Abstract
Background
While 60% of older adults have hearing loss (HL), the majority have never had their hearing tested.
Objective
We sought to estimate long-term clinical and economic effects of alternative adult hearing screening schedules in the USA.
Design
Model-based cost-effectiveness analysis simulating Current Detection (CD) and linkage of persons with HL to hearing healthcare, compared to alternative screening schedules varying by age at first screen (45 to 75 years) and screening frequency (every 1 or 5 years). Simulated persons experience yearly age- and sex-specific probabilities of acquiring HL, and subsequent hearing aid uptake (0.5–8%/year) and discontinuation (13–4%). Quality-adjusted life-years (QALYs) were estimated according to hearing level and treatment status. Costs from a health system perspective include screening ($30–120; 2020 USD), HL diagnosis ($300), and hearing aid devices ($3690 year 1, $910/subsequent year). Data sources were published estimates from NHANES and clinical trials of adult hearing screening.
Participants
Forty-year-old persons in US primary care across their lifetime.
Intervention
Alternative screening schedules that increase baseline probabilities of hearing aid uptake (base-case 1.62-fold; range 1.05–2.25-fold).
Main Measures
Lifetime undiscounted and discounted (3%/year) costs and QALYs and incremental cost-effectiveness ratios (ICERs).
Key Results
CD resulted in 1.20 average person-years of hearing aid use compared to 1.27–1.68 with the screening schedules. Lifetime total per-person undiscounted costs were $3300 for CD and ranged from $3630 for 5-yearly screening beginning at age 75 to $6490 for yearly screening beginning at age 45. In cost-effectiveness analysis, yearly screening beginning at ages 75, 65, and 55 years had ICERs of $39,100/QALY, $48,900/QALY, and $96,900/QALY, respectively. Results were most sensitive to variations in hearing aid utility benefit and screening effectiveness.
Limitation
Input uncertainty around screening effectiveness.
Conclusions
We project that yearly hearing screening beginning at age 55+ is cost-effective by US standards.
Similar content being viewed by others
INTRODUCTION
Most US adults will experience hearing loss (HL) at some point in their lifetime, with prevalence reaching 50% at age 70 years and 80% by 80.1,2,3 Despite this high prevalence, hearing screening is not commonly performed in adults, leaving most affected Americans without a diagnosis. As a result, 80% of persons with HL in the USA do not receive treatment.1,4 Furthermore, untreated HL is associated with significant impacts on quality of life, cognitive impairment and other morbidities, fall risk, and patient-provider communication.5,6,7,8,9,10 HL incurs yearly societal costs of upwards of $194B due to associated and independent risk of poor general health and dementia.7,9,11 Stakeholders are increasingly calling for identification of cost-effective interventions to diagnose, link, and treat persons with HL.12,13,14,15
Screening for HL in primary care settings increases diagnosis of HL and downstream treatment uptake.16,17,18 However, current US screening practices are varied and include single questions, surveys, and sound tests, with some professional societies recommending regular hearing screening of older adults.19,20 A recent United States Preventative Services Taskforce (USPSTF) update found that while several screening modalities successfully identify persons with HL, and that HL treatment is beneficial, there was insufficient evidence to make a recommendation on screening asymptomatic adults over age 50 years.21,22,23 A key limitation of the evidence cited by the USPSTF was the absence of a randomized trial that linked hearing screening to quality-of-life outcomes in the general population. In this study, we used a model to estimate the long-term clinical and economic effects of different adult hearing screening paradigms in the USA and identify key sources of uncertainty to guide future research and policy.
