Abstract
Background
Transgender and gender-diverse individuals are particularly vulnerable to healthcare discrimination and related health sequelae.
Objective
To demonstrate diversity in demographics and explore variance in needs at the time of intake among patients seeking care at a large, urban gender health program.
Design
We present summary statistics of patient demographics, medical histories, and gender-affirming care needs stratified by gender identity and sexual orientation.
Participants
We reviewed all intake interviews with individuals seeking care in our gender health program from 2017 to 2020.
Main Measures
Clients reported all the types of care in which they were interested at the time of intake as their “reason for call” (i.e., establish primary care, hormone management, surgical services, fertility services, behavioral health, or other health concerns).
Key Results
Of 836 patients analyzed, 350 identified as trans women, 263 as trans men, and 223 as non-binary. The most prevalent sexual identity was straight among trans women (34%) and trans men (38%), whereas most (69%) non-binary individuals identified as pansexual or queer; only 3% of non-binary individuals identified as straight. Over half of patients reported primary care, hormone management, or surgical services as the primary reason for contacting our program. Straight, transgender women were more likely to report surgical services as their primary reason for contacting our program, whereas gay transgender men were more likely to report primary care as their reason.
Conclusions
Individuals contacting our gender health program to establish care were diverse in sexual orientation and gender-affirming care needs. Care needs varied with both gender identity and sexual orientation, but primary care, hormone management, and surgical services were high priorities across groups. Providers of gender-affirming care should inquire about sexual orientation and detailed treatment priorities, as trans and gender-diverse populations are not uniform in their treatment needs or goals.
Similar content being viewed by others
INTRODUCTION
Transgender and gender-diverse individuals, or those who do not (or do not fully) identify with the gender assigned to them at birth, are particularly vulnerable to healthcare discrimination and related health sequelae. Although data suggest that about 0.5% of the United States (US) population identifies as transgender or otherwise gender-diverse (actual numbers are likely higher), research in this population is in its infancy and offers limited insight into how best to care for trans and gender-diverse individuals who present for care. What the current US health system does offer is evidence of poor healthcare engagement and outcomes, high risk of victimization, and lack of cultural competency and training among medical professionals.1,2,3
Specialized gender health programs around the world and US have recently grown amid increased demand and support for gender-affirming care, but quality and access vary widely.4,5,6 Gender-affirming care is complex, often requiring a multidisciplinary approach for behavioral, hormonal, and surgical treatments.4 Additionally, many gender health clinics serve as a safe place for primary care, given high rates of discrimination and victimization experienced in health care settings.7 Despite these challenges, gender-affirming care has been associated with improved quality of life and psychosocial outcomes.8,9,10
In addition to variation in gender identity, trans and gender-diverse populations frequently report intersecting diversity in sexual orientation identity,11, 12 and evidence suggests that sexual orientation may influence risk for certain disease states. For example, gay transgender men who engage in penile-vaginal intercourse may be at increased risk for high-risk cervical HPV infections.13 Medical comorbidities, such as HIV or depression, may differ among transgender women who identify as straight, lesbian, or bisexual.14 Measurement of sexual orientation in this population is complicated for many reasons, however, not the least of which is the contingency of common labels for sexual orientation on the subject’s own gender. Identities may change over time — the relationship between development of gender and sexual orientation identities are complex, interrelated, and not fully understood — but evidence suggests that gender-affirming care may alter individuals’ perceptions of their own sexuality.15 Given the impact of anatomy on the ways in which individuals can interact sexually, sexual orientation may even influence the type of gender-affirming care desired; however, there is a lack of research in this area.
With the goal of (1) describing the diversity of identities and care needs seen in this population and (2) exploring factors that vary with type of gender-affirming care sought, including sexual orientation, we describe data from initial intake interviews completed as part of enrollment into a gender health program in Los Angeles established in 2017. The program provides medical, behavioral, surgical, and case management services to patients across the gender spectrum. Our results may provide healthcare professionals useful data for shared decision-making regarding gender-affirming care and help inform public health strategies and health resource utilization for other gender health programs.
