Abstract
Background
Black individuals with type 2 diabetes suffer disproportionate morbidity and mortality relative to whites with type 2 diabetes, irrespective of health insurance coverage.
Objective
Examine the impact of a primary care–embedded clinical pharmacist–led intervention (UCMyRx) on cardiovascular risk factor control among blacks with type 2 diabetes in a large healthcare system.
Design
We used data extracted from the electronic health records (EHR) system and a difference-in-differences study design with a propensity-matched comparison group to evaluate the impact of UCMyRx on HbA1c and systolic blood pressure (SBP) among black patients with type 2 diabetes, relative to usual care.
Participants
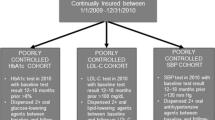
Individuals with type 2 diabetes identified as either black or African American in the EHR that were ≥ 18 years of age that had the following observations during the study window (03/02/2013–12/31/18: (1) HbA1C ≥ 8%, at least once, anywhere between 365 days before and 14 days after the UCMyRx visit and a follow-up HbA1c measure within 120 to 365 days after the visit and/or (2) SBP ≥ 140 mmHg at least once between 365 days before and 14 days after the UCMyRx visit that had a follow-up SBP measure within 120 to 450 days after the visit.
Intervention
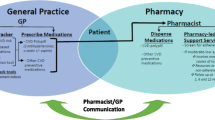
UCMyRx pharmacists review labs and vital signs, perform medication reconciliation, use a standardized survey to assess barriers to medication adherence, and develop tailored interventions to improve medication adherence.
Main Measures
Change in HbA1c and change in SBP from before to after the first UCMyRx visit.
Key Results
Having at least one visit with a UCMyRx clinical pharmacist was associated with a significant reduction in HbA1c (− 0.4%, p value = .01); however, there was no significant impact on SBP (− .051 mmHg, p value = 0.74).
Conclusions
The UCMyRx intervention is a useful strategy for improving HbA1c control among blacks with type 2 diabetes.
Similar content being viewed by others
INTRODUCTION
Type 2 diabetes is an enormous public health problem. In 2017 expenditures associated with diabetes topped 237 billion dollars in direct and 90 billion in indirect costs, respectively.1 Type 2 diabetes disproportionately affects the black population. In particular, blacks have a higher prevalence of diabetes (13.2% vs. 7.6%) and have anywhere from a 50 to 100% greater disease burden from complications such as kidney disease, lower extremity amputations, retinopathy, and cardiovascular disease, relative to non-Hispanic whites.2, 3
A large portion of racial morbidity difference from diabetes can be explained by differences in cardiovascular risk factor control across racial groups.4 Studies have found that even among insured patients with diabetes, relative to non-Hispanic whites, blacks with diabetes are less likely to have HbA1c, LDL, and blood pressure levels that are consistent with guidelines.5, 6 Differences in the quality of care received across racial groups are a key driver of the racial disparities in cardiovascular risk factor control. Studies indicate that even after controlling for access to care, racial/ethnic minorities are less likely than non-Hispanic whites to have annual HbA1c and cholesterol testing.7
Another important factor underlying disparities in risk factor control is medication adherence. Studies have found that among patients with diabetes, blacks are more likely to report not taking medications in accordance with their doctor’s instructions and are more likely to discontinue diabetes medications, relative to non-Hispanic whites.8, 9 The drivers of non-adherence among blacks with diabetes are multifactorial and include reduced health literacy, medication misbeliefs, concerns about medication side effects, and medication costs issues.10,11,12,13
Results from a few small randomized clinical trials suggest that primary care–based pharmacist-led management, a delivery system design intervention that uses clinical pharmacists to address care quality and patient self-management behavior, may be an effective strategy for improving cardiovascular risk factor control among black individuals with diabetes. Rothman et al. found that minorities with Hba1c ≥ 8, randomized to an intervention in which a clinical pharmacist provided patient education, addressed barriers to care, and managed cardiovascular risk factors using algorithms, during monthly visits, had reductions in HbA1c and systolic blood pressure (SBP) of 0.8% and 9 mmHg, respectively, after 12 months.14 Jaber et al. found that after 4 months, black individuals with diabetes, randomized to an intervention in which a clinical pharmacist provided diabetes education, lifestyle modification counseling, as well as instruction in home glucose monitoring and hypoglycemic regimen adjustment, had statistically significant reductions in HbA1c levels, compared with individuals randomized to usual care.15
While small RCTs have shown efficacy of primary care–based pharmacist-led management interventions for improving cardiovascular risk factor control among black individuals with diabetes, no effectiveness studies of this intervention in this population have been done. Individuals participating in RCTs are often more motivated and less sick than the general population. Adherence to intervention protocol is typically much stricter in RCTs than it is in every day practice.16 Consequently, the performance of primary care–embedded pharmacist-led management interventions among black individuals with type 2 diabetes, in a real-world context, remains uncertain. The objective of this study is to evaluate the effectiveness of a primary care–embedded clinical pharmacist–led management intervention, implemented in a large healthcare system, on cardiovascular risk factor control, among black patients with type 2 diabetes.
