Abstract
Background
Older smokers account for the greatest tobacco-related morbidity and mortality in the USA, while quitting smoking remains the single most effective preventive health intervention for reducing the risk of smoking-related illness. Yet, knowledge about patterns of smoking and smoking cessation in older adults is lacking.
Objective
Assess trends in prevalence of cigarette smoking between 1998 and 2018 and identify patterns and predictors of smoking cessation in US older adults.
Design
Retrospective cohort study
Participants
Individuals aged 55+ enrolled in the nationally representative Health and Retirement Study, 1998–2018
Main Measures
Current smoking was assessed with the question: “Do you smoke cigarettes now?” Quitting smoking was defined as having at least two consecutive waves (between 2 and 4 years) in which participants who were current smokers in 1998 reported they were not currently smoking in subsequent waves.
Key Results
Age-adjusted smoking prevalence decreased from 15.9% in 1998 (95% confidence interval (CI) 15.2, 16.7) to 11.2% in 2018 (95% CI 10.4, 12.1). Among 2187 current smokers in 1998 (mean age 64, 56% female), 56% of those living to age 90 had a sustained period of smoking cessation. Smoking less than 10 cigarettes/day was strongly associated with an increased likelihood of quitting smoking (subdistribution hazard ratio 2.3; 95% CI 1.9, 2.8), compared to those who smoked more than 20 cigarettes/day.
Conclusions
Smoking prevalence among older persons has declined and substantial numbers of older smokers succeed in quitting smoking for a sustained period. These findings highlight the need for continued aggressive efforts at tobacco cessation among older persons.
Similar content being viewed by others
INTRODUCTION
In the USA, older smokers account for the greatest tobacco-related morbidity and mortality.1,2 Cigarette smoking contributes to many of the major causes of death in older adults—including cardiac disease, cancer, cerebrovascular disease, and dementia—and over 70% of all smoking-related deaths occur in smokers over the age of 60.2,3,4,5,6 Quitting smoking, as it is in younger smokers, remains the single most effective preventive health intervention for reducing the risk of mortality and morbidity from smoking-related illness.7,8 Older adults experience immediate benefits from quitting, including decreased heart rate and blood pressure and improved lung function.1 When compared to those who continue to smoke, older adults who quit after age 65 may increase their life span by an average of 3 years and decrease years lived with disability.9,10
Despite the clear harms of smoking and numerous benefits of quitting smoking in older adults, we know little about the extent to which the prevalence of smoking has changed in recent years or patterns of smoking cessation in older adults.11 While there is extensive literature on smoking and smoking cessation in younger adults,12,13,14 the few studies examining prevalence and patterns of smoking in older adults in the USA either are outdated, are limited to a single year of data, aggregate all older adults into a single category rather than stratify by age categories, and rarely present data on smoking in those over the age of 80.15,16,17,18 Accurate national estimates of trends over time in the prevalence of smoking in older adults in the USA, as well as data on patterns and predictors of quitting smoking in this population, are critical for informing clinical and policy interventions targeted toward reducing smoking in older adults. Thus, we conducted a study using data from the nationally representative Health and Retirement Study (HRS) to (1) assess time trends in the prevalence of smoking for all adults aged 55 and older stratified by age category between 1998 and 2018 and (2) assess patterns and predictors of smoking cessation in this population.
METHODS
Data Source, Design, Participants
The HRS is a nationally representative, population-based longitudinal cohort study of community-dwelling Americans age 50 and older, with supplemental oversamples of Black and Hispanic individuals. The HRS employs a steady-state design with replenishment cohorts of individuals aged 50–55 added every 6 years. Participants undergo detailed in-person or telephone surveys approximately every 2 years from cohort entry until death or dropout. Each wave includes over 22,000 participants, and response rates range from 70 to 82% for first interviews and 88 to 90% for follow-up interviews. Mortality is ascertained through reports from next of kin or through a search in the National Death Index and captures virtually all deaths.19 Participants are surveyed on a variety of domains including health status, health behaviors, disability, family structure, and income and assets.20
We used two separate study designs and cohorts to address our objectives: (1) to assess time trends in prevalence of smoking, we used a serial cross-sectional design of HRS waves 1998–2018. We included all HRS participants at each wave who were 55+ (n = 32,382) and had a valid response for current smoking (n = 32,351); (2) for analyses of patterns and predictors of smoking cessation, we created a longitudinal cohort of participants 55 and older who had a completed interview in 1998 (n = 18,256), were current smokers in 1998 (n = 2779), were self- (non-proxy) respondents (n = 2507), and had at least one follow-up interview (n = 2187). As there is no clear agreement in the literature of at what age someone becomes an “older smoker,” with some studies including adults in their 40s and 50s and others only adults 60 plus, we chose 55 as an age that represented a “middle ground” of various definitions and ensured that our sample for the prevalence analysis was representative across waves and did not vary with the replenishment cohorts.
