Abstract
Background
Food insecurity, limited or uncertain access to enough food for an active, healthy life, affected over 37 million Americans in 2018. Food insecurity is likely to be associated with worse health-related quality of life (HRQoL), but this association has not been measured with validated instruments in nationally representative samples. Given growing interest understanding food insecurity’s role in health outcomes, it would be useful to learn what HRQoL measures best capture the experience of those with food insecurity.
Objective
To determine the association between food insecurity and several validated HRQoL instruments in US adults.
Design
Cross-sectional.
Participants
US adults (age ≥ 18), weighted to be nationally representative.
Main Measures
Food insecurity was assessed with three items derived from the USDA Household Food Security Survey Module. HRQoL was assessed using PROMIS-Preference (PROPr), which contains 7 PROMIS domains, self-rated health (SRH), Euroqol-5D-5L (EQ-5D), Health Utilities Index (HUI), and Short Form-6D (SF-6D).
Key Results
In December 2017, 4142 individuals completed at least part of the survey (31% response rate), of whom 4060 (98.0%) reported food security information. Of survey respondents, 51.7% were women, 12.5% self-identified as black, 15.8% were Hispanic, and 11.0% did not have a high school diploma. 14.1% of respondents reported food insecurity. In adjusted analyses, food insecurity was associated with worse HRQoL across all instruments and PROMIS domains (p < .0001 for all). The magnitude of the difference between food-insecure and food-secure participants was largest with the SF-6D, EQ-5D, and PROPr; among individual PROMIS domain scores, the largest difference was for ability to participate in social roles.
Conclusions
Food insecurity is strongly associated with worse HRQoL, with differences between food-secure and food-insecure individuals best measured using the SF-6D, EQ-5D, and PROPr. Future work should develop a specific instrument to measure changes in HRQoL in food insecurity interventions.
Similar content being viewed by others
Food insecurity, limited or uncertain access to enough food for an active, healthy life, affected 11.1% of American households in 2018, or over 37 million Americans.1 Food insecurity is strongly associated with poor health, including increased prevalence of diabetes mellitus, hypertension, coronary heart disease, chronic kidney disease, and depression.2,3,4,5,6,7,8 Food insecurity is also associated with more emergency department visits, more inpatient hospitalizations, and higher healthcare costs.9,10,11,12,13,14 For these reasons, it is likely that food insecurity is associated with lower health-related quality of life (HRQoL).
Food insecurity is a key target for interventions that seek to address health-related social needs to improve health.15,16,17 Common food insecurity interventions include clinic-based screening followed by referral to community food resources (e.g., food pantries), food subsidies, and medically tailored meal delivery programs.18,19,20,21,22,23,24,25 Typically, these programs are evaluated based on their ability to improve disease-specific biomarkers (e.g., hemoglobin A1c for individuals with diabetes), or healthcare utilization (e.g., emergency department visits). However, evaluation of these interventions should include effects on patient-centered outcomes, such as HRQoL.17 In the long-run, understanding which instruments most effectively capture any impact of food insecurity on HRQoL will inform the design and evaluation of food insecurity interventions.
As an initial step towards this goal, it is important to understand how different HRQoL measures are associated with food insecurity, as prior studies have not examined this association with nationally representative data across several validated instruments. Different instruments may each query different HRQoL domains. Therefore, comparing the relationship between food insecurity and HRQoL detected by each instrument will provide useful information for investigators (e.g., which instruments detect larger magnitudes of difference and have lower levels of variability). Furthermore, better understanding the variation across instruments may suggest specific pathways whereby food insecurity influences quality of life. To help fill this literature gap, we sought to determine the associations between food insecurity and several validated HRQoL instruments.
METHODS
Participants and Study Setting
Data used in this study were collected from NORC’s AmeriSpeak Panel, a general population sample of non-institutionalized US adults (age ≥ 18 years) designed to represent 97% of the US population.26 AmeriSpeak uses in-person recruitment to help overcome issues with online-only recruitment. AmeriSpeak participants were invited using sampling strata based on age, race/Hispanic ethnicity, education, and gender. This survey was offered in English and Spanish, and participants could choose to complete it either online or by telephone. NORC provided demographic information about the sample and the sampling weights necessary to make nationally representative estimates, accounting for non-response. IRB approval was obtained from the University of Pittsburgh.
