Abstract
Background
Ensuring equitable care remains a critical issue for healthcare systems. Nationwide evidence highlights the persistence of healthcare disparities and the need for research-informed approaches for reducing them at the local level.
Objective
To characterize key contributors in racial/ethnic disparities in emergency department (ED) throughput times.
Design
We conducted a sequential mixed methods analysis to understand variations in ED care throughput times for patients eventually admitted to an emergency department at a single academic medical center from November 2017 to May 2018 (n=3152). We detailed patient progression from ED arrival to decision to admit and compared racial/ethnic differences in time intervals from electronic medical record time-stamp data. We then estimated the relationships between race/ethnicity and ED throughput times, adjusting for several patient-level variables and ED-level covariates. These quantitative analyses informed our qualitative study design, which included observations and semi-structured interviews with patients and physicians.
Key Results
Non-Hispanic Black as compared to non-Hispanic White patients waited significantly longer during the time interval from arrival to the physician’s decision to admit, even after adjustment for several ED-level and patient demographic, clinical, and socioeconomic variables (Beta (average minutes) (SE): 16.35 (5.8); p value=.005). Qualitative findings suggest that the manner in which providers communicate, advocate, and prioritize patients may contribute to such disparities. When the race/ethnicity of provider and patient differed, providers were more likely to interrupt patients, ignore their requests, and make less eye contact. Conversely, if the race/ethnicity of provider and patient were similar, providers exhibited a greater level of advocacy, such as tracking down patient labs or consultants. Physicians with no significant ED throughput disparities articulated objective criteria such as triage scores for prioritizing patients.
Conclusions
Our findings suggest the importance of (1) understanding how our communication style and care may differ by race/ethnicity; and (2) taking advantage of structured processes designed to equalize care.
Similar content being viewed by others
INTRODUCTION
Healthcare systems continue to struggle with providing equitable care irrespective of personal characteristics such as gender, race/ethnicity, geographic location, and socioeconomic status.1,2 Over a decade since the Institute of Medicine (IOM) report Unequal Treatment and ten decades since the Flexner Report, racial/ethnic disparities in care quality persist.3,4 National organizations focused on improving healthcare quality have launched initiatives to galvanize health system efforts to address inequities in care.5,6 In response, health systems have begun to stratify performance measures7,8 by demographic characteristics to identify any existing disparities.1,9 Agencies assessing healthcare performance have focused on equity in emergency department (ED) throughput,10 given its effects on inpatient care quality, length of stay, and costs.11,12,13,14,15,16 Such efforts have identified disparities across multiple institutions nationally, including at our institution, where unadjusted analyses over several reporting periods revealed a racial/ethnic disparity in wait times from ED arrival to hospital admission. The objective of this mixed-methods study was to characterize contributors to this observed racial/ethnic variation in ED throughput.
METHODS
We conducted a sequential explanatory mixed-methods analysis17,18 to evaluate racial/ethnic variations in ED care delivery and wait times at a single academic level 1 trauma, comprehensive stroke, and STEMI center that serves a predominantly non-Hispanic Black community. In this framework, qualitative analysis is used to help explain quantitative findings. Informed by the racial/ethnic variations in ED throughput cited by Vizient19 and criteria used to assess performance by CMS,20 we analyzed data extracted from our electronic health records on non-trauma patients eventually admitted through the ED from November 2017 to May 2018. These quantitative analyses informed our qualitative study design, which included a combination of observation and semi-structured interviewing aiming to achieve a depth of understanding sufficient to generate hypotheses for our quantitative findings. Our research team was diverse in gender, race/ethnicity, and hierarchy with a breadth of roles and positions within the organization. The University of Pennsylvania Institutional Review Board approved our study protocol and recruitment language.
Quantitative Methods
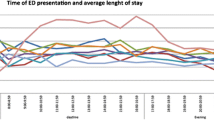
We analyzed demographic, healthcare utilization, and clinical data extracted from the electronic health record on non-trauma patients admitted to the hospital through the ED from November 2017 to May 2018 who self-identified as either non-Hispanic White or Black (n=3152). Of all non-trauma patients admitted during that time period, we excluded only 4.9% (n=163) who did not identify as non-Hispanic White or Black. Prior unadjusted comparisons revealed that non-Hispanic Black as compared to non-Hispanic White patients waited on average 41.4 min longer from their arrival to when a physician requests an inpatient bed (decision to admit) (p=0.002), with no significant difference in boarding time (decision to admit to arrival to inpatient bed). Therefore, our mixed-methods analysis focused on the time from arrival to decision to admit. Our objectives were as follows: (1) to determine the location of the racial/ethnic ED throughput disparity along the process from ED arrival to decision to admit; (2) to assess variability in ED throughput disparities by mode of arrival, time of day, and day of the week; (3) to estimate the association of race/ethnicity with throughput times, adjusting for patient- and ED-level variables. Race/ethnicity was determined from the self-report within the electronic health records and limited to non-Hispanic White and non-Hispanic Black because the remaining race/ethnic groups combined comprised less than 5% of our patient sample.