Measures
Smoking and Quitting Smoking
Smoking is assessed in the HRS by asking participants if they smoke cigarettes now and how many cigarettes or packs participants smoke daily (not including cigars or pipes). For the time-trends prevalence analysis, we identified prevalent smoking if participants reported currently smoking in that wave.
For the longitudinal cohort analysis, we conceptualized quitting smoking as successfully living a substantial part of one’s life as a nonsmoker, which we operationalized as having at least two consecutive waves of reporting not smoking among participants who reported current smoking in 1998. We required two consecutive waves of non-smoking for two reasons: (1) since we could not be sure with only a single wave that the person had quit smoking the day before or 2 years prior to their interview, including two waves of responses allowed us to be sure that the participant had quit smoking for a meaningful amount of time; (2) requiring two consecutive waves of non-smoking excluded those who stopped smoking in the last 2 years of life due to terminal illness from being classified as sustained non-smokers, given potentially limited benefit of quitting during the terminal phase. Although we required two consecutive waves of quitting for our definition, we considered the onset of quitting as occurring at the first wave at which a person reported not smoking.
Predictors of Quitting Smoking
For the longitudinal cohort analysis, characteristics of current smokers in 1998 were examined as potential predictors for quitting. These characteristics fall under several broad categories of factors that have been associated with quitting smoking in previous studies.17,21,22,23 These include (1) demographic characteristics (gender, race and ethnicity, education level, marital status, median wealth; living alone; rural versus urban residence); (2) comorbidities (0–1/2/2+ comorbidities including history of cancer, chronic obstructive lung disease, coronary artery disease, stroke, hypertension, diabetes; significant pain); (3) functional impairment (difficulty managing finances, difficulty walking several blocks, 3 or more impairments in activities of daily living (ADL)); (4) depressive symptoms (score of 3 or higher on the 8-item Center for Epidemiological Studies Depression Scale (CES-D)24); (5) cognitive impairment (cognitively normal (12–27)/cognitive impairment not dementia (7–11)/dementia (0–6) based on the Crimmens et al. algorithm25); (6) alcohol use (none = no alcohol; low = up to 1 drink a day for women and up to 2 drinks per day for men; heavy = more than 4 drinks per day for women and 5 drinks per day for men based on the National Institute on Alcohol Abuse and Alcoholism to define alcohol use levels26); and (7) number of cigarettes/day (< 10/11–20/20+).
Statistical Analysis
Time Trends in Current Smoking Prevalence
Overall prevalence of current smoking for the entire cohort was estimated using an age-adjusted logistic regression model at each wave. We also estimated prevalence stratified by age group (55–64/65–74/75–84/85+) and by gender (male/female).
Patterns and Predictors of Smoking Cessation
First, we identified prevalent smokers in 1998 and then followed them to assess one of the four possible outcomes: (1) still alive and quit smoking; (2) died and quit smoking before death; (3) still alive and no report of quitting; and (4) died and no report of quitting before death. Second, we estimated and visualized cumulative incidence of smoking cessation as one ages using a Fine and Gray model to account for competing risk of death.27 Fine and Gray modeling is recommended over Kaplan-Meier survival modeling in the presence of competing risks such as mortality.28 We estimated the overall cumulative incidence as well as stratified cumulative incidence by number of cigarettes smoked at baseline. To assess associations between participant characteristics and smoking cessation, we used the Fine and Gray model to estimate both unadjusted and fully adjusted sub-distribution hazard ratios (sHR) for each participant characteristic. We also tested for interactions between age and patient characteristics that were statistically significant in adjusted models. Finally, we conducted a sensitivity analysis where we defined quitting as requiring only one wave of not smoking instead of two waves.
All analyses were adjusted for HRS’s complex survey design. Estimates are reported with 95% confidence intervals, and statistical significance was set at p < 0.05. All analyses were conducted in Stata 17 (StataCorp, LLC) and R.6.2 (R Project). The HRS Sciences Institutional Review Board at the University of Michigan approved the HRS data collection. This study was approved by the University of California, San Francisco, Committee on Human Research as exempt.