Food Insecurity
Food insecurity was assessed based on responses to three food insecurity items derived from the USDA Household Food Security Survey Module.27 The items used asked how often, in the last 12 months, the respondent or people in the respondent’s household (1) worried whether your food would run out before you had money to buy more; (2) the food that you bought did not last, and you didn’t have enough money to get more; or (3) you couldn’t afford to eat balanced meals. Response options were “Always,” “Usually,” “Sometimes,” “Rarely,” and “Never.” Participants who responded “Always” or “Usually” to any of these questions were categorized as food insecure, with the remainder of respondents being categorized as food secure.
Health-Related Quality of Life Measures
We used several previously validated patient-reported HRQoL measures. Our goal was to assess the relationship between food insecurity and a wide variety of instruments in order to capture subtleties in the relationship between food insecurity and specific instruments that measure HRQoL.
PROMIS Domains
This study measured 7 adult PROMIS domains28: Cognitive Function v2.0, Depression v1.0, Fatigue v1.0, Pain Interference v1.0, Physical Function v2.0, Sleep Disturbance v2.0, and Ability to Participate in Social Roles and Activities v2.0. The PROMIS questions refer to the respondent’s own health “in the past 7 days” and have 5 response options. This study collected 2 questions per PROMIS domain and responses were scored for each individual domain using the Assessment Center Scoring Service with default settings. PROMIS domains are constructed such that the US population mean is 50 with a standard deviation of 10. Higher scores indicate more of the construct; higher scores on function scales indicate more function (i.e., better cognitive function, physical function, and social roles) while higher scores on symptom scales indicate more of a symptom (i.e., worse depression, fatigue, pain interference, sleep disturbance).
PROMIS-Preference
PROMIS-Preference (PROPr) is based on levels of functioning for the 7 PROMIS domains collected in this study. The PROPr scoring algorithm was developed from standard gamble valuations in a US sample. Each domain was described using 2 items to create a unidimensional valuation (e.g., values over a range of depression). The 7 domains were then combined using multi-attribute utility theory to give a single score that represents average health preferences in the USA.29,30,31 Possible PROPr scores range from − .022 (worst) to 1.0 (best).
Self-Rated Health
The self-rated health (SRH) item was, “In general, my health is: excellent, very good, good, fair, poor.”32
Euroqol-5D-5L
Euroqol-5D-5L (EQ-5D) descriptive system has 5 domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and this study used the EQ-5D-5L version with 5 response options per domain.33 The EQ-5D-5L questions refer to “your health today.” We scored the EQ-5D-5L using the time trade-off value set from US adults.34 Possible scores range from − .699 (worst) to 1.0 (best).
Short Form-6D
The Short Form-6D (SF-6D) scoring algorithm uses 7 questions from the Short Form-12 (SF-12) that were evaluated using the standard gamble technique in a representative sample of the UK population.35 Six questions reference “the last 4 weeks” and cover 5 domains (role limitations, pain, vitality, social functioning, and mental health) and 1 question references a “typical day” to cover physical function. Possible SF-6D scores range from .345 (worst) to 1.0 (best).
Health Utilities Index
The self-administered Health Utilities Index (HUI) questionnaire allows scoring of both Mark 2 and Mark 3.36,37 The HUI Mark 2 defines health status on 6 attributes (sensation, mobility, emotion, cognition, self-care, and pain). The HUI Mark 3 defines health on 8 attributes (vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain). HUI questions refer to “your level of ability or disability during the past week.” Scoring algorithms for both HUI Mark 2 and HUI Mark 3 were derived from standard gamble assessments made by adults in community samples in Hamilton, Ontario. HUI Mark 2 scores range from − .03 (worst) to 1.0 (best); HUI Mark 3 scores range from − .36 (worst) to 1.0 (best).