METHODS
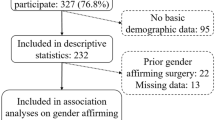
After approval of the institutional review board, we conducted a descriptive analysis utilizing intake interviews for patients enrolling in our health center’s gender health program. Intake interviews were conducted telephonically by administrative specialists or case managers as part of our case management program, in which clients may participate regardless of whether they receive care at our health system. Patient intake interviews cover client demographics, transition history, and medical history and needs, all self-reported. As of July 2020, 1124 assessments were recorded in our Gender Health Program database. Repeat assessments were removed (n=124). Only patients 18 years or older were included in this analysis (n=101 interviews removed). Potential patients who called the program but did not complete an intake assessment were not recorded.
Gender Identity
Given the fluidity of identities and at patient request, clients could report multiple pronouns, gender identities, and sexual orientations. Clients were grouped into larger categories as follows: (1) clients reporting identities such as “genderqueer,” “gender fluid,” or “gender non-binary” were grouped into the “non-binary” group regardless of assigned sex at birth; (2) clients reporting identities such as “male” or “transgender male” whose reported sex assigned at birth was “female” were grouped under “transgender men”; (3) clients reporting identities such as “female” or “transgender female” whose reported sex assigned at birth was “male” were grouped under “transgender women.” As such, 39 cases missing gender identity or natal sex were excluded. All individuals reporting gender identities congruent with sex assigned at birth were removed from the current analysis (n=24).
Sexual Orientation
Transgender women were stratified into the following groups: straight, lesbian, or bisexual/pansexual/queer. Transgender men were stratified into the following groups: straight, gay, or bisexual/pansexual/queer. The majority of non-binary participants (69%) identified as pansexual or queer; only 3% of non-binary individuals identified as straight. Therefore, we excluded the gender non-binary participants from this analysis, as stratifying other groups beyond this point resulted in groups too small for useful analysis.
Gender-Affirming Care Needs
Types of gender-affirming care needed were reported in two ways. Clients reported all the types of care in which they were interested at the time of intake as their “reason for call” (i.e., establish primary care, hormone management, surgical services, fertility services, behavioral health, or other health concerns). As part of the transition history section of the interview, clients also reported surgical services for which they were seeking an immediate referral or consultation. This latter item indicated more proximal needs, while the former item captured all potential treatment modalities in which the client was interested, regardless of timeline. For both items, the client could select as many care types as applied. For those interested in gender-affirming surgery, we assessed the type of surgery desired. We compared the proportion of each response by sexual orientation categories listed above and reported mental and physical health histories.
Statistical Analysis
All statistical analysis was performed in Stata v. 13 (College Station, TX). All descriptive numbers with respondent groups less than or equal to 3 were reported as “< 4” to protect patient confidentiality. The Kruskal-Wallis rank sum test and Pearson’s chi-squared test were used for continuous and categorical variables, respectively. All statistical tests were two-sided. All missing or incomplete data were excluded from the analysis. The false discovery rate was calculated to examine statistical significance for multiple comparison tests.16 After adjustments, p-values less than 0.015 were considered statistically significant.
RESULTS
Patient Characteristics
In all, 836 interviews were included in the final analyses: 350 trans women, 263 trans men, and 223 non-binary individuals. The median age (interquartile range, IQR) was 29 (24–41) for trans women, 25 (20–31) for trans men, and 27 (23–31) for non-binary individuals, p<0.01. The majority of trans women and trans men identified as straight (34 and 38%, respectively), whereas the majority (69%) of non-binary individuals identified as pansexual or queer, and 3% identified as straight, p<0.01. In total, 67% of the sample identified as white and 23% of the sample identified as Latino/Hispanic. Trans men and non-binary patients were more likely to have a private insurance than trans women (88% and 91% versus 72%, p<0.01). The majority of patients had insurance card sex incongruent with their current gender (Table 1).
Table 2 shows the type of care desired, surgical, and psychiatric histories of patients. Over half of patients reported the reason for visit to be for primary care, hormone management, and/or surgical services. Overall, 552/836 (66%) of respondents selected multiple reasons for presenting to care—56% of trans women, 74% of trans men, and 73% of non-binary individuals selected multiple reasons. Among respondents who selected one primary reason, surgical care (203/284 or 71%) was the most common (data not shown).