RESULTS
Trends in Current Smoking Prevalence 1998–2018
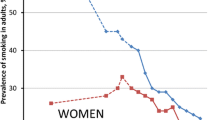
For any given wave between 1998 and 2018, the sample size for the prevalence analyses ranged from 14,347 to 16,932 (eTable 1). Age-adjusted prevalence of current smoking overall was 15.9% (95% CI 15.2, 16.7) in 1998, decreasing to 11.2% (95% CI 10.4–12.1) by 2018 (Fig. 1 and eTable 2). Differences were seen in the prevalence of smoking by age group and over time (Fig. 1 and eTable 2). The prevalence of smoking was markedly higher in younger age categories. In 1998, for example, the prevalence of current smoking was 22.8% (95% CI 21.7, 23.9) among participants 55–64, 14.99% (95% CI 13.7, 16.3) in participants aged 65–74, 7.79% (95% CI 7.05, 8.54) in participants aged 75–84, and 2.78% (95% CI 2.03, 3.53) in participants aged 85+. All age groups saw declines in the prevalence of current smoking over the observation period. Men had higher prevalence rates of smoking than women, although both groups saw declines over time (eFigure 1).
Patterns and Predictors of Smoking Cessation
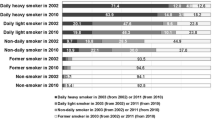
Of the 2187 current smokers in 1998 who met criteria for smoking cessation analyses, the mean age was 64.2 (standard deviation 7.4), 56.1% were female, 82.1% were non-Hispanic White, 10.3% non-Hispanic Black, 5.3% Hispanic, and 2.3% other (Table 1). By the end of the study period, 22.4% had quit and were still alive, 18.6% had quit before they died, 39.6% had died with no report of quitting before death, and 19.4% were alive and still smoking by the end of the follow-up period (Fig. 2 and eTable 3). The mean follow-up time was 9.3 years (standard deviation (SD) 5.5 years, range 1 to 8) for the entire cohort, 7 years (SD 4.6 years, range 3 to 18) for participants who quit, 9 years for participants who died (SD 4.8 years, range 1.5 to 19), and 16.8 years (SD 2.4 years, range 2.4 to 18) for those who did not quit and were censored in 2016.
The overall cumulative incidence of smoking cessation is shown in the pink line in Fig. 3. Accounting for the competing risk of death, 56.3% of older smokers quit smoking by the age of 90. Fewer number of cigarettes smoked per day was strongly associated with increased likelihood of smoking cessation (Fig. 3). Compared to participants who smoked more than 20 cigarettes per day, participants who smoked 10–19 cigarettes per day were 1.7 (95% CI 1.4, 2.2) more likely to quit smoking, while those who smoked fewer than 10 cigarettes per day were 2.3 (95% CI 1.9, 2.8) more likely to quit smoking. Depression, heavy drinking, and difficulty tracking finances were associated with lower likelihood of quitting smoking in adjusted models (Table 1). There was no interaction effect between age and any of the statistically significant predictors in our model. The cumulative incidence of smoking cessation was higher when only 1 wave of no smoking was used to define quitting (eFigure 2). Heavy drinking and numbers of cigarettes per day remained statistically significant for quitting, while depression was no longer significant in adjusted models (eTable 4).
DISCUSSION
In this study of the epidemiology of smoking in a nationally representative sample of US older adults, we observed a decrease in smoking prevalence in US older adults aged 55 and older from almost 16% in 1998 to 11% in 2018. We found that more than half of all older adults surviving to age 90 successfully quit smoking for at least 2 years. We confirm previous studies that have found a relationship between indicators of nicotine dependence (i.e., more cigarettes/day) and likelihood of quitting smoking. While these results provide a somewhat optimistic picture of declining smoking prevalence and successful smoking cessation in older adults, our results indicate there is still significant room to further reduce smoking in older adults through public health and clinical interventions.
