-021-06966-4
Reid DBC, Shah KN, Ruddell JH, et al. Effect of narcotic prescription limiting legislation on opioid utilization following lumbar spine surgery. Spine J. 2019;19(4):717-725. https://doi.org/10.1016/j.spinee.2018.09.007
Davis CS, Piper BJ, Gertner AK, Rotter JS. Opioid prescribing laws are not associated with short-term declines in prescription opioid distribution. Pain Med. 2020;21(3):532-537. https://doi.org/10.1093/pm/pnz159
McGinty EE, Bicket MC, Seewald NJ, et al. Effects of state opioid prescribing laws on use of opioid and other pain treatments among commercially insured U.S. adults. Ann Intern Med. 2022;175(5):617-627. https://doi.org/10.7326/M21-4363
Agarwal S, Bryan JD, Hu HM, et al. Association of state opioid duration limits with postoperative opioid prescribing. JAMA Netw Open. 2019;2(12):e1918361. https://doi.org/10.1001/jamanetworkopen.2019.18361
First Databank. FDB MedKnowledge. Published 2022. Accessed December 28, 2022. https://www.fdbhealth.com/solutions/medknowledge-drug-database
Unite Sates Census Bureau. X-13ARIMA-SEATS Seasonal Adjustment Program. Published July 11, 2022. Accessed December 28, 2022. https://www.census.gov/data/software/x13as.html
Sax C. Seasonal: R interface to X-13-ARIMA-SEATS. Published online August 6, 2016. Accessed June 3, 2022. https://cran.microsoft.com/snapshot/2016-10-23/web/packages/seasonal/vignettes/seas.pdf
Box GEP, Jenkins GM, Reinsel GC, Ljung GM. Time Series Analysis: Forecasting and Control. John Wiley & Sons; 2015.
Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082-2093. https://doi.org/10.1093/ije/dyy135
Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231-1238. https://doi.org/10.1111/j.1365-2753.2010.01504.x
Ranapurwala SI, Ringwalt CL, Pence BW, et al. State Medical Board policy and opioid prescribing: a controlled interrupted time series. Am J Prev Med. 2021;60(3):343-351. https://doi.org/10.1016/j.amepre.2020.09.015
Shackelton RJ, Marceau LD, Link CL, McKinlay JB. The intended and unintended consequences of clinical guidelines. J Eval Clin Pract. 2009;15(6):1035-1042. https://doi.org/10.1111/j.1365-2753.2009.01201.x
Alalouf M, Miller S, Wherry LR. What Difference Does a Diagnosis Make? Evidence from Marginal Patients. Published online October 2019. https://doi.org/10.3386/w26363
Almond D, Doyle JJ Jr, Kowalski AE, Williams H. Estimating marginal returns to medical care: evidence from at-risk newborns*. Q J Econ. 2010;125(2):591-634. https://doi.org/10.1162/qjec.2010.125.2.591
Fisher ES, Welch HG. Avoiding the unintended consequences of growth in medical care: how might more be worse? JAMA. 1999;281(5):446-453. https://doi.org/10.1001/jama.281.5.446
Alexander GC, Ballreich J, Mansour O, Dowdy DW. Effect of reductions in opioid prescribing on opioid use disorder and fatal overdose in the United States: a dynamic Markov model. Addiction. 2021;117(4):969-976. https://doi.org/10.1111/ADD.15698
Weiner SG, Baker O, Poon SJ, et al. The effect of opioid prescribing guidelines on prescriptions by emergency physicians in Ohio. Ann Emerg Med. 2017;70(6):799-808.e1. https://doi.org/10.1016/j.annemergmed.2017.03.057
Sullivan MD, Bauer AM, Fulton-Kehoe D, et al. Trends in opioid dosing among Washington state Medicaid patients before and after opioid dosing guideline implementation. J Pain. 2016;17(5):561-568. https://doi.org/10.1016/j.jpain.2015.12.018
Bohnert ASB, Guy GP, Losby JL. Opioid prescribing in the United States before and after the centers for disease control and prevention’s 2016 opioid guideline. Ann Intern Med. 2018;169(6):367-375. https://doi.org/10.7326/M18-1243
Chua KP, Brummett CM, Waljee JF. Opioid prescribing limits for acute pain: potential problems with design and implementation. JAMA. 2019;321(7):643-644. https://doi.org/10.1001/jama.2019.0010
Antoniou T, Ala-Leppilampi K, Shearer D, Parsons JA, Tadrous M, Gomes T. “Like being put on an ice floe and shoved away”: a qualitative study of the impacts of opioid-related policy changes on people who take opioids. Int J Drug Policy. 2019;66:15-22. https://doi.org/10.1016/j.drugpo.2019.01.015
Achkar MA, Revere D, Dennis B, MacKie P, Gupta S, Grannis S. Exploring perceptions and experiences of patients who have chronic pain as state prescription opioid policies change: a qualitative study in Indiana. BMJ Open. 2017;7(11):e015083. https://doi.org/10.1136/bmjopen-2016-015083