Approximately 1 in 4 patients had already had some type of gender affirming surgery; 503 (60%) reported a previous psychiatric diagnosis; and 142 (17%) had been hospitalized for a psychiatric condition. The prevalence of self-reported HIV seropositivity was 2%. Some notable differences were observed by gender identity. First, the percentage of patients desiring primary care differed by gender identity (64% of non-binary and 61% of trans men compared with 47% of trans women, p<0.01). Twice the percentage of trans women and trans men had a gender affirming surgery in the past as did non-binary individuals (25% and 31% vs 14%, p<0.01). HIV was most common in trans women compared with trans men and non-binary individuals (4% vs 0% and 1%, p<0.01). There were no statistical differences between mental illness histories, hospitalizations, and specific diagnoses. In this sample, only 22% of patients self-reported a diagnosis of gender dysphoria.
Sexual Orientation
Sexual orientation was available in 501/613 (82%) of trans women and trans men. Trans women were split into three groups: straight (n=107), lesbian (n=45), or pansexual/bisexual (n=50). Trans men reported three groups: straight (n=79), gay (n=23), or pansexual/bisexual (n=97). Figure 1 shows the type of gender-affirming care desired stratified by gender and sexual orientation. Again, the majority of all genders and sexual orientation were presenting for primary care, hormone management, and surgical services. However, a significantly greater proportion of straight trans women were seeking surgical services compared to lesbian and pansexual/bisexual trans women (79% versus 67% and 63%, p<0.01). There were no significant differences between sexual orientation among those seeking primary care, fertility services, behavioral health, or other health issues in trans women. There was a significantly greater proportion of gay trans men seeking primary care compared with straight and pansexual/bisexual trans men (65% vs 44% and 57%, p<0.01). Pansexual/bisexual patients were more likely to be seeking services for hormone therapy compared to straight and lesbian/gay trans women and trans men (64% vs 52% and 56% in trans women, p<0.01; 64% vs 53% and 51% in trans men, p<0.01). Lastly, a greater proportion of straight and gay trans men were seeking surgical services compared to pansexual/bisexual trans men (76% and 78% vs 63%, p<0.01). There were no significant differences among trans men seeking fertility services, behavioral health, or other health issues by sexual orientation.
Table 3 shows the surgical needs of trans women and trans men, stratified by sexual orientation, as the proportion who either had or were interested in each specific type of operation. We collapsed categories to show surgical needs in preoperative or postoperative management. Straight trans women were more likely to need surgical services for facial feminization and breast augmentation. Otherwise, there were no significant differences between the types of surgeries and sexual orientation.
DISCUSSION
We report a secondary analysis of intake interviews within our gender health program serving a large, urban population of transgender and non-binary individuals. Overall, this program serves a young population (average age 30.5) and most patients are insured. Sexual orientation varies widely within transgender and non-binary participants. Patients mostly are seeking primary care, hormone management, and surgical services. However, the type of desired gender-affirming care varied by both gender identity and sexual orientation.