All respondents were asked PROMIS and SRH questions. Respondents were randomly assigned to receive either the EQ-5D-5L and SF-12 or the HUI, to reduce respondent burden and repetitive questions. The minimally important difference for the EQ-5D-5L, SF-12, HUI, or PROPr is generally between .03 and .05.38 We refer to scores on EQ-5D-5L, SF-12, HUI, PROPr, and SRH as “summary scores” and scores on individual PROMIS domains as “domain scores.” All HRQoL measures included domains of physical function, pain, and mood. However, each has a different emphasis beyond this common basis. For example, HUI does not include questions about usual activities or role activities, but does include cognitive function. The EQ-5D and SF-6D include questions about activities and roles but do not include questions about cognitive function. If a key mechanism by which food insecurity influences HRQoL is cognitive function, we would expect the HUI instruments and PROPr to detect greater differences than EQ-5D and SF-6D. Conversely, if a key mechanism is social roles and activities, we would expect the EQ-5D, SF-6D, and PROPr to detect greater differences than HUI.
Covariates and Other Data
We collected information on several factors that may confound the relationship between food insecurity and HRQoL. These were age (categorized as 18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75+), gender, race (categorized as white only, black only, other), ethnicity (categorized as Hispanic versus non-Hispanic), household income (categorized as < $20,000, $20,000 to $40,000, $40,000 to $60,000, $60,000 to $100,000, > $100,000), educational attainment (categorized as no high school diploma, high school graduate or equivalent, some college, bachelors or above), health insurance (categorized as uninsured or single service, private, Medicare, Medicaid/CHIP/State plan, other government), whether the participant lived alone, and region of residence (categorized as New England, Mid-Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain, Pacific).
In order to assess relationships between food insecurity and HRQoL in specific clinical populations, we also assessed subgroups that self-reported: atherosclerotic cardiovascular disease, depression, diabetes mellitus, overweight (body mass index [BMI] 25 to 30 kg/m2), and obesity (BMI > 30 kg/m2).
Statistical Analyses
We first conducted descriptive statistics. We then fit a series of regression models with a goal of determining the association between food insecurity and HRQoL measures. For ease of coefficient interpretability, we fit linear models (except for self-reported health status, where we fit a cumulative logistic model), adjusting for age, gender, race/ethnicity, income, education, health insurance, whether the participant lived alone, and region of residence. We chose not to adjust for chronic conditions (e.g., diabetes) because of the association between food insecurity and these conditions2,4,8, which suggests that chronic conditions may be mediators of the relationship, if any, between food insecurity and HRQoL. Instead, we fit similar models in subsamples stratified by self-report of atherosclerotic cardiovascular disease, depression, diabetes mellitus, overweight, and obesity. Participants who reported more than one condition were included in analyses for each of the conditions they reported. To determine whether food insecurity was associated with differences in outcomes, compared with those who were food secure, we conducted F-tests on the model regression coefficient contrasting food-secure and food-insecure status, and constructed 95% confidence intervals. To compare the magnitude of the association between food insecurity and a given HRQoL score across all the HRQoL instruments used in the study, which have different scales, we calculated partial omega-square statistics.39,40 These effectively standardize the scores, and can be interpreted as the amount of variation in the outcome explained by food insecurity, after accounting for the variation explained by other variables in the model. Omega-square statistics range from 0 to 1, with greater statistics indicating that more variation in the outcome is explained by food security status. Thus, a greater omega-square statistic suggests that a given instrument may be better attuned to the ways in which food security status is related to HRQoL.
All analyses were conducted in SAS version 9.4 (Cary, NC), and analyses included sampling weights so that estimates would reflect a nationally representative sample. The sampling design is not stratified, so clustering adjustment for standard errors is not needed. A p value < .05 indicated statistical significance. The analysis testing the relationship between food insecurity and the PROPr score was considered the primary analysis for this study, with additional analyses considered exploratory.
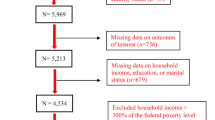
RESULTS
In December 2017, 13371 individuals were invited from the panel and 4142 individuals completed at least part of the survey (31%), of whom 4060 (98.0%) reported food security information (survey weights accounted for non-response). Of survey respondents, 51.7% were women, 12.5% self-identified as black, 15.8% were Hispanic, and 11.0% did not have a high school diploma. Additional demographic information is presented in Table 1. 14.1% of respondents reported food insecurity. Those who were food insecure, compared with food secure, were younger (p < .0001), more likely to be racial/ethnic minorities (p < .0001) and had lower income (p < .0001).
In unadjusted analyses (Table 2), food insecurity was associated with worse self-reported health status (p < .0001), lower HRQoL for all summary scores (p < .0001 for all), and worse symptomatology and decreased function for all PROMIS domains (p < .0001 for all).