Using the Wilcoxon rank-sum tests, we compared median time spent at each of the intervals above, stratified by patient race/ethnicity (non-Hispanic White versus non-Hispanic Black patients and mode of arrival (whether patients arrived via Emergency Medical Services (EMS) versus whether they came on their own (walk-ins)). After constructing a process map detailing patient progression from ED arrival to decision to admit, we determined the following time intervals from the electronic health record time-stamp data: (1) ED arrival to triage start; (2) triage time; (3) triage complete to patient room assignment; (4) patient room assignment to physician assigned; (5) physician assigned to decision to admit. We used false discovery methods to account for multiple hypothesis testing. We also estimated the interaction between race/ethnicity and both time of day and day of the week on throughput time disparities21 to inform logistics of qualitative data collection.
We tabulated and compared the distributions of several key patient characteristics by race/ethnicity, using chi-square tests or Wilcoxon rank-sum tests. We then estimated the relationships between race/ethnicity and ED throughput, adjusting for the following patient-level and ED-level covariates informed by key stakeholders: (1) patient age, sex, insurance status/type, and primary language; (2) degree of presenting comorbidity including ED encounter diagnoses (Charlson comorbidity index)22; (3) whether or not a patient had been seen in the ED in the past 30 days and their disposition at the time (admitted versus not admitted); (4) a same-day visit within the health system (yes or no); (5) a call-in referral from a healthcare provider (yes or no); (6) assigned triage score (Emergency Severity Index (ESI))23; (7) admitting service and unit; (8) ED overcrowding score (National ED Over Crowding (NEDOC)) 24; and (9) the presence of a provider in triage (yes or no). We employed generalized estimating equations (GEE) with an exchangeable correlation structure to account for patient clustering by physician provider. In sensitivity analyses, we examined the following additional factors on ED throughput disparities: (1) presence of resident physician assigned to patient; (2) the number of specialty consults ordered; and (3) whether or not an MRI was ordered on ED throughput disparities. Please refer to Appendix E for our complete set of analyses and considerations that determine the categorization of our covariates and final model specifications.
Qualitative Methods
Data Collection
Informed by our quantitative analyses, we obtained data from four sources as follows: (1) semi-structured interviews with patients and community members; (2) general observations of the ED; (3) observations of specific ED physicians followed by (4) semi-structured interviews of observed physicians. All participants were told that the objective of the study was to understand contributors to patient experience and wait times. While patient participants were eventually asked about racial/ethnic disparities in wait times in their semi-structured interviews, all ED staff and providers were not told this was a study examining racial/ethnic disparities. In addition, physicians were interviewed only after the observations were complete. These measures were taken to mitigate the potential Hawthorne effect, though there is mixed evidence that the qualitative researcher’s presence causes substantial alterations in the behavior of those observed.25,26,27 We obtained consent for semi-structured interviews to be audio-recorded and transcribed and to conduct general and physician-specific observations within the emergency department in 2-h intervals at predetermined dates/times. Appendices A–D include all semi-structured interview guides and observational templates pilot tested for content validity and usability. Data were collected until theoretical saturation28—when the addition of new data did not alter our coding schemas or the explanations we were developing to explain patterns found. Saturation was evaluated separately for patient and physician samples.
Patient Semi-Structured Interviews
We conducted 30-min semi-structured telephone interviews with a purposive sample of equal numbers of non-Hispanic White and non-Hispanic Black patients admitted through the ED in the past 6 months (n=10), as well as members from community-based organizations identified by the hospital Office of Community and Government Relations (n=2). We focused on patient interviews after the initial community member interviews, as early interviews revealed that the community stakeholders often could not provide detailed responses to the questions and provided similar responses with less detail than the patient sample. Research assistants asked participants to confirm their race/ethnicity noted in their patient records or provide their race/ethnicity if a community member. Using a 17-item interview guide, we asked about the following: (1) general ED visit experience; (2) perceptions of wait times and why they may occur; (3) impressions of racial/ethnic wait time disparities; (4) any recommendations to improve experience (Appendix A). Participants received a 25-dollar incentive for their time.
General Observations
We conducted eight 120-min observation sessions, purposively sampled at different weekdays and timeshifts. Each 2-h session was divided into 25-min intervals followed by 5-min reflection periods to review and edit fieldnotes. During each session, 2 to 3 research assistants, wearing ED personnel badges, conducted observations at rotating pre-specified areas within the ED informed by our quantitative findings, where they assumed seated positions in low traffic areas, such as in chairs located in the corners of rooms. The research assistants used a template to create contemporaneous reports of their observations (Appendix B). This observational template was structured to capture the following: activity, background setting, location, observants, and interpersonal communications. While the observational field notes captured actions and discussions between all provider types, our analyses centered on interactions directly or indirectly involving the physician, as directed by our quantitative findings. Perceived sex and race/ethnicity of observed clinicians and patients were recorded on the template and then later de-identified for initial coding.