The US transgender population is racially diverse and more likely than non-transgender individuals to live below the poverty line.17 Approximately 34% of our patient sample was non-white and 23% identified as Latino/Hispanic. The literature reports a wide variation in the insurance status of transgender individuals, ranging from 28 to 90%.18 Insurance status has been associated with delays in gender-affirming care, and public insurance has been associated with denied coverage claims.19 The majority of our patient intake population is insured, which may represent a group with higher socioeconomic status than the general US transgender population. Trans women were more likely to be on public insurance or have no insurance (28%) compared with trans men (11%) and non-binary individuals (9%). This could be explained by the age differences within our sample, as trans women were the oldest group. As such, trans women in our sample were eligible for Medicare. On the other hand, trans men or non-binary individuals may be more likely be on their parent’s private insurance. Of note, the majority of individuals had incongruent insurance ID card gender (58% for trans women, 64% for trans men, and 99% for non-binary individuals). Documentation of gender can impact insurance approval and access. In the US transgender survey, 71% of respondents did not have an updated gender on their driver’s license.12 Our data highlight the continued need for a non-binary or other option on official documentation, as only one non-binary individual reported an insurance card documentation that read non-binary. Non-binary individuals often have conflicting identification, which poses many challenges regarding access to housing, education, and health services.20 A more inclusive documentation strategy for gender diversity is needed among healthcare providers, legal scholars, and researchers.21 Efforts to standardize sexual orientation and gender identity have begun and are overall well received with disclosure rates more than 70%.22
Trans women in our study represent a slightly older population as the 75th to 100th percentile of age within this group was 41–70. A large portion of trans women (25%) had already undergone some form of gender-affirming surgery before presenting to our clinic, and 67% percent are interested in further surgical care. Breast augmentation is often the first type of gender-affirming surgery in trans women.23 On average, the median time from initiation of hormone therapy to breast augmentation has been reported to be 2 years (IQR 2–4 years).24 Breast augmentation has been associated with improved confidence in social situations, and overall complications are minor.25 The prevalence of HIV was highest among trans women (4% of our sample). Trans women represent one of the highest risk groups for HIV acquisition, especially among straight trans women and sex workers.14, 26 Gender-affirming care may present an opportunity for tailored approaches to HIV prevention and treatment.27
Trans men in our study were overall a younger group and thus over two-thirds presented for hormone management. About one-third had already had some form of gender-affirming surgery at presentation. Chest reconstruction was the most commonly cited previous surgery and was the type of surgery patients were most interested in. Chest reconstruction has been associated with improved body image and mental well-being.28 A relatively minor percentage of patients have had or desired phalloplasty/metoidioplasty (<10% of our sample). Motivations for phalloplasty/metoidioplasty include affirming one’s identity, enabling sexual intercourse, and voiding while standing.29 However, urethral complications are high (approximately 30–32%) and risk of neophallus loss is substantial (3–7%).30 Continued research is needed regarding shared decision-making for surgical options in trans men. A large proportion of patients presenting to our gender health clinic identify as non-binary. Within this group, sexual orientation also appears to be expansive with approximately 70% identifying as queer/pansexual. Overall, the majority of these individuals (64%) seek a place for primary care. A growing body of literature indicates that gender-diverse individuals experience discrimination in health settings and are often misunderstood by clinicians.31 In our experience, these patients need a healthcare setting that fosters acceptance and a safe, judgment-free space. As in other reports, the majority of our patients identifying as non-binary were assigned female at birth (n=157/223 or 70%).32 In our program, non-binary individuals were less likely to have already undergone gender-affirming surgery, but over half of patients were interested in hormone management (63%) and surgical services (57%). Young non-binary patients are less likely to report being on hormones but do experience barriers to accessing hormone therapy when needed.32 Ideal patient-centered outcomes for gender-affirming care need to be defined within this population, an area of active exploration.
Sexual orientation is highly variable within gender-diverse individuals. While the absolute differences between groups may not be clinically significant, some notable findings are worthy of discussion. First, straight trans women are significantly more likely to present for surgical services. In particular, straight trans women are especially interested in facial feminization and breast augmentation. The relationship between sexual attraction and type of surgery desired requires further research. Second, gay trans men are seeking a safe place for primary care. Gay trans men may have a variety of primary care needs, which may be unfamiliar to most providers. For instance, gay trans men may present for family planning, cervical cancer screening, or STD/HIV prevention or treatment, which require a particular sensitivity to address in this population. Third, similar sexual orientation labels used in cisgender research may not apply directly toward transgender individuals.33 For example, we had 4 transgender women who identified as gay, and 4 transgender men who identified as lesbian. Others have proposed using terms such as androphilic or gynephilic to best capture sexual attraction.34 Regardless, various aspects of gender-affirming care may be motivated by sexual attraction. Asking about sexual attraction and goals for sexual function is one essential element of care for providers providing gender-affirming care and allows for informed medical decisions.