In analyses adjusted for age, gender, race/ethnicity, income, education, health insurance, whether the participant lived alone, and region of residence, food insecurity remained associated with lower HRQoL summary scores across all summary scores (p < .0001 for all) and worse PROMIS scores across all domains (p < .0001 for all) (Table 3). Adjusted differences ranged from − .11 to − .21 across summary scores.
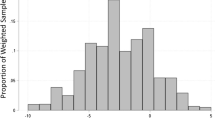
Food insecurity typically accounted for approximately 4 to 9% of the variation in scores across HRQoL instruments, adjusted for the other covariates. The magnitude of the difference between food-insecure and food-secure participants was largest with the SF-6D instrument (partial omega-square .091, 95% CI .069 to .116; Fig. 1), but the partial omega-square for the EQ-5D and PROPr fell within this confidence interval. With regard to PROMIS domain scores, the magnitude of the difference between food-insecure and food-secure participants was greatest for ability to participate in social roles (partial omega-square .067, 95% CI .053 to .082; Fig. 2). Food insecurity consistently accounted for a large share of the variation in HRQoL, relative to other covariates (eTable 1).
Patterns seen in the overall sample typically held when examining subgroups with specific chronic conditions—HRQoL summary scores and PROMIS domain scores were statistically significantly worse for those experiencing food insecurity in all cases but one (EQ-5D score in those with diabetes, where the point estimate was worse but the difference was not statistically significant) (eTables 2–6).
DISCUSSION
In this nationally representative sample, food insecurity was strongly associated with worse HRQoL summary scores and PROMIS domain scores. The SF-6D, EQ-5D, and PROPr seemed particularly attuned to detecting differences in HRQoL by food security status. PROPr has the added benefit of also providing PROMIS domain scores. The relationship between HRQoL and food insecurity within subgroups defined by comorbidities was similar to that seen in the overall sample.
The differences in scores associated with food insecurity are both statistically significant and large. The minimally important difference of health utility summary scores is generally between .03 and .0538; differences associated with food insecurity were .11 to .21. For context, in other US nationally representative studies using the same scores, differences associated with diabetes were .04 to .09, differences associated with COPD were .11 to .22, and differences associated with angina were .07 to .16.41 Likewise, the minimally important difference of PROMIS domain scores is generally between 3 and 5; the smallest difference in these analyses was 3.8 (sleep disturbance) and the largest was 6.3 (social roles).
The findings of this study are consistent with and extend those of prior studies that typically found food insecurity is associated with lower HRQoL.42,43,44,45,46 However, these studies were not nationally representative, focused on specific subsets of the population, and/or used only a single HRQoL instrument—often the “Healthy Days” tool.47 This study adds nationally representative data with a variety of validated, and commonly used, HRQoL instruments. Despite widespread use, neither “Healthy Days” nor single item self-rated health has an established minimally important difference. The difficulty comparing “Healthy Days” and single item self-rated health to other HRQoL scores, along with difficulty in establishing a meaningful change, illustrates limitations of using these as outcomes.
As clinical and public health evaluations shift their focus to person-centered outcomes, the use of linear, validated, preference-based summary scores of HRQoL has advantages for both modeling flexibility and interpretability. First, they provide a single score that combines multiple health domains. This provides a standardized way to compare interventions with effects on different domains of health (e.g., comparing one intervention that improves depression to another intervention that improves pain) or with differential effects on different domains of health (e.g., comparing one intervention that moderately improves depressive symptoms but mildly worsens physical functioning to another intervention that mildly improves depression with no change in physical functioning). Second, generic, societal preference-based scores are appropriate for use in cost-effectiveness analyses. Third, their widespread use facilitates comparison across different types of interventions. Of this group, PROPr is unique because it is constructed from PROMIS domains. This means that in addition to having a summary score, investigators can explore the effects of interventions on individual domains, acknowledging that societal weights do not necessarily represent individual weights.
Prior qualitative studies have suggested that food insecurity affects many aspects of individuals’ lives, even ones that may not seem directly related to food or diet.48,49 Examples of this include individuals reporting that fulfilling social roles can be difficult when worrying about food.48,49 This study helps quantify some of those associations. For example, we found a strong association between food insecurity and the social role domain within PROPr. Furthermore, we found that HRQoL scales, like PROPr and SF-6D, that query aspects of social roles detected differences in HRQoL with larger point estimates than scales that did not, like HUI.