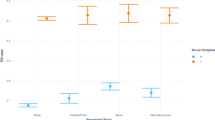
Physician Observation and Semi-Structured Interviews
We determined the distribution of individual physician time differences between non-Hispanic Black and non-Hispanic White patients from our sample dataset. Physicians that had seen at least 10 patients from each racial/ethnic category were grouped in quartiles along this distribution. Of the 36 physicians that met these criteria, 18 physicians had at least one shift during the study period. Of those 18, we recruited 2 to 3 physicians from each quartile for a total of nine participants. Physician race/ethnicity was retrieved from departmental records, which similar to patient medical records is likely self-identified race/ethnicity. Each physician was shadowed for 2 h during their shift followed by a semi-structured telephone interview, conducted within 48 h of their observed shift. The research assistants used a shadowing template similar to the observational template (Appendix D). The 14-item interview guide assessed the following from physician participants: (1) details on their position, including any non-clinical roles, their average number of shifts per month, and types of shifts (e.g., day); (2) perceptions of and approach to a busy shift; (3) views on what patient characteristics or specific populations may be predisposed to experience longer wait times; (4) personal communication style/approach; and (5) general recommendations for optimizing ED workflows 29 (Appendix C).
Data Analysis
All data were stripped of any personal identifiers and imported into NVivo 1230 for coding and analysis. The team jointly annotated at least 10% of data from each source to develop and iteratively refine four distinct codebooks—thematic taxonomies for the categorization of qualitative data.31 The team either double- or triple-coded an additional 10% or more of the sample independently from each data source to estimate inter-rater reliability (IRR).32 For patient interview data, the mean κ (kappa statistic) was 0.82 (range= 0.70–1.00). For general ED observations data, the mean κ was 0.79 (range=0.53–1.00). For physician ED observation and interview data, the mean κ was 0.87 (range=0.78–1.00) and 0.94 (range=0.87–1.00), respectively. The team met routinely to resolve coding discrepancies and refine codebooks. For general observations’ notes, for any instance where two or more coders disagreed, a third and sometimes fourth team member moderated the discussion, reviewed all observational notes, and facilitated a final coding determination.
To ensure anonymity and avoid anchoring bias, the team members who coded the data were distinct from those who collected the data. In addition, the three research assistants that conducted the general observations did not code their own observations. Team members that then analyzed codes for emerging themes were blind initially to the perceived race/ethnicity and sex of interviewees and observed patients and healthcare personnel. All team members involved with recruiting, conducting, coding, and analyzing qualitative data were blind to physician groupings and what they represented in terms of performance. Data were unblinded after coding in two stages. We first unblinded participant race/ethnicity to identify patterns in communication and interactions between physician/staff and patients of the same race/ethnicity (concordant pairs) versus not (discordant pairs). We then unblinded the performance of the four groups of interviewed and shadowed physicians in terms of racial/ethnic disparities in ED throughput; this was done only after we had first examined coding patterns by physician groupings while blinded to each group’s quartile rank.
RESULTS
Quantitative Findings
Among our sample population of patients (n= 3152) seen in the ED and eventually admitted, 54.6% of non-Hispanic Black patients were female with 23.9% insured by Medicaid as compared to 44.0% of non-Hispanic White patients that were female with only 8.3% insured by Medicaid. Over 30% of non-Hispanic White patients had a same-day visit and 17.8% had a call-in referral prior to presenting to the ED, as compared to 14.6% of non-Hispanic Black with a same-day visit and 8.8% with a call-in referral. Lastly, non-Hispanic Black patients presented with greater comorbidities as compared to non-Hispanic White (Charlson comorbidity index 0.44 versus 0.30). Table 1 details the remaining baseline characteristics.
The only time interval along this path from arrival to decision to admit with a significant racial/ethnic disparity in median times and in mean time after accounting for multiple hypothesis testing was from physician assignment to inpatient bed request (physician assigned to decision to admit). Evaluating this disparity by patient’s mode of arrival revealed that non-Hispanic Black as compared to non-Hispanic White patients who self-presented (“walk-ins”) waited on average 29 min longer from arrival to decision to admit (p=.0006), with the only significant racial/ethnic disparities during the interval between physician assignment and inpatient bed request (Table 2). We did not find a significant ED wait time racial/ethnic disparity among patients that arrived via EMS; however, non-Hispanic Black as compared to non-Hispanic White patients had significantly higher mean triage acuity scores. There were no significant interactions between racial/ethnic wait times, time of day, or day of the week. In adjusted models, accounting for patient characteristics, ESI score, mode of arrival, admitting service and unit, and ED process variables, the racial/ethnic ED throughput disparity attenuated to 16.35 min but remained significant (p<.0001) (Table 3). Lastly, additional sensitivity analyses revealed no significant differences in model estimations of throughput disparity after adjusting for the presence of a resident, the number of speciality consults, and a MRI order (Appendix E).