In the National Transgender Discrimination Survey, a staggering 41% of respondents reported a previous suicide attempt.19 Sixty percent of our participants reported a psychiatric diagnosis, and 17% reported a previous psychiatric hospitalization. A minority (15%) stated they were seeking behavioral health treatment within our gender health program, although 71% had previous mental health treatment in the past elsewhere. According to the guidelines from the World Professional Association for Transgender Health (WPATH), before surgery is recommended, all mental health concerns must be “reasonably controlled.”35 For patients with complex mental health conditions, collaboration and rapport with mental health specialists help guide medical and surgical decision-making, especially for irreversible operations. We believe that housing a program with an interdisciplinary team of providers allows for a more comprehensive treatment plan for all patients.
This study must be considered in light of its limitations. All data are from patient intakes and do not represent in-person patients seen in our program. Most responders in this analysis have insurance and may represent a higher socioeconomic class. This is a reflection of the insurance accepted at our academic institution. All diagnoses are self-reported. The analysis was exploratory and is subject to false positives. To control for this possibility, we adjusted our p-value thresholds as indicated in the methods. We did not perform a multivariable analysis and thus residual confounding cannot be excluded. This was a secondary analysis of data not intended directly for this analysis. Recall bias and social desirability bias could impact the results. Despite these limitations, we present a contemporary needs assessment of a large population of urban transgender and non-binary individuals.
CONCLUSION
Individuals contacting our gender health program to establish care were diverse in sexual orientation and gender-affirming care needs. Care needs varied with both gender and sexual orientation identity, but primary care, hormone management, and surgical services were high priorities across groups. Providers of gender-affirming care should assess sexual orientation and detailed treatment priorities, as trans and gender-diverse populations are not uniform in their treatment needs or goals.
References
Baker KE. Findings from the behavioral risk factor surveillance system on health-related quality of life among US transgender adults, 2014-2017. JAMA Internal Med. 2019;179(8):1141-1144.
Streed Jr CG, McCarthy EP, Haas JS. Self-reported physical and mental health of gender nonconforming transgender adults in the United States. LGBT Health. 2018;5(7):443-448.
Streed CG, Davis JA. Improving clinical education and training on sexual and gender minority health. Curr Sex Health Rep. 2018;10(4):273-280.
Barrett J. Gender dysphoria: assessment and management for non-specialists. BMJ. 2017;357:j2866.
Cheung AS, Ooi O, Leemaqz S, et al. Sociodemographic and clinical characteristics of transgender adults in Australia. Transgend Health. 2018;3(1):229-238.
Klein P, Narasimhan S, Safer JD. The Boston Medical Center experience: an achievable model for the delivery of transgender medical care at an academic medical center. Transgend Health. 2018;3(1):136-140.
Davies A, Bouman WP, Richards C, et al. Patient satisfaction with gender identity clinic services in the United Kingdom. Sex Relatsh Ther. 2013;28(4):400-418.
Allen LR, Watson LB, Egan AM, Moser CN. Well-being and suicidality among transgender youth after gender-affirming hormones. Clin Pract Pediatr Psychol. 2019;7(3):302.
Van De Grift TC, Elaut E, Cerwenka SC, et al. Effects of medical interventions on gender dysphoria and body image: a follow-up study. Psychosom Med. 2017;79(7):815.
da Silva DC, Schwarz K, Fontanari AMV, et al. WHOQOL-100 before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. J Sex Med. 2016;13(6):988-993.
Kuper LE, Nussbaum R, Mustanski B. Exploring the diversity of gender and sexual orientation identities in an online sample of transgender individuals. J Sex Res. 2012;49(2-3):244-254.
James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi MA. The report of the 2015 US transgender survey 2016.
Deutsch MB, Reisner SL, Peitzmeier S, Potter J, Pardee D, Hughto JM. Recent penile sexual contact is associated with an increased odds of high-risk cervical human papillomavirus infection in transgender men. Sex Transm Dis. 2020;47(1):48-53.
Gaither TW, Awad MA, Osterberg EC, Romero A, Bowers ML, Breyer BN. Impact of sexual orientation identity on medical morbidities in male-to-female transgender patients. LGBT Health. 2017;4(1):11-16.
Spielmann J, Stern C. Gender transition shapes perceived sexual orientation. Self Identity. 2019;1-15.
Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67(8):850-857.
Crissman HP, Berger MB, Graham LF, Dalton VK. Transgender demographics: a household probability sample of US adults, 2014. Am J Public Health. 2017;107(2):213-215.