This study has implications for future work on the relationship between food insecurity and HRQoL. Through mechanisms such as PROMIS, there are now a wide variety of health domains available for use. PROPr uses 7 domains, but there are presently 96 PROMIS domains for adults and 19 for children ages 5–17.50 Future work could determine whether other domains are more attuned to the circumstances faced by those who experience food insecurity than domains used here. Additionally, this study demonstrates inter-individual differences related to food insecurity, but does not address which instrument will be most sensitive to the effects of changing food insecurity (intra-individual change). Such work could aid in the development of a “condition-specific” outcome measure for food insecurity interventions that may comprised available PROMIS domains with or without supplemental questions. Additionally, analyses in other clinical populations, particularly those that include diet as part of condition management, such as chronic kidney disease, should be pursued.
This study should be interpreted in light of several limitations. Though food security questions were derived from USDA Food Security Survey Module, the response options were modified to fit the survey formatting. However, food insecurity prevalence estimated from this study is very similar to the national average reported by the USDA in December 2017 (the study period)1, suggesting that this change did not meaningfully impact food security assessment. The data were cross-sectional, so we cannot determine whether food insecurity caused lower HRQoL, or vice versa. Though we used several common HRQoL instruments, there are of course other HRQoL instruments that were not included. Finally, online panel surveys can be biased with regard to which individuals participate, and we did not have access to data comparing the characteristics of those who did versus did not participate. However, this particular panel uses face-to-face recruitment to help mitigate this concern, and weighting to help account for non-response bias.
In this study using responses from a nationally representative panel of adults, food insecurity was strongly associated with worse HRQoL, both in the overall sample and in subgroups defined by specific comorbidities. Of HRQoL instruments, the SF-6D, EQ-5D, and PROPr were particularly attuned to the specific challenges of those experiencing food insecurity. Improving our ability to measure HRQoL in those who experience food insecurity will enable us to better develop and study interventions that address this important health risk.
References
Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018. Published September 4, 2019. Accessed April 16, 2020. http://www.ers.usda.gov/publications/pub-details/?pubid=94848
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310. doi:https://doi.org/10.3945/jn.109.112573
Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018-1023. doi:https://doi.org/10.1007/s11606-007-0192-6
Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. Cheng X, ed. PLOS ONE. 2017;12(6):e0179172. doi:https://doi.org/10.1371/journal.pone.0179172
Crews DC, Kuczmarski MF, Grubbs V, et al. Effect of food insecurity on chronic kidney disease in lower-income Americans. Am J Nephrol. 2014;39(1):27-35. doi:https://doi.org/10.1159/000357595
Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household Food Insecurity Is Positively Associated with Depression among Low-Income Supplemental Nutrition Assistance Program Participants and Income-Eligible Nonparticipants. J Nutr. 2015;145(3):622-627. doi:https://doi.org/10.3945/jn.114.199414
Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The Relationship Between Food Insecurity and Depression, Diabetes Distress and Medication Adherence Among Low-Income Patients with Poorly-Controlled Diabetes. J Gen Intern Med. 2015;30(10):1476-1480. doi:https://doi.org/10.1007/s11606-015-3351-1
Gundersen C, Ziliak JP. Food Insecurity And Health Outcomes. Health Aff Proj Hope. 2015;34(11):1830-1839. doi:https://doi.org/10.1377/hlthaff.2015.0645
Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265. doi:https://doi.org/10.1001/jamainternmed.2014.6888
Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011-2013. Health Serv Res. Published online June 13, 2017. doi:https://doi.org/10.1111/1475-6773.12730
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
Tarasuk V, Cheng J, Oliveira C de, Dachner N, Gundersen C, Kurdyak P. Association between household food insecurity and annual health care costs. CMAJ. 2015;187(14):E429-E436. doi:https://doi.org/10.1503/cmaj.150234
Berkowitz SA, Basu S, Gundersen C, Seligman HK. State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis. 2019;16:E90. doi:https://doi.org/10.5888/pcd16.180549
Garcia SP, Haddix A, Barnett K. Incremental Health Care Costs Associated With Food Insecurity and Chronic Conditions Among Older Adults. Prev Chronic Dis. 2018;15:E108. doi:https://doi.org/10.5888/pcd15.180058
Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities--Addressing Social Needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. doi:https://doi.org/10.1056/NEJMp1512532
Bibbins-Domingo K. Integrating Social Care Into the Delivery of Health Care. JAMA. Published online September 25, 2019. doi:https://doi.org/10.1001/jama.2019.15603
National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. doi:https://doi.org/10.17226/25467
Schickedanz A, Sharp A, Hu YR, et al. Impact of Social Needs Navigation on Utilization Among High Utilizers in a Large Integrated Health System: a Quasi-experimental Study. J Gen Intern Med. Published online June 21, 2019. doi:https://doi.org/10.1007/s11606-019-05123-2
Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing Unmet Basic Resource Needs as Part of Chronic Cardiometabolic Disease Management. JAMA Intern Med. 2017;177(2):244-252. doi:https://doi.org/10.1001/jamainternmed.2016.7691
Seligman HK, Smith M, Rosenmoss S, Marshall MB, Waxman E. Comprehensive Diabetes Self-Management Support From Food Banks: A Randomized Controlled Trial. Am J Public Health. Published online July 19, 2018:e1-e8. doi:https://doi.org/10.2105/AJPH.2018.304528
Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot. Am J Clin Nutr. 2016;104(2):423-435. doi:https://doi.org/10.3945/ajcn.115.129320
Berkowitz SA, Delahanty LM, Terranova J, et al. Medically Tailored Meal Delivery for Diabetes Patients with Food Insecurity: a Randomized Cross-over Trial. J Gen Intern Med. 2019;34(3):396-404. doi:https://doi.org/10.1007/s11606-018-4716-z
Berkowitz SA, O’Neill J, Sayer E, et al. Health Center-Based Community-Supported Agriculture: An RCT. Am J Prev Med. 2019;57(6S1):S55-S64. doi:https://doi.org/10.1016/j.amepre.2019.07.015
Basu S, Gardner CD, White JS, et al. Effects Of Alternative Food Voucher Delivery Strategies On Nutrition Among Low-Income Adults. Health Aff Proj Hope. 2019;38(4):577-584. doi:https://doi.org/10.1377/hlthaff.2018.05405
Choi SE, Seligman H, Basu S. Cost Effectiveness of Subsidizing Fruit and Vegetable Purchases Through the Supplemental Nutrition Assistance Program. Am J Prev Med. 2017;52(5):e147-e155. doi:https://doi.org/10.1016/j.amepre.2016.12.013
Panel Design | AmeriSpeak. Accessed April 16, 2020. http://amerispeak.norc.org/about-amerispeak/Pages/Panel-Design.aspx
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Published online March 2000. Accessed September 17, 2018. https://fns-prod.azureedge.net/sites/default/files/FSGuide.pdf
Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179-1194. doi:https://doi.org/10.1016/j.jclinepi.2010.04.011
Hanmer J, Cella D, Feeny D, et al. Selection of key health domains from PROMIS® for a generic preference-based scoring system. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2017;26(12):3377-3385. doi:https://doi.org/10.1007/s11136-017-1686-2
Dewitt B, Feeny D, Fischhoff B, et al. Estimation of a Preference-Based Summary Score for the Patient-Reported Outcomes Measurement Information System: The PROMIS®-Preference (PROPr) Scoring System. Med Decis Mak Int J Soc Med Decis Mak. 2018;38(6):683-698. doi:https://doi.org/10.1177/0272989X18776637
Dewitt B, Jalal H, Hanmer J. Computing PROPr Utility Scores for PROMIS® Profile Instruments. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2020;23(3):370-378. doi:https://doi.org/10.1016/j.jval.2019.09.2752
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483.