METHODS
Analytic Overview
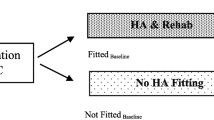
We used Decision model of the Burden of Hearing Loss Across the Lifespan (DeciBHAL-US) to simulate Current Detection (CD), e.g., current rates of symptomatic presentation and uptake of hearing healthcare, compared to different hearing screening schedules that varied by age at first screen and screening frequency.24 In previously published validation exercises, DeciBHAL accurately modeled observed HL natural history and treatment.24 We simulated a cohort of 40-year-old persons without HL throughout their remaining lifetime, with yearly probabilities of acquiring HL and subsequent hearing aid (HA) uptake and discontinuation. Screening effectiveness was simulated as an increase in baseline HA uptake. We measured undiscounted and discounted (3%/year) effectiveness, using quality-adjusted life-years (QALYs), and estimated health system costs (2020 USD). We considered incremental cost-effectiveness ratios (ICERs) of <$100,000/QALY to be cost-effective.25,26 This study followed the Second Panel on Cost-Effectiveness in Health and Medicine and Consolidated Health Economic Reporting Standards.27,28
Model Overview
DeciBHAL-US is a microsimulation model of HL natural history, detection, diagnosis, and treatment (see Appendix 1 for health state diagrams, and the published validation for further details).24 Simulated persons experience yearly age- and sex-specific probabilities of acquiring bilateral sensorineural HL, conductive HL, or both, based on published National Health and Nutrition Examination Survey (NHANES) estimates.1 Persons with sensorineural HL experience age-related decline in pure tone average (PTA) hearing level (Table 1).15 After acquiring HL, patients experience age- and severity-specific yearly probabilities of acquiring HAs and, once using HAs, rates of discontinuation. Adults with severe-to-profound HL may receive cochlear implantation after use of HAs for at least 1 year.29
Simulated Screening Schedules
We simulated screening schedules starting at ages 45, 55, 65, and 75 years and lasting throughout the lifetime with frequencies of screening every 1 and 5 years. We simulated a sound test screening modality, however, to account for imperfect implementation, incorporating a lower specificity to capture costs from falsely positive tests acquiring audiological services (described below).21
Model Input Data
Natural History of Hearing Loss
Yearly probabilities of bilateral sensorineural HL ranged from 0.8 to 10.4% for males and 0.1 to 9.2% for females.1,30,31,32,33 Age-specific decline in HL is modeled as a yearly decibel (dB) increase in PTA (mean=1.05dB/year; SD=0.4) that was derived from a longitudinal study of older adults and validated to the Baltimore Longitudinal Study on Aging.34,35 Simulated persons may also acquire conductive HL.36,37,38,39,40,41,42
Hearing Aid Uptake
Simulated persons with HL experience yearly probabilities of HA acquisition that vary with age and severity (Table 1).4,43 After acquiring HAs, simulated persons have yearly probabilities of discontinuation that range from 13% in year 1 after acquisition and decline to 4% in year 10.44,45 These combined inputs were previously calibrated to NHANES estimates of HA use prevalence.4 DeciBHAL-US projects average person-time of HA use by aggregating each year a simulated person uses a HA and dividing by the total cohort size.
Cochlear Implant Uptake
Patients with severe or profound HL experienced a 1.3% annual probability of cochlear implantation after at least 1 year of HA use, and a 1% probability of CI discontinuation thereafter.46,47
Screening Effectiveness
We simulated the effectiveness of HL screening schedules as a multiplier on calibrated baseline rates of HA uptake among simulated persons with HL. We based this multiplier on one randomized control trial and one non-randomized before-and-after study that demonstrated increased rates of hearing healthcare uptake after screening implementation that ranged from 1.50 to 2.0 (using a tone-emitting otoscope or four-frequency screening device).18,48 For our base-case screening effectiveness parameter (1.62), we combined the risk ratios of hearing healthcare uptake after screening versus no screening using inverse variance weighting. We assumed that among persons who had screen-suggested HL, there would be a similar risk ratio for HA uptake in veterans and non-veterans (though the absolute rate is different). We also assumed that the risk ratio for increased hearing healthcare uptake was equivalent to the risk ratio of HA uptake in one study that measured only hearing healthcare uptake. Given this uncertainty, we varied screening effectiveness in sensitivity analysis from 1.05 to 2.25.
Screening Test Characteristics
While we simulated a sound testing screening strategy, we incorporated test characteristics from other screening test modalities to capture imperfect implementation. To estimate the number of persons without HL who might be referred for a hearing diagnostic test based on results of hearing screening, we used a false positive probability of 24% (1-specificity, 74%), based on pooled estimates of the Hearing Handicap Inventory for the Elderly from the USPSTF Evidence Review.21 We similarly incorporated a pooled sensitivity of 80%. These screening test characteristics affected model-projected costs, but not screening effectiveness because test characteristics were already incorporated in downstream HA uptake estimates.