Edmiston EK, Donald CA, Sattler AR, Peebles JK, Ehrenfeld JM, Eckstrand KL. Opportunities and gaps in primary care preventative health services for transgender patients: a systematic review. Transgend Health. 2016;1(1):216-230.
Grant JM, Motter LA, Tanis J. Injustice at every turn: a report of the national transgender discrimination survey. 2011.
Elias N, Colvin R. A third option: understanding and assessing non-binary gender policies in the United States. Administr Theory Praxis. 2020;42(2):191-211.
Streed CG, Grasso C, Reisner SL, Mayer KH. Sexual orientation and gender identity data collection: clinical and public health importance. Am J Public Health. 2020;110(7):991-993.
Grasso C, Goldhammer H, Funk D, et al. Required sexual orientation and gender identity reporting by US health centers: First-year data. Am J Public Health. 2019;109(8):1111-1118.
Wilson EC, Chen Y-H, Arayasirikul S, Wenzel C, Raymond HF. Connecting the dots: examining transgender women’s utilization of transition-related medical care and associations with mental health, substance use, and HIV. J Urban Health. 2015;92(1):182-192.
de Blok CJ, Staphorsius AS, Wiepjes CM, Smit JM, Nanayakkara PW, den Heijer M. Frequency, determinants, and satisfaction of breast augmentation in trans women receiving hormone treatment. J Sex Med. 2020;17(2):342-348.
Coon D, Lee E, Fischer B, Darrach H, Landford WN. Breast augmentation in the transfemale patient: comprehensive principles for planning and obtaining ideal results. Plast Reconstr Surg. 2020;145(6):1343-1353.
Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109(1):e1-e8.
Radix A, Sevelius J, Deutsch MB. Transgender women, hormonal therapy and HIV treatment: a comprehensive review of the literature and recommendations for best practices. J Int AIDS Soc. 2016;19:20810.
van de Grift TC, Elfering L, Greijdanus M, et al. Subcutaneous mastectomy improves satisfaction with body and psychosocial function in trans men: findings of a cross-sectional study using the BODY-Q chest module. Plast Reconstr Surg. 2018;142(5):1125.
van de Grift TC, Pigot GL, Boudhan S, et al. A longitudinal study of motivations before and psychosexual outcomes after genital gender-confirming surgery in transmen. J Sex Med. 2017;14(12):1621-1628.
Ascha M, Massie JP, Morrison SD, Crane CN, Chen ML. Outcomes of single stage phalloplasty by pedicled anterolateral thigh flap versus radial forearm free flap in gender confirming surgery. J Urol. 2018;199(1):206-214.
Goldhammer H, Malina S, Keuroghlian AS. Communicating with patients who have nonbinary gender identities. Ann Fam Med. 2018;16(6):559-562.
Clark BA, Veale JF, Townsend M, Frohard-Dourlent H, Saewyc E. Non-binary youth: access to gender-affirming primary health care. Int J Transgend. 2018;19(2):158-169.
Galupo MP, Henise SB, Mercer NL. “The labels don’t work very well”: transgender individuals’ conceptualizations of sexual orientation and sexual identity. Int J Transgend. 2016;17(2):93-104.
Petterson LJ, Dixson BJ, Little AC, Vasey PL. Viewing time and self-report measures of sexual attraction in Samoan cisgender and transgender androphilic males. Arch Sex Behav. 2018;47(8):2427-2434.
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, 7th Version. WPATH, World Professional Association for Transgender Health; 2012. 2019.
Acknowledgements
We would like to acknowledge our patients for sharing their stories with us.
Funding
All sources of funds supporting the completion of this manuscript are under the auspices of the University of California Los Angeles.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations
none
Supplementary Information
ESM 1
(PDF 26 kb)
Rights and permissions
About this article
Cite this article
Gaither, T.W., Williams, K., Mann, C. et al. Initial Clinical Needs Among Transgender and Non-binary Individuals in a Large, Urban Gender Health Program. J GEN INTERN MED 37, 110–116 (2022). https://doi.org/10.1007/s11606-021-06791-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06791-9