Brooks R, Rabin R, Charro F de, eds. The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective: Evidence from the EuroQol BIOMED Research Programme. Springer Netherlands; 2003. Accessed May 7, 2020. https://www.springer.com/gp/book/9781402012143
Pickard AS, Law EH, Jiang R, et al. United States Valuation of EQ-5D-5L Health States Using an International Protocol. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2019;22(8):931-941. doi:https://doi.org/10.1016/j.jval.2019.02.009
Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42(9):851-859. doi:https://doi.org/10.1097/01.mlr.0000135827.18610.0d
Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40(2):113-128. doi:https://doi.org/10.1097/00005650-200202000-00006
Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi:https://doi.org/10.1186/1477-7525-1-54
Luo N, Johnson JA, Coons SJ. Using Instrument-Defined Health State Transitions to Estimate Minimally Important Differences for Four Preference-Based Health-Related Quality of Life Instruments. Med Care. 2010;48(4):365–371. doi:https://doi.org/10.1097/MLR.0b013e3181c162a2
Omega Squared. In: Encyclopedia of Research Design. SAGE Publications, Inc.; 2010. doi:https://doi.org/10.4135/9781412961288.n289
Olejnik S, Algina J. Generalized eta and omega squared statistics: measures of effect size for some common research designs. Psychol Methods. 2003;8(4):434-447. doi:https://doi.org/10.1037/1082-989X.8.4.434
Hanmer J, Dewitt B, Yu L, et al. Cross-sectional validation of the PROMIS-Preference scoring system. PloS One. 2018;13(7):e0201093. doi:https://doi.org/10.1371/journal.pone.0201093
Sharkey JR, Johnson CM, Dean WR. Relationship of household food insecurity to health-related quality of life in a large sample of rural and urban women. Women Health. 2011;51(5):442-460. doi:https://doi.org/10.1080/03630242.2011.584367
Gany F, Leng J, Ramirez J, et al. Health-Related Quality of Life of Food-Insecure Ethnic Minority Patients With Cancer. J Oncol Pract. 2015;11(5):396-402. doi:https://doi.org/10.1200/JOP.2015.003962
Frongillo EA, Nguyen HT, Smith MD, Coleman-Jensen A. Food Insecurity Is Associated with Subjective Well-Being among Individuals from 138 Countries in the 2014 Gallup World Poll. J Nutr. 2017;147(4):680-687. doi:https://doi.org/10.3945/jn.116.243642
Sok P, Gardner S, Bekele T, et al. Unmet basic needs negatively affect health-related quality of life in people aging with HIV: results from the Positive Spaces, Healthy Places study. BMC Public Health. 2018;18(1):644. doi:https://doi.org/10.1186/s12889-018-5391-z
Kihlström L, Burris M, Dobbins J, et al. Food Insecurity and Health-Related Quality of Life: A Cross-Sectional Analysis of Older Adults in Florida, U.S. Ecol Food Nutr. 2019;58(1):45-65. doi:https://doi.org/10.1080/03670244.2018.1559160
Healthy Days Methods and Measures | HRQOL | CDC. Published November 5, 2018. Accessed June 3, 2020. https://www.cdc.gov/hrqol/methods.htm
Berkowitz SA, Shahid NN, Terranova J, et al. “I was able to eat what I am supposed to eat”-- patient reflections on a medically-tailored meal intervention: a qualitative analysis. BMC Endocr Disord. 2020;20(1):10. doi:https://doi.org/10.1186/s12902-020-0491-z
Hege A, Ball L, Christiana RW, et al. Social Determinants of Health and the Effects on Quality of Life and Well-being in 2 Rural Appalachia Communities: The Community Members’ Perspective and Implications for Health Disparities. Fam Community Health. 2018;41(4):244-254. doi:https://doi.org/10.1097/FCH.0000000000000201
PROMIS Measures. Accessed May 8, 2020. http://www.healthmeasures.net/search-view-measures?task=Search.search
Funding
Funding for JH’s role on the study was provided by the Robert Wood Johnson Foundation Award Number 74695. Funding for SAB’s role on the study was provided by the National Institute of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number K23DK109200. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Robert Wood Johnson Foundation.
Author information
Authors and Affiliations
Contributions
JH and SAB conceived the study and drafted the manuscript. DAD contributed to interpretation of the data and revised the manuscript critically for important intellectual content. All authors give approval of the manuscript version to be submitted.
Corresponding author
Ethics declarations
Conflict of Interest
JH, DAD, and SAB have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Janel Hanmer and Seth A. Berkowitz contributed equally to first authorship.
Prior Presentation
None.
Supplementary Information
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Hanmer, J., DeWalt, D.A. & Berkowitz, S.A. Association between Food Insecurity and Health-Related Quality of Life: a Nationally Representative Survey. J GEN INTERN MED 36, 1638–1647 (2021). https://doi.org/10.1007/s11606-020-06492-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-06492-9