Health State Utilities
We assumed a population average utility of 0.84 for persons without HL, and mild and moderate HL utility values derived from the published literature of 0.71 and 0.65.49,50,51 We incorporated data from a recent systematic review on the utility benefits of HAs (+0.11) and cochlear implants (+0.17) and vary these in sensitivity analysis (Appendix 2).50,51,52,53
Screening Costs
Screening test costs were applied to persons without and with HL (schedule-dependent, either yearly or every 5 years). For persons without HL, we included the cost of a screening test ($2; device cost and personnel time amortized across all persons screened) and the proportion of persons receiving a false positive test (24%) who would seek an audiology diagnostic test (43%; $295), coming to a net cost of $33.18,21,54,55 For persons with HL but without hearing treatment, we included the proportion of persons that receive a true positive screen (80%) and seek an audiology diagnostic test but do not acquire HAs (51%). Along with the screening test cost ($2), the total was $120.18,54,55
Hearing Healthcare Costs
We included costs of an audiology diagnostic test ($295), HA one-time purchase ($3690 for the device) and recurring operational and replacement costs ($910), and costs of cochlear implantation ($54,380 one-time, $1260–1400 yearly recurring).12,55,56,57,58,59,60 For HAs, we assumed 84% of fittings were binaural and accounted for the proportion of reduced cost HA fittings done through the US Department of Veteran’s Affairs.12 Recurring HA costs included batteries and replacement of the HA device every 5 years.59,61 In sensitivity analyses, we considered lower HA device costs that may be seen with over-the-counter HAs.
Sensitivity Analysis
We performed a one-way sensitivity analysis, varying model parameters across their plausible ranges. We selected parameters with the most underlying uncertainty. We then varied multiple parameters simultaneously across their plausible ranges. We included a sensitivity analysis incorporating World Health Organization (WHO) assumptions (HL treatment improves utility by 1 severity stratum) for HA utility benefits. We additionally performed probabilistic uncertainty analysis (PUA), assigning distributions to the most influential parameters identified in deterministic analysis and assessing the impact of their joint uncertainties on our cost-effectiveness outcomes (Appendix 3).62,63
Budget Impact Analysis
We projected 5-year undiscounted incremental costs of a screening schedule for the current US adult population compared to CD, simulating 59 cohorts of persons (ages 40–99), scaled to the US population, over 5 years to estimate 5-year costs for each schedule (Appendix 4).
RESULTS
Clinical Results
HA use increased with earlier age of onset of screening and increased frequency of screening, ranging from 1.20 average person-years under CD to 1.68 for yearly screening starting at age 45 years. Mean age at first HA with CD was 79.2 years, whereas yearly screening schedules initiated before age 75 reduced this age by 0.2 to 0.8 years depending on the age at first screen. Per-person lifetime undiscounted QALYs for CD were 32.107 (Table 2). Compared to CD, 5-yearly schedules increased undiscounted lifetime QALYs by 0.01–0.02, and yearly screening schedules imparted increases of 0.04–0.07 QALYs.
Costs and Cost-Effectiveness
CD had lifetime undiscounted per-person hearing healthcare costs of $3300, 5-yearly screening schedules had per-person costs of $3630–3960 (varying with age at first screen, 45–75 years), and yearly schedules $4780–6490. Using discounted costs and QALYs, annual screening beginning at ages 75, 65, and 55 years were all considered cost-effective, with ICERs of $39,100/QALY, $48,900/QALY, and $96,900/QALY, respectively. Annual screening beginning at age 45 years had an ICER of $234,600/QALY. Compared to annual screening strategies, 5-year screening strategies beginning at 65, 55, and 45 were eliminated by weak (or extended) dominance because they were less effective and less efficient (i.e., had a higher ICER) than yearly screening beginning at age 75 (Appendix 5).
One-Way Sensitivity Analysis
The ICER for yearly screening beginning at age 55 years was most sensitive to single parameter variations in audiology diagnostic test cost, screening effectiveness, HA device cost, screening test false positive probability, and HA utility benefit (Fig. 1). Varying these parameters across their plausible ranges, the yearly screening schedule beginning at age 55 exceeded the $100,000/QALY threshold (Fig. 1, dashed line).
One-way sensitivity analysis on the cost-effectiveness of yearly screening beginning at age 55 years. This is a tornado diagram illustrating the effects of variation of single parameters (row) across their plausible range on the incremental cost-effectiveness ratio (ICER) of yearly screening beginning at age 55. The y-axis crosses the x-axis at the base-case ICER of $96,900/QALY. Each sensitivity analysis is presented with a base-case value, range explored, and the resulting ICERs from that range are plotted. The long-dashed line represents the US willingness-to-pay threshold of $100,000/QALY, and the short-dashed line indicates an ICER of $50,000/QALY.
Multi-way Sensitivity Analysis
With base-case HA utility benefit inputs, yearly screening beginning at age 55 years remained under $100,000/QALY as long as effectiveness was >1.55 and device cost was <$6580 (cut points; Fig. 2A). With screening effectiveness ranging between 1.25 and 1.45, yearly screening beginning at age 65 years was <$100,000/QALY. When screening effectiveness was lowered to 1.05–1.15, none of the simulated screening schedules was cost-effective.