Our findings extend the limited data available regarding trends in smoking prevalence in older adults and address a significant limitation of previous studies by providing detail on refined age categories of older adults over longer time periods. Our prevalence rates are similar to those found in the National Health Interview Survey (NHIS), a cross-sectional nationally representative survey often used for tobacco research. For example, data from 2016 NHIS showed the prevalence of smoking among adults 65–74 was 11.3% in 2016, compared to 11.0% in our study,29 while the 2015 prevalence among older adults 85 and older was 1.7% in NHIS compared to 1.8% (in 2016) in our sample.18 The lower prevalence of smoking in older age categories is likely explained by a combination of increased mortality among smokers, as well as successful smoking cessation with more opportunities to quit as one ages.
The 20-year time frame and large sample size in our study enable a clearer understanding of smoking prevalence trends over time and highlights that—although there were declines in smoking prevalence—these declines might be smaller than what one would expect. Previous studies with shorter study periods of 5–10 years have demonstrated variability in smoking prevalence in older adults, which may be due to “noise” over shorter time periods and smaller sample sizes in subgroups.29,30,31 Between the period when many participants in the 1998 cohort were children (i.e., the 1940s) to when the 2018 cohort were children (i.e., the 1960s), knowledge of the harms of smoking and government responses increased dramatically, most notably indicated by the 1964 Surgeon General’s first report on the harms of smoking. Given this fact, it is perhaps somewhat surprising that smoking prevalence rates only decreased about 5% in our study period.
To our knowledge, this is one of the first studies to examine incidence of smoking cessation among older adults. Our finding that over half of older smokers are able to successfully quit smoking by the oldest ages is somewhat surprising given previous findings that older smokers are less likely to report a cessation attempt than younger smokers32, but consistent with studies showing that older smokers who do attempt to quit are more likely to be successful.18,33 Furthermore, our findings show the importance of taking into account competing risk of death for these analyses. Our descriptive analyses demonstrate that a very high proportion of the cohort died and many did not quit before death. Taking into account competing risk of death allows for a more accurate assessment of smoking cessation incidence for people surviving to older ages compared to Kaplan-Meier and other survival regression techniques. Because the Kaplan-Meier model assumes those who are censored for whatever reason (including both death or loss to follow-up) have the same risk of the outcome as those in the remaining cohort, they artificially inflate incidence of outcomes (e.g., quitting smoking) in cohorts with high mortality rates.
Our findings are also consistent with previous literature that has found a strong association between lower nicotine dependence as indicated by fewer cigarettes smoked per day and increased likelihood of quitting smoking. 17,21,22,23 Lower nicotine dependence may indicate that a person has more negative beliefs about smoking and may already be trying to cut down on cigarette use, as well as having a lower physiological dependency on nicotine. Negative beliefs about smoking may result in a higher motivation to quit, which—when combined with being less physiologically addicted to nicotine—can facilitate successful quitting.34
There are several important implications for smoking-related public health and policy interventions generated from this study. Older smokers have received less attention from public health smoking cessation efforts than younger smokers and are frequently targeted by Big Tobacco marketing efforts.11 Older smokers are less likely to report that they have received advice from their health care provider to quit smoking and are less aware of Quitlines and other smoking cessation tools.32 Recent changes to Medicare billing that allow for smoking cessation counseling and treatments represent progress, but more efforts are needed to reduce smoking rates among older adults. Older smokers should be a target of public health efforts, and these efforts should be adapted to an older adult population that is extremely heterogenous in degree of educational attainment, cultural backgrounds, and functional capacity. For example, increasingly older adults are adept with technology and can be reached through online efforts, but barriers in access remain for some.35,36 Smoking cessation efforts targeted at older adults is an art and science that requires well-designed tobacco counter-marketing programs, ideally driven by professionals with experience in marketing research.37
Moreover, our findings could be used as a basis to explore potential marketing messages and clinical advice to older adults. For example, results showing high rates of quitting in older adults could be used to counter false beliefs common among older smokers that cessation attempts are unlikely to be successful after a lifetime of smoking and that “it is too late” to quit smoking.38,39,40,41 In addition, the fact that we found a strong relationship between lower nicotine dependence (fewer cigarettes per day) and successful quitting should be leveraged in older adults, who are more likely than younger adults to report smoking fewer cigarettes per day.18 Older smokers who have already reduced their cigarette consumption could be counseled that their lower cigarette consumption makes them more likely to be able to quit, and older smokers with higher nicotine dependency should be counseled that any attempt to cut back on cigarette consumption is beneficial and will help them quit in the long run. Focusing on older adults in the 55- to 75-year-old age range might have the biggest payoffs, since this group both has the highest prevalence of smoking and is also more likely to experience benefits of quitting smoking in terms of increased life expectancy.42 The relationship between smoking and depression is complex, but our finding showing a difference in the association between depressive symptoms and quitting for 1 wave compared to 2 waves supports the hypothesis that treating depression in older adults may also support sustained smoking cessation.43
This study has a number of limitations. First, we relied on self-report of quitting smoking and did not have laboratory verification of non-smoking status and individuals may not accurately report smoking behaviors.44 Second, characteristics of smokers for the smoking cessation analyses were only assessed in 1998 and were not time-varying. Finally, the smoking measures in the HRS are limited and do not include items about smoking beliefs, smoking behaviors (e.g., time from waking to first cigarette), or quitting methods tried, including pharmacological or non-pharmacological approaches.