Qualitative Findings
Theme 1: Patients Perceptions of ED Wait Times Align but Their Recommendations Differ
Patients’ perceived wait times mostly aligned with actual wait times and ranged from 1 to 24 h with four time points of reference: arrival, leaving waiting room, seeing doctor, and departure to floor. In the instances where patient perceptions differed from actual wait times, patients underestimated their wait times. Patients perceived wait times as ending upon seeing a physician and did not appear to distinguish between seeing an ED physician versus seeing an inpatient attending physician. Patients viewed prolonged wait as inevitable and attributed their wait times to the following factors: (1) ED census; (2) complexity of patient (i.e., sicker patients seen faster; (3) “squeaky wheel” effect (i.e., those who complain/make noise are seen faster). There were no discernible patterns by race/ethnicity on wait time perceptions.
However, reactions to the hypothetical presence of wait time disparities varied by race/ethnicity, as did recommendations for improvement. Non-Hispanic Black patients reported having previously witnessed such disparities in various settings, whereas non-Hispanic White patients expressed surprise, disbelief, or lack of understanding. Moreover, only non-Hispanic Black patients’ recommendations for improvement focused on system-level processes, such as providing staff with communication skills training.
Theme 2: Provider Communications with or in Reference to Patients Differ by Race/Ethnicity
Communicating with Patients
Observations revealed consistent patterns of communication between healthcare personnel (physician, nurse, or technician) and patients of similar race/ethnicity (concordant pairs) and those of dissimilar race/ethnicity (discordant pairs).
The communication style of healthcare personnel during discordant interactions as compared to concordant interactions differed in the following ways (Table 4): (1) Verbal communications involved more frequent interruptions of patients by health care personnel; and (2) Non-responses (e.g., ignoring or dismissing) to patient requests and/or concerns were more frequent; and (3) Nonverbal communication involved providers standing greater than a foot away from the bed as compared to close proximity to the patient. Seventy-five percent of codes for bedside position greater than a foot away from the bed were among discordant pairs. Of all the negative verbal and non-verbal interactions coded, two-thirds were among discordant pairs.
Communications Referencing Patients
Another pattern that emerged was a difference in how healthcare personnel referenced their patients in interactions with each other depending on whether the patient was similar in race/ethnicity to the provider or not. Among concordant pairs, there was observed advocacy, such as expressing concern for patient’s satisfaction, tracking down labs, or contacting a consultant. Conversely, there were no noted observations of advocacy among discordant pairs. Moreover, among discordant pairs, there were instances of dark or negative humor and a lack of advocacy when discussing patients with their colleagues (Table 4).
Theme 3: Physicians Differ in Their Approach to Prioritizing Patients
Physician interviewees from the group without significant disparities consistently articulated a clear set of criteria for prioritizing patient evaluations, which included the following: (1) arrival by EMS (including perceived acuity using visual cues and input of EMS workers); (2) objective wait times; (3) triage score (ESI).33,34 Notably, 4 of 5 physicians from groups with minimal/no disparities mentioned ESI as a criterion used to prioritize patients. In contrast, 1 of 4 physicians from groups displaying significant wait time disparities mentioned ESI, with the sole mention being a rebuke of its validity.
Theme 4: Physician Communication Styles and Attitudes
Physicians who in their interviews perceived poor communication style as a patient attribute that causes longer wait times did not adapt the way they spoke during observed encounters in order to confirm understanding or elicit clearer responses. Among physicians, negative verbal interactions (e.g., frequent interruptions, asking patients to “speed it up”) occurred 21% of the time among discordant physician and patient pairs and in contrast were not observed among concordant physician and patient pairs (Table 4). Of all recorded adaptive communication (e.g., asking questions, confirming understanding), 75% was between concordant pairs as compared to 25% among discordant pairs (Table 5). Physicians with this non-adaptive communication style were found to have significant disparities upon unblinding our data. We also found that all physicians who expressed dissatisfaction with hospital “administration” during their interviews were from the group with significant disparities.
Theme 5: Physicians Avoid Discussing Race/Ethnicity
When asked during interviews what patient attributes or specific patient populations may experience delays in care or longer wait times, the majority of physician interviewees did not reference race/ethnicity. Race was directly mentioned only three times. One physician volunteered race without prompting and stated, “I don’t think race is necessarily the issue, I think it's maybe more of a reflection of connectedness or knowing how to say the right things to prompt a response or just being sicker.” Physicians, however, did mention age, gender, and insurance as patient characteristics that contribute to delays in care. Physicians also perceived the following other patient attributes as contributors to longer wait times: “unsophisticated,” “difficult to understand,” “not well-to-do,” “not well-connected,” “urban,” “no care integration,” and “regular consumers of healthcare.” The only two physicians that cited that populations may experience delays in care or longer wait times due to their race/ethnicity were from the group without significant disparities.
DISCUSSION
In this sequential mixed-methods study, we examined racial/ethnic disparities in ED throughput among patients eventually admitted to the hospital. We determined that significant racial/ethnic disparities at our hospital occurred during the physician evaluation period prior to requesting an inpatient bed, a notable finding given that the bulk of evidence to date has explored disparities in the time before physician evaluation. This disparity attenuated but remained significant even after adjustment for patient and ED characteristics. Interestingly, this disparity was not observed among patients arriving via EMS. However, the lack of significant differences within this cohort suggests a disparity given the significantly higher triage acuity scores for non-Hispanic Black as compared to non-Hispanic White patients.