Three-way sensitivity analysis on the cost-effectiveness of adult hearing screening schedules in the USA. This figure shows the impact of varying hearing screening effectiveness, hearing aid device cost, and hearing aid utility benefit on the incremental cost-effectiveness ratios (ICERs) of screening schedules. Screening effectiveness was varied from 1.05 to 2.25 on the x-axis, and hearing aid device cost was varied from $800 to 6580 on the y-axis. Panel A shows the base-case hearing aid utility benefit of +0.11 and panel B shows the results assuming a hearing aid utility benefit of +0.01–0.07 (varying with severity, similar to that assumed by the WHO and the Global Burden of Disease). Each combination of parameters yields an ICER that is color-coded, with red indicating that all screening schedules had ICERs >$100,000/QALY, orange that only yearly screening at age 75 was below $100,000/QALY, yellow that yearly screening at age 65 was below $100,000/QALY, green that yearly screening at age 55 was between $50 and 100,000/QALY, and blue that yearly screening at age 55 was less than $50,000/QALY. The X marks the base-case input combination of screening effectiveness and hearing aid device cost.
Lowering the HA utility benefit to match assumptions used by the WHO15 and Global Burden of Disease64 increased the base-case ICER of yearly screening at age 55 to $169,700/QALY (Fig. 2B). With these utility benefit assumptions, yearly screening at age 75 years was cost-effective (ICER=$93,500/QALY).
Probabilistic Uncertainty Analysis
We simultaneously varied the utility benefit of HAs, screening effectiveness and false positive probability, audiology diagnostic test cost, and HA device cost across defined distributions (Appendix 6). At base-case WTP of $100,000/QALY, there was large uncertainty around the optimal screening schedule (most effective non-dominated schedule with an ICER under the WTP), with no single schedule representing the optimal schedule in ≥ 50% of simulations.
Budget Impact Analysis
The average annual undiscounted cost of CD over 5 years and for the US population over age 40 years was $12.8B, and for yearly screening beginning at age 55 it was $21.8B (Fig. 3; Appendix 7).
Budget impact analysis. This figure depicts the model-projected average annual outlays over the first 5 years of the Current Detection and yearly screening beginning at age 55 years (55q1). The height of the bars represents the total annual cost of CD and the 55q1 screening schedule, with 2020 USD on the y-axis. The components of the total cost are chronic suppurative otitis media (CSOM) treatment (blue), hearing aid (HA) uptake (gray), hearing aid maintenance (yellow), cochlear implant (CI) costs, and screening costs (orange).
DISCUSSION
Our model predicts that hearing screening schedules for US adults would increase uptake of hearing healthcare and improve quality of life. Yearly screening at ages 55+years increased per-person undiscounted lifetime QALYs by 0.07, equivalent to extending full-health survival by 26 days (averaged across all persons without and with HL). Compared to CD, per-person lifetime undiscounted costs increased by ~$2,900, and the ICER was $96,900/QALY for yearly screening beginning at age 55. Simulated screening schedules beginning later in life, such as 65 and 75 years when HL is more prevalent, were even more cost-effective (ICERs<$50,000/QALY) and initiating screening at age 65 may be more clinically feasible than at age 55 given the onset of Medicare coverage.
In sensitivity analysis, applying less optimistic parameter values resulted in the ICER of yearly screening beginning at 55 years to exceed $100,000/QALY, while screening at older ages remained cost-effective. To improve the cost-effectiveness of screening, policymakers could focus on improving referral processes to hearing healthcare after screening (effectiveness) and lowering patient’s costs for audiology diagnosis or purchase of HA devices. There was large uncertainty around the optimal hearing screening strategy in PUA and future efforts should focus on quantifying the value of reduction in parameter uncertainty ascertained by potential research projects through value of information analysis.65 In particular, clinical studies clarifying the impact of hearing screening on HA uptake would likely reduce this decision uncertainty.
Previous model-based cost-effectiveness analyses of adult hearing screening schedules in high-income settings have supported the economic efficiency of screening beginning at ages 55–65 years.54,66,67,68 One study set in the USA, based on a randomized controlled trial of ≥ 50-year-old, primarily male veterans, projected a $1400 cost per additional HA user at 1 year.54 Our results are not directly comparable to this study because we projected costs/QALY and over a lifetime. Two European studies projected ICERs of €3700/QALY ($4700 in 2020 USD) and £1800/QALY ($2800 in 2020 USD) for 5-yearly screening in the Netherlands and the UK.66,67 These ICERs are lower than our estimates, likely due to our incorporation of audiometric evaluation costs for false positives, consideration of HA discontinuation, and the higher costs of HAs and healthcare in the USA.