Walker DM, Childerhose JE, Chen S, et al. Exploring perspectives on changing opioid prescribing practices: a qualitative study of community stakeholders in the HEALing Communities Study. Drug Alcohol Depend. 2022;233:109342. https://doi.org/10.1016/j.drugalcdep.2022.109342
Hurstak EE, Kushel M, Chang J, et al. The risks of opioid treatment: perspectives of primary care practitioners and patients from safety-net clinics. Subst Abuse. 2017;38(2):213-221. https://doi.org/10.1080/08897077.2017.1296524
Bateman BT, Choudhry NK. Limiting the duration of opioid prescriptions: balancing excessive prescribing and the effective treatment of pain. JAMA Intern Med. 2016;176(5):583-584. https://doi.org/10.1001/jamainternmed.2016.0544
Pitt AL, Humphreys K, Brandeau ML. Modeling health benefits and harms of public policy responses to the US opioid epidemic. Am J Public Health. 2018;108(10):1394-1400. https://doi.org/10.2105/AJPH.2018.304590
Dassieu L, Heino A, Develay É, et al. “They think you’re trying to get the drug”: qualitative investigation of chronic pain patients’ health care experiences during the opioid overdose epidemic in Canada. Can J Pain. 2021;5(1):66-80. https://doi.org/10.1080/24740527.2021.1881886
Alpert A, Powell D, Pacula RL. Supply-side drug policy in the presence of substitutes: evidence from the introduction of abuse-deterrent opioids. Am Econ J Econ Policy. 2018;10(4):1-35. https://doi.org/10.1257/pol.20170082
Hallvik SE, El Ibrahimi S, Johnston K, et al. Patient outcomes after opioid dose reduction among patients with chronic opioid therapy. Pain. 2022;163(1):83-90. https://doi.org/10.1097/j.pain.0000000000002298
Agnoli A, Xing G, Tancredi DJ, Magnan E, Jerant A, Fenton JJ. Association of dose tapering with overdose or mental health crisis among patients prescribed long-term opioids. JAMA. 2021;326(5):411-419. https://doi.org/10.1001/jama.2021.11013
James JR, Scott JAM, Klein JW, et al. Mortality after discontinuation of primary care–based chronic opioid therapy for pain: a retrospective cohort study. J Gen Intern Med. 2019;34(12):2749-2755. https://doi.org/10.1007/S11606-019-05301-2/FIGURES/1
Oliva EM, Bowe T, Manhapra A, et al. Associations between stopping prescriptions for opioids, length of opioid treatment, and overdose or suicide deaths in US veterans: observational evaluation. The BMJ. 2020;368. https://doi.org/10.1136/bmj.m283
Marks JH. Lessons from corporate influence in the opioid epidemic: toward a norm of separation. J Bioethical Inq. 2020;17(2):173-189. https://doi.org/10.1007/s11673-020-09982-x
Rubin R. Limits on opioid prescribing leave patients with chronic pain vulnerable. JAMA. 2019;321(21):2059-2062. https://doi.org/10.1001/jama.2019.5188
Centers for Disease Control and Prevention. Proposed 2022 CDC Clinical Practice Guideline for Prescribing Opioids. Published online February 10, 2022. Accessed June 3, 2022. https://www.federalregister.gov/documents/2022/02/10/2022-02802/proposed-2022-cdc-clinical-practice-guideline-for-prescribing-opioids
Samples H. Commentary on Lo-Ciganic et al.: The importance of evidence-based clinical and policy approaches to reduce opioid harms. Addiction. Published online May 11, 2022. https://doi.org/10.1111/add.15915
Blanco C, Wall MM, Olfson M. Expanding current approaches to solve the opioid crisis. JAMA Psychiatry. 2022;79(1):5. https://doi.org/10.1001/jamapsychiatry.2021.3136
Funding
This work was supported by the National Institute on Drug Abuse (grants 1R01 DA047347-01 & K01 DA049950); NIH’s National Center for Advancing Translational Sciences (grant UL1TR003017); and the New Jersey Health Foundation. We acknowledge the New Jersey Department of Human Services for providing access to data and for their review of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Samples received consulting fees from the American Society of Addiction Medicine outside the submitted work. The remaining authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 6.33 mb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Treitler, P., Samples, H., Hermida, R. et al. Association of a State Prescribing Limits Policy with Opioid Prescribing and Long-term Use: an Interrupted Time Series Analysis. J GEN INTERN MED 38, 1862–1870 (2023). https://doi.org/10.1007/s11606-022-07991-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07991-7