To better characterize the differences identified in our quantitative analysis, we used a series of direct observations and semi-structured interviews. While it is reassuring that the patients in our study perceived their “wait time” as ending at the time of ED physician evaluation, this throughput disparity still reflects unequal treatment. Our quantitative analysis narrowed the location of the disparity to the interval from physician assigned to hospital bed requested. This is a complex period encompassing numerous patient-staff encounters beyond the physician-patient interaction and our observations aimed to capture that. Given this, we focused on physician-staff interactions, but captured other patient-staff interactions as well. Our qualitative data suggest that the manner in which physicians, and healthcare personnel more generally, communicate with, advocate for, and prioritize patients may have contributed to these disparities. These findings highlight the importance of (1) examining and improving upon our attitudes and communication styles; (2) taking advantage of structured processes designed to equalize care; and (3) acknowledging how our care may differ by race/ethnicity. Furthermore, we believe the methods utilized and key insights they revealed may prove useful for other health systems seeking to minimize disparities in care.
Communication and Bias Training
Prior evidence suggests that physicians deliver less information to, spend less time with, and engage in less supportive talk with racial/ethnic minorities as compared to non-minority patients.3,35 Such racial/ethnic differences extend to nonverbal communications.36,37 Ineffective provider-patient communication has been shown to influence readmission rates, medication adherence, patient satisfaction, and end-of-life care.37,38,39,40 Our study builds upon this work and highlights poignant racial/ethnic differences in provider verbal and nonverbal communications with patients and in provider advocacy for patients. We found relationships between physicians’ attitudes and their communication styles, and both may be driving disparities in ED throughput times. Notably, only non-Hispanic Black patients in our study recommended communication training for providers as a mechanism to combat wait time disparities. Effective communication training41 should focus on improving nonverbal and verbal communication, honing adaptive communication styles, learning evidence-based methods to confirm patient understanding (e.g. teach back),42 and learning how to mitigate potential unconscious biases.43
Use of Structured Processes to Mitigate Bias
We found that physicians without significant wait-time disparities uniformly articulated standardized criteria used to prioritize patient evaluation. Specifically, they reported using objective wait times and the Emergency Severity Index (ESI), a five-level ED triage score designed and validated as an effective method to stratify patients into groups based on clinical need to signal how quickly they should be seen.23,33,34,44 In contrast, those physicians with significant racial/ethnic wait-time disparities either did not mention ESI as a criterion they use or explicitly stated they do not believe in its utility. Of note, we found no significant racial/ethnic disparities in assigning ESI rating nor in triage wait time, despite some work that demonstrates racial/ethnic disparities in ESI assignment and triage.45,46,47 While the interval containing the disparity in the present study occurred after room placement, the primary ED event influenced by ESI, it is possible that ESI influenced the sequence and expediency with which physicians evaluated patients after assigning themselves, particularly when assigning themselves to multiple patients simultaneously during high-volume times. Supported by prior evidence of the effectiveness of ESI in decreasing ED wait times and length of stay,48 our study suggests the need to develop strategies that promote routine use of objective data to prioritize patients. Structured processes, akin to ESI use, should be considered interventions to reduce bias and disparities in care even beyond the ED.49,50,51
Discussing Race/Ethnicity
We found that physicians avoided citing race/ethnicity as a potential reason for longer wait times, but cited numerous other demographic traits. Many, however, referenced terms such as “urban” that do not denote a specific racial/ethnic category by their strict definition but are often racially marked—that is, the presence of certain contextual cues, or awareness that these terms have in the past been used to refer to a certain race/ethnicity, leads to their use as a proxy for a racial/ethnic group.52 Interviewers did not explicitly probe physicians for the meaning of these terms as these patterns were elucidated only after analysis was complete; however, prior evidence exists for the use of such terms as proxies for race/ethnicity.53 Usage of these terms in lieu of explicit racial/ethnic signifiers suggests that physicians may be aware of the possibility that race impacts care, but remain uncomfortable discussing race/ethnicity and racial/ethnic differences in care.
This avoidance of discussing race/ethnicity presents several challenges. First, using proxies for race/ethnicity such as socioeconomic status (e.g., “not-well-to-do”) reinforces stereotypes that (1) are often inaccurate and (2) have been shown to exacerbate healthcare disparities.54,55,56,57 Second, the avoidance of discussing race/ethnicity itself, or “strategic color-blindness,” has been shown to worsen social interactions between white and black individuals.58,59 Moreover, explicitly recognizing race/ethnicity as a factor influencing social interactions is a key prerequisite to applying strategies that have shown to reduce bias, such as perspective-taking.56 Future inquiry should consider how physicians may be supported and encouraged to openly discuss how patients may experience differential care based on their perceived race/ethnicity.