A major consideration around adult hearing screening is successful implementation in real-world settings.69,70 Challenges throughout the implementation process include appropriate distribution of the hearing screening test, referral to a hearing professional, and linkage to hearing healthcare. Our sensitivity analyses varying screening effectiveness might approximate reductions in effect due to imperfect implementation. Innovative hearing screening strategies could expand access and help to alleviate the burden on primary care settings.71,72
We simulated a sound testing–based screening modality as objective assessment measures, such as tone-emitting otoscopes or four-frequency screening devices, have shown better results in trials of adult hearing screening. However, single-question or other clinical hearing screening tests may be more feasible in a clinic setting.18,54 To be conservative and account for imperfect implementation, we incorporated a higher false positive probability (associated with a survey). However, novel mobile app–based point of care hearing screening modalities would likely reduce false positives and lower overall test costs.73
Affordability of HAs after a positive screen and diagnosis of HL remains a large barrier to increased adoption of HAs.16 HAs are not covered under Medicare and receive limited coverage by other insurers, so persons with HL bear the majority of the several thousand-dollar cost of HAs. We project Medicare coverage of HAs for adults over age 65 years to be very cost-effective (ICER<$50,000/QALY) and would help with affordability issues. Another potential mitigation of this problem is the Over-the-Counter Hearing Aid Act, which allows persons with perceived mild-to-moderate HL to purchase FDA-regulated over-the-counter HA devices without a medical exam or fitting by a specialist.74 While the introduction of this new category of FDA-regulated hearing devices is projected to increase access and lower HA device cost, its overall impacts on the costs and effectiveness of hearing screening are less well understood. Our sensitivity analysis demonstrated that if over-the-counter HAs increase HA uptake at lower cost, hearing screening becomes even more cost-effective.
Our analysis has several limitations. First, we made simplifying assumptions in our model structure and input data; however, we documented these assumptions and tested them in sensitivity analysis. Second, we assumed that the risk ratio of HA uptake due to screening (hearing screening effectiveness) remained constant throughout the lifetime. The true impact of repeated screening on persons with HL and at different ages is unknown; therefore, we varied screening effectiveness extensively in sensitivity analysis. Third, we excluded possible benefits to screening beyond provision of technology, including acknowledgement of a suspected health issue and treatment approaches not based on use of HAs.75 Additionally, there may be benefits to passing a hearing screen, such as peace of mind, that we did not consider. Fourth, we conservatively excluded potential benefits of hearing healthcare on physical and cognitive health and healthcare costs. To the extent that early detection and treatment of HL improves physical and cognitive health, the benefits of hearing screening would be larger than our current estimates. Lastly, due to data limitations we did not include indirect societal costs such as improved workforce participation due to HL and its treatment. Assuming that early treatment of HL improves workforce participation, the cost-effectiveness of hearing screening would improve.76
To conclude, we project annual hearing screening in US adults beginning at age 55 to be cost-effective. In addition, our analysis supports that annual screening beginning at ages 65 and 75 is even more cost-effective and should likely be performed. While future research might inform more certain parameters such as screening effectiveness, our findings were robust over a wide range of assumptions of screening effectiveness. Delaying hearing screening implementation in the hopes of perfect evidence will only further increase the wide hearing healthcare diagnosis and treatment gap and perpetuate long-standing inequities in hearing healthcare. The inclusion of hearing in health assessments of older adults is imperative to their health and well-being, and we demonstrate here that it too is likely a good use of resources.
References
Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health 2016;106(10):1820-2.
Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol Series A: Biomed Sci Med Sci 2011;66(5):582-90.
Bainbridge KE, Wallhagen MI. Hearing loss in an aging American population: extent, impact, and management. Annu Rev Public Health 2014;35:139-52.
Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med 2012;172(3):292-3.
Gopinath B, McMahon CM, Burlutsky G, Mitchell P. Hearing and vision impairment and the 5-year incidence of falls in older adults. Age Ageing 2016;45(3):409-14.
Kamil RJ, Betz J, Powers BB, Pratt S, Kritchevsky S, Ayonayon HN, et al. Association of hearing impairment with incident frailty and falls in older adults. J Aging Health 2016;28(4):644-60.
Lin FR, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med 2012;172(4):369-71.
Deal JA, Reed NS, Kravetz AD, Weinreich H, Yeh C, Lin FR, et al. Incident hearing loss and comorbidity: a longitudinal administrative claims study. JAMA Otolaryngol Head Neck Surg 2019;145(1):36-43.
Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol 2011;68(2):214-20.
Shukla A, Nieman CL, Price C, Harper M, Lin FR, Reed NS. Impact of hearing loss on patient-provider communication among hospitalized patients: a systematic review. Am J Med Qual 2019;34(3):284-92.
Huddle MG, Goman AM, Kernizan FC, Foley DM, Price C, Frick KD, et al. The economic impact of adult hearing loss: a systematic review. JAMA Otolaryngol–Head Neck Surg. 2017;143(10):1040-8.
National Academies of Sciences, Engineering, and Medicine. Hearing health care for adults: priorities for improving access and affordability. Washington, DC: The National Academies Press; 2016.
National Institute on Deafness and Other Communication Disorders (NIDCD). 2017-2021 NIDCD Strategic Plan. Accessed 17 February 2022 at https://www.nidcd.nih.gov/sites/default/files/Documents/NIDCD-StrategicPlan2017-508.pdf.
Wilson BS, Tucci DL, Merson MH, O’Donoghue GM. Global hearing health care: new findings and perspectives. Lancet 2017;390(10111):2503-15.
World Health Organization. World report on hearing. Geneva 2021. Accessed 17 February 2022 at https://www.who.int/publications/i/item/world-report-on-hearing.
Barnett M, Hixon B, Okwiri N, Irungu C, Ayugi J, Thompson R, et al. Factors involved in access and utilization of adult hearing healthcare: a systematic review. Laryngoscope 2017;127(5):1187-94.
Folmer RL, Saunders GH, Vachhani JJ, Margolis RH, Saly G, Yueh B, et al. Hearing health care utilization following automated hearing screening. J Am Acad Audiol 2021.
Zazove P, Plegue MA, McKee MM, DeJonckheere M, Kileny PR, Schleicher LS, et al. Effective hearing loss screening in primary care: the early auditory referral-primary care study. The Annals of Family Medicine 2020;18(6):520-7.
American Speech-Language-Hearing Association. Preferred practice patterns for the profession of audiology. Rockville, MD: ASHA National Office; 2006. Accessed 17 February 2022 at https://www.asha.org/policy/pp2006-00274/.
Yueh B, Shekelle P. Quality indicators for the care of hearing loss in vulnerable elders. J Am Geriatr Soc 2007;55:S335-9.
United States Preventative Services Task Force. Hearing Loss in Older Adults: Screening. 2020. Accessed 17 February 2022 at https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/hearing-loss-in-older-adults-screening.
Krist AH, Davidson KW, Mangione CM, Cabana M, Caughey AB, Davis EM, et al. Screening for hearing loss in older adults: US Preventive Services Task Force recommendation statement. JAMA 2021;325(12):1196-201.
Feltner C, Wallace IF, Kistler CE, Coker-Schwimmer M, Jonas DE. Screening for hearing loss in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2021;325(12):1202-15.
Borre ED, Myers ER, Dubno JR, O’Donoghue GM, Diab MM, Emmett SD, et al. Development and validation of DeciBHAL-US: a novel microsimulation model of hearing loss across the lifespan in the United States. EClinicalMedicine. 2022;44:101268.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med 2014;371(9):796-7.
Vanness DJ, Lomas J, Ahn H. A health opportunity cost threshold for cost-effectiveness analysis in the United States. Ann Intern Med 2021;174(1):25-32.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS)—explanation and elaboration: a report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health 2013;16(2):231-50.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA 2016;316(10):1093-103.
Centers for Medicare & Medicard Services. Cochlear Implantation. Accessed 17 February 2022 at https://www.cms.gov/Medicare/Coverage/Coverage-with-Evidence-Development/Cochlear-Implantation-.
Arias E, Xu JQ. United States life tables, 2018. National Vital Statistics Reports; vol 69, no 12. Hyattsville, MD: National Center for Health Statistics. 2020.
Homans NC, Metselaar RM, Dingemanse JG, van der Schroeff MP, Brocaar MP, Wieringa MH, et al. Prevalence of age-related hearing loss, including sex differences, in older adults in a large cohort study. Laryngoscope 2017;127(3):725-30.
Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: the epidemiology of hearing loss study. Am J Epidemiol 1998;148(9):879-86.
Van Naarden K, Decouflé P, Caldwell K. Prevalence and characteristics of children with serious hearing impairment in metropolitan Atlanta, 1991–1993. Pediatrics. 1999;103(3):570-5.