In conclusion, with population aging, older smokers will make up a growing proportion of smokers in the USA. Older smokers suffer disproportionately from the impacts of smoking and continue to derive benefit from quitting smoking. Yet, older smokers have largely been ignored from public health tobacco cessation campaigns and are less likely to receive clinical advice to stop smoking. Our study found that despite declines in prevalence and high incidence of quitting among older adults, over 1 in 10 US older adults still smoke cigarettes. To reduce smoking among older smokers, public health efforts should target older smokers by tailoring their messages to the unique behavioral and physiological characteristics of older adults.
References
Office of the Surgeon General. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention (US); 2014.
Gellert C, Schöttker B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Int Med. 2012;172(11):837-844.
Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53-59.
Heron M. Deaths: leading causes for 2017. Natl Vital Stat Rep. 2019;68(6):1-77.
Cataldo JK, Malone RE. False promises: the tobacco industry, "low tar" cigarettes, and older smokers. J Am Geriatr Soc. 2008;56(9):1716-1723.
Anstey KJ, von Sanden C, Salim A, O'Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol. 2007;166(4):367-378.
Burns DM. Cigarette smoking among the elderly: disease consequences and the benefits of cessation. Am J Health Promot. 2000;14(6):357-361.
Nash SH, Liao LM, Harris TB, Freedman ND. Cigarette smoking and mortality in adults aged 70 years and older: results from the NIH-AARP cohort. Am J Prev Med. 2017;52(3):276-283.
Taylor DH, Jr., Hasselblad V, Henley SJ, Thun MJ, Sloan FA. Benefits of smoking cessation for longevity. Am J Public Health. 2002;92(6):990-996.
Østbye T, Taylor DH. The effect of smoking on years of healthy life (YHL) lost among middle-aged and older Americans. Health Serv Res. 2004;39(3):531-552.
Cataldo JK. Double whammy for older smokers: marginalized by tobacco control and valued by the tobacco industry. West J Nurs Res. 2019;41(8):1137-1151.
Fagan P, Augustson E, Backinger CL, et al. Quit attempts and intention to quit cigarette smoking among young adults in the United States. Am J Public Health. 2007;97(8):1412-1420.
Diemert LM, Bondy SJ, Brown KS, Manske S. Young adult smoking cessation: predictors of quit attempts and abstinence. Am J Public Health. 2013;103(3):449-453.
Siegel M, Mowery PD, Pechacek TP, et al. Trends in adult cigarette smoking in California compared with the rest of the United States, 1978-1994. Am J Public Health. 2000;90(3):372-379.
Husten CG, Shelton DM, Chrismon JH, Lin YC, Mowery P, Powell FA. Cigarette smoking and smoking cessation among older adults: United States, 1965-94. Tob Control. 1997;6(3):175-180.
Cohen-Mansfield J. Predictors of smoking cessation in old-old age. Nicotine Tob Res. 2016;18(7):1675-1679.
Salive ME, Cornoni-Huntley J, LaCroix AZ, Ostfeld AM, Wallace RB, Hennekens CH. Predictors of smoking cessation and relapse in older adults. Am J Public Health. 1992;82(9):1268-1271.
Henley SJ, Asman K, Momin B, et al. Smoking cessation behaviors among older U.S. adults. Prev Med Rep. 2019;16:100978.
Weir DR. Validating Mortality Ascertainment in the Health and Retirement Study. University of Michigan: Survey Research Center 2016.
Health and Retirement Study. Data Products: What's Available (Public): Cross-Wave Tracker File. http://hrsonline.isr.umich.edu/index.php?p=shoavail&iyear=ZS. Accessed 03/23/22.