LIMITATIONS
Our study has several limitations. Our sequential mixed methods design circumscribed the sample size of our physician interviews and targeted observations. We focused on the limited number of physicians that met the criteria to rank their performance on throughput disparities using quantitative data, and only a portion of them had shifts during the study period. However, in enrolling 50% of eligible and available attendings (n=9), we were able to reach theoretical saturation with a sample size not atypical in qualitative work.18,60 We determined race/ethnicity in our observational data as perceived race/ethnicity rather than self-report. Prior work suggests that socially assigned as compared to self-identified race/ethnicity is significantly associated with unequal care.61,62 Notably, there were no non-Hispanic Black physicians in the cohort studied by direct observation. As a result, all observed concordant physician-patient pairs were between those that were non-Hispanic White. However, we did observe concordant interactions between non-physician staff and patients who were non-Hispanic Black, and all patterns observed were similar irrespective of race/ethnicity of the concordant pairs. Our study relies on ED timestamp data, and there is some evidence that this has lower precision than passive observations,63 but the use of timestamp data is the norm for CMS performance assessment.20 This single center services West Philadelphia, which does not have a racial/ethnic majority and provides a useful backdrop for comparisons by race/ethnicity. In addition, our ability to benchmark our findings with the growing evidence of the role of provider bias, patient-provider communications, and disparities in quality of care29,64 speaks in part to the generalizability of our study results.
CONCLUSION
Nationwide studies highlight the persistence of healthcare disparities and the need for research-informed approaches for reducing them at the local level.65 This study demonstrates how health systems can employ mixed methods to evaluate local disparities while yielding generalizable insights to mitigate bias and minimize disparities in care.
References
Chin MH. How to achieve health equity. N Engl J Med. 2014;371(24):2331-2. doi:https://doi.org/10.1056/NEJMe1412264
Six Domains of Health Care Quality. Agency for Healthcare Research and Quality, Rockville, MD. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/talkingquality/measures/six-domains.html. Accessed August 9 2019.
Nelson AR, Stith AY, Smedley BD. Unequal treatment: confronting racial and ethnic disparities in health care (full printed version): National Academies Press; 2002.
Duffy TP. The Flexner Report--100 years later. Yale J Biol Med. 2011;84(3):269-76.
Wyatt R LM, Botwinick L, Mate K, Whittington J. Achieving Health Equity: A Guide for Health Care Organizations. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement2016.
American Hospital Association #123Equity Campaign to Eliminate Health Care Disparities. 2015. http://www.equityofcare.org/. .
Commission TJ. Performance Measurement: Accountability Measures. https://www.jointcommission.org/accountability_measures.aspx. .
Performance Measurement. The Joint Commission. The Joint Commission. https://www.jointcommission.org/core_measure_sets.aspx. .
Chin MH, Goldmann D. Meaningful Disparities Reduction Through Research and Translation Programs. JAMA. 2011;305(4):404-5. doi:https://doi.org/10.1001/jama.2011.26
Specifications Manual for National Hospital Inpatient Quality Measures. The Joint Commission. https://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx. Accessed August 8 2019.
Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63-8.
Handel DA, French LK, Nichol J, Momberger J, Fu R. Associations Between Patient and Emergency Department Operational Characteristics and Patient Satisfaction Scores in an Adult Population. Annals of Emergency Medicine.64(6):604-8. doi:10.1016/j.annemergmed.2014.07.451
Huang Q, Thind A, Dreyer JF, Zaric GS. The impact of delays to admission from the emergency department on inpatient outcomes. BMC emergency medicine. 2010;10:16. doi:https://doi.org/10.1186/1471-227x-10-16
Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. The American journal of emergency medicine. 2010;28(3):304-9. doi:https://doi.org/10.1016/j.ajem.2008.12.014
Pines JM, Garson C, Baxt WG, Rhodes KV, Shofer FS, Hollander JE. ED crowding is associated with variable perceptions of care compromise. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14(12):1176-81. doi:https://doi.org/10.1197/j.aem.2007.06.043
Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):510-6. doi:https://doi.org/10.1016/j.annemergmed.2007.07.021
Ivankova NV, Creswell JW, Stick SL. Using Mixed-Methods Sequential Explanatory Design: From Theory to Practice. Field Methods. 2006;18(1):3-20. doi:https://doi.org/10.1177/1525822x05282260
O’Reilly M, Parker N. ‘Unsatisfactory Saturation’: a critical exploration of the notion of saturated sample sizes in qualitative research. Qualitative Research. 2013;13(2):190-7. doi:https://doi.org/10.1177/1468794112446106
Vizient. https://www.vizientinc.com/. Accessed October 20 2020.
Centers for Medicare & Medicaid Services. Hospital Compare Web site. . Available at https://www.medicare.gov/hospitalcompare/search.html.
Johnson TJ, Hickey RW, Switzer GE, Miller E, Winger DG, Nguyen M, et al. The Impact of Cognitive Stressors in the Emergency Department on Physician Implicit Racial Bias. Acad Emerg Med. 2016;23(3):297-305. doi:https://doi.org/10.1111/acem.12901
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373-83. doi: https://doi.org/10.1016/0021-9681(87)90171-8
Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7(3):236-42. doi:https://doi.org/10.1111/j.1553-2712.2000.tb01066.x
Weiss SJ, Derlet R, Arndahl J, Ernst AA, Richards J, Fernandez-Frackelton M, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med. 2004;11(1):38-50.