Lee F-S, Matthews LJ, Dubno JR, Mills JH. Longitudinal study of pure-tone thresholds in older persons. Ear Hear 2005;26(1):1-11.
Morrell CH, Gordon-Salant S, Pearson JD, Brant LJ, Fozard JL. Age-and gender-specific reference ranges for hearing level and longitudinal changes in hearing level. J Acoustical Soc Am 1996;100(4):1949-67.
Monasta L, Ronfani L, Marchetti F, Montico M, Brumatti LV, Bavcar A, et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS One 2012;7(4):e36226.
Rosenfeld RM, Kay D. Natural history of untreated otitis media. Laryngoscope 2003;113(10):1645-57.
Rosenfeld RM, Shin JJ, Schwartz SR, Coggins R, Gagnon L, Hackell JM, et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngology–Head Neck Surg. 2016; 154(1_suppl):S1-S41.
National Collaborating Centre for Women’s and Children’s Health Surgical management of otitis media with effusion in children. National Institute for Health and Clinical Excellence 2008. Accessed 13 July 2021 at https://www.nice.org.uk/guidance/cg60/documents/cg60-surgical-management-of-ome-full-guideline2.
Acuin, J. Chronic suppurative otitis media: burden of illness and management options. Geneva: World Health Organization, 2004.
Avnstorp MB, Homøe P, Bjerregaard P, Jensen RG. Chronic suppurative otitis media, middle ear pathology and corresponding hearing loss in a cohort of Greenlandic children. Int J Pediatr Otorhinolaryngol 2016;83:148-53.
Aarhus L, Tambs K, Kvestad E, Engdahl B. Childhood otitis media: a cohort study with 30-year follow-up of hearing (the HUNT study). Ear Hear 2015;36(3):302.
Simpson AN, Matthews LJ, Cassarly C, Dubno JR. Time from hearing aid candidacy to hearing aid adoption: a longitudinal cohort study. Ear Hear 2019;40(3):468-76.
Takahashi G, Martinez CD, Beamer S, Bridges J, Noffsinger D, Sugiura K, et al. Subjective measures of hearing aid benefit and satisfaction in the NIDCD/VA follow-up study. J Am Acad Audiol 2007;18(4):323-49.
Kochkin S, Beck DL, Christensen LA, Compton-Conley C, Fligor BJ, Kricos PB, et al. MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review 2010;17(4):12-34.
American Cochlear Implant Alliance. Cochlear Implants. Accessed 17 February 2022 at https://www.acialliance.org/page/CochlearImplant.
Raine CH, Summerfield Q, Strachan DR, Martin JM, Totten C. The cost and analysis of nonuse of cochlear implants. Otol Neurotol 2008;29(2):221-4.
Yueh B, Collins MP, Souza PE, Boyko EJ, Loovis CF, Heagerty PJ, et al. Long-term effectiveness of screening for hearing loss: the screening for auditory impairment--which hearing assessment test (SAI-WHAT) randomized trial. J Am Geriatr Soc 2010;58(3):427-34.
Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health 2015;3(11):e712-e23.
Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technol Assess 2007;11(42):1-294.
Kaur P, Chong SL, Kannapiran P, Teo W-SK, Ling CNW, Weichen CW, et al. Cost-utility analysis of hearing aid device for older adults in the community: a delayed start study. BMC Health Serv Res 2020;20(1):1-11.
Borre ED, Kaalund K, Frisco N, Zhang G, Ayer A, Kelly-Hedrick M, Reed SD, Emmett SD, Francis HW, Tucci DL, Wilson BW, Kosinski A, Ogbuoji O, Sanders Schmidler GD. The impact of hearing loss and its treatment on health-related quality of life utility: a systematic review and meta-analysis. Under Rev
Grutters JP, Joore MA, van der Horst F, Verschuure H, Dreschler WA, Anteunis LJ. Choosing between measures: comparison of EQ-5D, HUI2 and HUI3 in persons with hearing complaints. Qual Life Res 2007;16(8):1439-49.
Liu C-F, Collins MP, Souza PE, Yueh B. Long-term cost-effectiveness of screening strategies for hearing loss. J Rehabil Res Dev 2011;48(3).
Hojjat H, Svider PF, Davoodian P, Hong RS, Folbe AJ, Eloy JA, et al. To image or not to image? A cost-effectiveness analysis of MRI for patients with asymmetric sensorineural hearing loss. Laryngoscope 2017;127(4):939-44.
Semenov YR, Yeh ST, Seshamani M, Wang N-Y, Tobey EA, Eisenberg LS, et al. Age-dependent cost-utility of pediatric cochlear implantation. Ear Hear 2013;34(4):402-12.