U.S. Department of Health and Human Services. Smoking Cessation. A Report of the Surgeon General. In: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention NCfCDPaHP, Office on Smoking and Health, eds. Atlanta, GA 2020.
Augustson EM, Wanke KL, Rogers S, et al. Predictors of sustained smoking cessation: a prospective analysis of chronic smokers from the alpha-tocopherol Beta-carotene cancer prevention study. Am J Public Health. 2008;98(3):549-555.
Abdullah AS, Ho LM, Kwan YH, Cheung WL, McGhee SM, Chan WH. Promoting smoking cessation among the elderly: what are the predictors of intention to quit and successful quitting? J Aging Health. 2006;18(4):552-564.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):285-401.
Crimmins EM, Kim JK, Langa KM, Weir DR. Assessment of cognition using surveys and neuropsychological assessment: the health and retirement study and the aging, demographics, and memory study. J Gerontol Ser B, Psychol Sci Soc Sci. 2011;66 Suppl 1:i162-171.
National Institute on Alcohol Abuse and Alcoholism. Drinking Levels Defined. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed March 29, 2021, 2021.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509.
Austin PC, Lee DS, Fine JP. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation. 2016;133(6):601-609.
National Center for Health Statistics. Crude percentages of current cigarette smoking for adults aged 18 and over, United States, 2015-2018. National Health Interview Survey. Generated interactively: Wed Mar 31 2021.
National Center for Health Statistics. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2007. Vital Health Stat. 2007;10(240).
Isenberg JY, Quinones AR, Slatore CG, Bryson WC, Thielke SM. Trends in cigarette smoking and cessation among Medicare managed care recipients, 2005-2012. Addict Behav. 2016;58:155-160.
Jordan H, Hidajat M, Payne N, Adams J, White M, Ben-Shlomo Y. What are older smokers' attitudes to quitting and how are they managed in primary care? An analysis of the cross-sectional English Smoking Toolkit Study. BMJ Open. 2017;7(11):e018150.
Lee CW, Kahende J. Factors associated with successful smoking cessation in the United States, 2000. Am J Public Health. 2007;97(8):1503-1509.
Hyland A, Borland R, Li Q, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15 (Suppl 3):iii83-94.
Chen D, Wu LT. Smoking cessation interventions for adults aged 50 or older: A systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:14-24.
Hung LY, Lyons JG, Wu CH. Health information technology use among older adults in the United States, 2009-2018. Curr Med Res Opin. 2020;36(5):789-797.
Centers for Disease Control and Prevention. 2003. Designing and Implementing an Effective Tobacco Counter-Marketing Campaign. In: U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health, ed. Atlanta, Georgia.
Jarvis MJ, Wardle J, Waller J, Owen L. Prevalence of hardcore smoking in England, and associated attitudes and beliefs: cross sectional study. BMJ (Clinical research ed). 2003;326(7398):1061.
Kulak JA, LaValley S. Cigarette use and smoking beliefs among older Americans: findings from a nationally representative survey. J Addict Dis. 2018;37(1-2):46-54.
Kerr S, Watson H, Tolson D, Lough M, Brown M. Smoking after the age of 65 years: a qualitative exploration of older current and former smokers' views on smoking, stopping smoking, and smoking cessation resources and services. Health Soc Care Commun. 2006;14(6):572-582.
Cataldo JK. Clinical implications of smoking and aging: breaking through the barriers. J Gerontol Nurs. 2007;33(8):32-41.
Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-350.
Mathew AR, Hogarth L, Leventhal AM, Cook JW, Hitsman B. Cigarette smoking and depression comorbidity: systematic review and proposed theoretical model. Addiction. 2017;112(3):401-412.
Benowitz NL, Bernert JT, Foulds J, et al. Biochemical verification of tobacco use and abstinence: 2019 update. Nicotine Tob Res. 2020;22(7):1086-1097.
Funding
This study was supported by the National Institute on Aging (P30AG04428). Dr. Hunt is supported by the National Institute on Aging (K76AG074924).
Author information
Authors and Affiliations
Contributions
Study conception and design, all authors; analysis and interpretation of results, all authors; draft manuscript preparation, all authors. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 511 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hunt, L.J., Covinsky, K.E., Cenzer, I. et al. The Epidemiology of Smoking in Older Adults: A National Cohort Study. J GEN INTERN MED 38, 1697–1704 (2023). https://doi.org/10.1007/s11606-022-07980-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07980-w