Paradis E, Sutkin G. Beyond a good story: from Hawthorne Effect to reactivity in health professions education research. Med Educ. 2017;51(1):31-9. doi:https://doi.org/10.1111/medu.13122
Stoddart K. The Presentation of Everyday Life: Some Textual Strategies for “Adequate Ethnography”. Urban Life. 1986;15(1):103-21. doi:https://doi.org/10.1177/0098303986015001004
Monahan T, Fisher JA. Benefits of "Observer Effects": Lessons from the Field. Qualitative research : QR. 2010;10(3):357-76. doi:https://doi.org/10.1177/1468794110362874
Glaser BG, Strauss AL. Discovery of grounded theory: Strategies for qualitative research: Routledge; 2017.
Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A Systematic Review of the Impact of Physician Implicit Racial Bias on Clinical Decision Making. Acad Emerg Med. 2017;24(8):895-904. doi:https://doi.org/10.1111/acem.13214
NVivo Qualitative Data Analysis Software. QSR International Pty Ltd.; Version 11, 2015.
Macqueen K, McLellan-Lemal E, Kay K, Milstein B, Cdc A. Codebook Development for Team-Based Qualitative Analysis. Cultural Anthropology. 1998;10:pp. 31–6. doi:https://doi.org/10.1177/1525822X980100020301
Cohen J. A Coefficient of Agreement for Nominal Scales. Educational and Psychological Measurement. 1960;20(1):37-46. doi:https://doi.org/10.1177/001316446002000104
Gilboy N, Tanabe T, Travers D, Rosenau AM. Emergency Severity Index (ESI): A triage tool for emergency department. Rockville, MD: Agency for Healthcare Research and Quality. 2011.
Ganjali R, Golmakani R, Ebrahimi M, Eslami S, Bolvardi E. Accuracy of the Emergency Department Triage System using the Emergency Severity Index for Predicting Patient Outcome; A Single Center Experience. Bulletin of emergency and trauma. 2020;8(2):115-20. doi:10.30476/BEAT.2020.46452
Disparities In Physician Care: Experiences And Perceptions Of A Multi-Ethnic America. Health Affairs. 2008;27(2):507-17. doi:10.1377/hlthaff.27.2.507
Elliott AM, Alexander SC, Mescher CA, Mohan D, Barnato AE. Differences in Physicians' Verbal and Nonverbal Communication With Black and White Patients at the End of Life. Journal of pain and symptom management. 2016;51(1):1-8. doi:https://doi.org/10.1016/j.jpainsymman.2015.07.008
Robinson JD, Jagsi R. Physician-Patient Communication—An Actionable Target for Reducing Overly Aggressive Care Near the End of Life. JAMA Oncology. 2016;2(11):1407-8. doi:https://doi.org/10.1001/jamaoncol.2016.1948
Acher AW, LeCaire TJ, Hundt AS, Greenberg CC, Carayon P, Kind AJ, et al. Using Human Factors and Systems Engineering to Evaluate Readmission after Complex Surgery. Journal of the American College of Surgeons. 2015;221(4):810-20. doi:https://doi.org/10.1016/j.jamcollsurg.2015.06.014
Manary MP, Boulding W, Staelin R, Glickman SW. The Patient Experience and Health Outcomes. New England Journal of Medicine. 2012;368(3):201-3. doi:https://doi.org/10.1056/NEJMp1211775
Zolnierek KBH, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826-34. doi:https://doi.org/10.1097/MLR.0b013e31819a5acc
Chou C. Time to start using evidence-based approaches to patient engagement. NEJM Catalyst. 2018;4(2).
Nouri SS, Rudd RE. Health literacy in the “oral exchange”: An important element of patient–provider communication. Patient education and counseling. 2015;98(5):565-71.
Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Processes & Intergroup Relations. 2016;19(4):528-42. doi:https://doi.org/10.1177/1368430216642029
Tanabe P, Gimbel R, Yarnold PR, Kyriacou DN, Adams JG. Reliability and validity of scores on The Emergency Severity Index version 3. Acad Emerg Med. 2004;11(1):59-65. doi:https://doi.org/10.1197/j.aem.2003.06.013
Vigil JM, Alcock J, Coulombe P, McPherson L, Parshall M, Murata A, et al. Ethnic Disparities in Emergency Severity Index Scores among U.S. Veteran’s Affairs Emergency Department Patients. PLOS ONE. 2015;10(5):e0126792. doi:10.1371/journal.pone.0126792
Vigil JM, Coulombe P, Alcock J, Kruger E, Stith SS, Strenth C, et al. Patient Ethnicity Affects Triage Assessments and Patient Prioritization in U.S. Department of Veterans Affairs Emergency Departments. Medicine. 2016;95(14):e3191. doi:10.1097/md.0000000000003191
Zook HG, Kharbanda AB, Flood A, Harmon B, Puumala SE, Payne NR. Racial Differences in Pediatric Emergency Department Triage Scores. The Journal of emergency medicine. 2016;50(5):720-7. doi:https://doi.org/10.1016/j.jemermed.2015.02.056
Maleki M, Fallah R, Riahi L, Delavari S, Rezaei S. Effectiveness of Five-Level Emergency Severity Index Triage System Compared With Three-Level Spot Check: An Iranian Experience. Arch Trauma Res. 2015;4(4):e29214-e. doi:10.5812/atr.29214
Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260(1):174-81.