Wyatt JR, Niparko JK, Rothman M, DeLissovoy G. Cost utility of the multichannel cochlear implant in 258 profoundly deaf individuals. Laryngoscope 1996;106(7):816-21.
Gillard DM, Harris JP. Cost-effectiveness of stapedectomy vs hearing aids in the treatment of otosclerosis. JAMA Otolaryngology–Head Neck Surg. 2020;146(1):42-8.
Chao T-K, Chen TH-H. Cost-effectiveness of hearing aids in the hearing-impaired elderly: a probabilistic approach. Otol Neurotol 2008;29(6):776-83.
2012 Consumers Union of U.S. What’s fair? Fair healthcare pricing from Healthcare Blue Book. Consumers Report March, 2012.
Zobay O, Dillard LK, Naylor G, Saunders GH. A measure of long-term hearing-aid use persistence based on battery re-ordering data. Ear Hear 2021.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation: Oxford University Press; 2006.
O’Hagan A, McCabe C, Akehurst R, Brennan A, Briggs A, Claxton K, et al. Incorporation of uncertainty in health economic modelling studies. Pharmacoeconomics 2005;23(6):529-36.
Haile LM, Kamenov K, Briant PS, Orji AU, Steinmetz JD, Abdoli A, et al. Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet 2021;397(10278):996-1009.
Claxton KP, Sculpher MJ. Using value of information analysis to prioritise health research. Pharmacoeconomics 2006;24(11):1055-68.
Morris A, Lutman M, Cook A, Turner D. An economic evaluation of screening 60-to 70-year-old adults for hearing loss. J Public Health 2013;35(1):139-46.
Linssen AM, Anteunis LJ, Joore MA. The cost-effectiveness of different hearing screening strategies for 50-to 70-year-old adults: a Markov model. Value Health 2015;18(5):560-9.
Borre ED, Diab MM, Ayer A, Zhang G, Emmett SD, Tucci DL, et al. Evidence gaps in economic analyses of hearing healthcare: a systematic review. EClinicalMedicine 2021;35:100872.
Bettger JP, Dolor RJ, Witsell DL, Dubno JR, Pieper CF, Walker AR, et al. Comparative implementation-effectiveness of three strategies to perform hearing screening among older adults in primary care clinics: study design and protocol. BMC Geriatr 2020;20:1-10.
Khan KM, Bielko SL, Barnes PA, Evans SS, Main AL. Feasibility of a low-cost hearing screening in rural Indiana. BMC Public Health 2017;17(1):1-9.
Saunders G, Frederick M, Silverman S, Arnold M, Chisolm T. Community-based hearing screening: pros, cons, and lessons learned. Innov Aging 2018;2(Suppl 1):360.
Saunders GH, Frederick MT, Silverman SC, Penman T, Gardner A, Chisolm TH, et al. Hearing screening in the community. J Am Acad Audiol 2019;30(02):145-52.
Mahomed-Asmail F, Swanepoel DW, Eikelboom RH, Myburgh HC, Hall J. Clinical validity of hearScreen™ smartphone hearing screening for school children. Ear Hear 2016;37(1):e11-e7.
United States Senate. Over-the-Counter Hearing Aid Act of 2017. Accessed 17 February 2022 at https://www.congress.gov/bill/115th-congress/senate-bill/670.
Lakdawalla DN, Doshi JA, Garrison Jr LP, Phelps CE, Basu A, Danzon PM. Defining elements of value in health care—a health economics approach: an ISPOR Special Task Force report [3]. Value Health 2018;21(2):131-9.
Emmett SD, Francis HW. The socioeconomic impact of hearing loss in US adults. Otol Neurotol 2015;36(3):545-50.
Funding
This study was funded by the National Institute on Deafness and Other Communication Disorders and the National Institute on Aging (3UL1-TR002553-03S3 and F30 DC019846). The funding source had no role in the design, analysis, or interpretation of the study or in the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Dubno declares grants from the National Institutes of Health, participation on the National Institute of Deafness and Other Communication Disorders Data Safety Monitoring Board, participation on the National Institute on Aging ACHIEVE study Data Safety Monitoring Board, participation on the Board of Directors of the Hearing Health Foundation, and the Executive Council of the American Society of Audiologists.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 371 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borre, E.D., Dubno, J.R., Myers, E.R. et al. Model-Projected Cost-Effectiveness of Adult Hearing Screening in the USA. J GEN INTERN MED 38, 978–985 (2023). https://doi.org/10.1007/s11606-022-07735-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07735-7