Pasero C, Puntillo K, Li D, Mularski RA, Grap MJ, Erstad BL, et al. Structured approaches to pain management in the ICU. Chest. 2009;135(6):1665-72.
Abimanyi-Ochom J, Bohingamu Mudiyanselage S, Catchpool M, Firipis M, Wanni Arachchige Dona S, Watts JJ. Strategies to reduce diagnostic errors: a systematic review. BMC medical informatics and decision making. 2019;19(1):174-. doi:10.1186/s12911-019-0901-1
Urciuoli B. Talking/not talking about race: The enregisterments of culture in higher education discourses. Journal of Linguistic Anthropology. 2009;19(1):21-39.
Woodson AN. Racial code words, re-memberings and Black kids’ civic imaginations: A critical race ethnography of a post-civil rights leader. Anthropology & Education Quarterly. 2019;50(1):26-47.
Health Disparities By Race And Class: Why Both Matter. Health Affairs. 2005;24(2):343-52. doi:https://doi.org/10.1377/hlthaff.24.2.343
Aronson J, Burgess D, Phelan SM, Juarez L. Unhealthy interactions: the role of stereotype threat in health disparities. American journal of public health. 2013;103(1):50-6. doi:https://doi.org/10.2105/AJPH.2012.300828
Chapman EN, Kaatz A, Carnes M. Physicians and Implicit Bias: How Doctors May Unwittingly Perpetuate Health Care Disparities. Journal of General Internal Medicine. 2013;28(11):1504-10. doi:https://doi.org/10.1007/s11606-013-2441-1
Nelson AR, Smedley BD, Stith AY. Unequal Treatment:: Confronting Racial and Ethnic Disparities in Health Care (with CD): National Academies Press; 2009.
Apfelbaum EP, Sommers SR, Norton MI. Seeing race and seeming racist? Evaluating strategic colorblindness in social interaction. J Pers Soc Psychol. 2008;95(4):918-32. doi:https://doi.org/10.1037/a0011990
West TV, Schoenthaler A. Color-Blind and Multicultural Strategies in Medical Settings. Social Issues and Policy Review. 2017;11(1):124-58. doi:https://doi.org/10.1111/sipr.12029
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field methods. 2006;18(1):59-82.
Macintosh T, Desai MM, Lewis TT, Jones BA, Nunez-Smith M. Socially-assigned race, healthcare discrimination and preventive healthcare services. PLoS One. 2013;8(5):e64522. doi:https://doi.org/10.1371/journal.pone.0064522
White K, Lawrence JA, Tchangalova N, Huang SJ, Cummings JL. Socially-assigned race and health: a scoping review with global implications for population health equity. Int J Equity Health. 2020;19(1):25. doi:https://doi.org/10.1186/s12939-020-1137-5
Gordon BD, Flottemesch TJ, Asplin BR. Accuracy of staff-initiated emergency department tracking system timestamps in identifying actual event times. Ann Emerg Med. 2008;52(5):504-11. doi:https://doi.org/10.1016/j.annemergmed.2007.11.036
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science & Medicine. 2018;199:219-29.
Wasserman J, Palmer RC, Gomez MM, Berzon R, Ibrahim SA, Ayanian JZ. Advancing health services research to eliminate health care disparities. American journal of public health. 2019;109(S1):S64-S9.
Acknowledgements
We would like to thank Oluwarotimi (Tim) Vaughan-Ogunlusi, Elaine Weigelt, Barbara Biney, and Laura Lombardo for their assistance with community engagement and recruitment. We would like to also thank Meredith Lawler, Maryam Behta, and Tiffani Johnson for their guidance on the grant and Kevin Fosnocht, James Ballinghoff, and Michele Volpe for their endorsement and administrative support.
Funding
This project was funded via a Patient-Centered Outcomes Research Pilot Study grant from the Center for Therapeutic Effectiveness Research at the Perelman School of Medicine, University of Pennsylvania. In addition, Jaya Aysola, MD, MPH, was supported in part by an American Cancer Society - Tri-State CEO’s Against Cancer Mentored Research Scholar Grant, MRSG-17-155-01- CPPB. Lastly, support for the analysis of this study came from the Office of Inclusion, Diversity, and Equity, Perelman School of Medicine, University of Pennsylvania.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sean Foster and Mira Mamtani are co-last authors.
Supplementary Information
ESM 1
(DOCX 121 kb)
Rights and permissions
About this article
Cite this article
Aysola, J., Clapp, J.T., Sullivan, P. et al. Understanding Contributors to Racial/Ethnic Disparities in Emergency Department Throughput Times: a Sequential Mixed Methods Analysis. J GEN INTERN MED 37, 341–350 (2022). https://doi.org/10.1007/s11606-021-07028-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07028-5