METHODS
Setting
The University of California Los Angeles (UCLA) is an academic medical center comprised of four hospitals and more than 180 medical practices throughout Southern California.
Data Extraction
The electronic health records (EHR) system was implemented at UCLA in March 2013. We obtained EHR data for all patients in the exposure and usual care groups. The abstracted data included medical encounter types, demographics, diagnoses, vital signs, laboratory test results, prescription medications, and health insurance coverage variables.
Exposure: UCMyRx Visit
In January 2012, UCLA began the UCMyRx initiative. As of October 2018, the program existed in 32 clinics. UCMyRx involves embedding clinical pharmacists trained in motivational interviewing into primary care practices to co-manage complex patients along with their primary care physicians. Individuals can access the UCMyRx program in a number of ways including by physician, clinical care coordinator, or self-referral. Additionally, individuals in the UCLA Diabetes Registry, meeting one or more of the following criteria: (1) a HbA1C ≥ 9%, (2) a SBP ≥ 140 mmHg, (3) an LDL ≥ 130 mg/dL, and (4) on ≥ 5 prescription medications, are contacted to schedule a consultation with a UCMyRx pharmacist. In the initial UCMyRx visit, clinical pharmacists review vital signs and labs, order labs as needed, perform medication reconciliation, assess medication adherence using a standardized survey and, based on the results of the survey, implement an intervention to improve medication adherence (Table 1). For example, survey responses that indicate out-of-pocket costs as a barrier to adherence would prompt the pharmacist to look for less expensive therapeutic options, patient-assistance programs, and generic substitutions. The pharmacist schedules follow-up visits with the patient and supplements the visits with e-mails and phone calls as needed. The results of all assessments and recommendations regarding medication changes are communicated to the primary care physician through the EHR.
The exposure group included adults with any instance of ICD-9/10 diagnosis code for type 2 diabetes, race either black or African American, and ≥ 18 years of age that had at least one face-to-face visit with a UCMyRx clinical pharmacist, during the study window (03/02/2013–12/31/2018). The exposure population for the HbA1c analyses was limited to adults that had HbA1C ≥ 8%, at least once, anywhere between 365 days before and 14 days after the visit and a follow-up HbA1c measure within 120 to 365 days of the visit. The SBP population was limited to adults that had SBP ≥ 140 mmHg at least once, between 365 days before and 14 days after the UCMyRx visit that had a follow-up SBP measure within 120 to 450 days after the visit. The index date for the exposure population was the date of the first UCMyRx visit.
Usual Care
The usual care group came from UCLA patients, with any instance of ICD-9/10 diagnosis code for type 2 diabetes, identified in the EHR as black or African American that were ≥ 18 years of age that had at least 2 visits to one or more UCLA primary care clinics, ≥ 2 years apart, during the study window. The population used for the HbA1c analyses was further limited to the population that had HbA1C ≥ 8%, at least once, anywhere between 365 days before and 14 days after a randomly generated index date, between the two primary care visits and a follow-up HbA1c measure within 120 to 365 days of the index date. The SBP population was limited to adults that had SBP ≥ 140 mmHg at least once, between 365 days before and 14 days after the randomly generated index date that had a follow-up SBP measure within 120 to 450 days after the index date. Usual care patients came from clinics both with and without UCMyRx pharmacists; however, they did not have a visit with a UCMyRx pharmacist.
Propensity Score Matching Analysis
Since it is not possible to randomize patients to the UCMyRx program, we use propensity score matching to create comparable cohorts of UCMyRx and usual care patients.17 Logistic regression models were used to generate propensity scores. Variable choices for the propensity scores were informed by the extant literature and included pre-index (HbA1c and SBP levels, age, gender, Charlson Comorbidity Index (CCI), Diabetes Severity Index (DSI)18, serious mental illness (bipolar disorder, schizophrenia, major depression), having seen an endocrinologist (yes/no), number of diabetes medications, total number of prescription medications, and health insurance status (private, Medicare, Medicaid, Medicaid + Medicare)).6, 13, 19 Variables for insulin use, language, neighborhood-level educational status, body mass index, and smoking status were initially included in the propensity score models but they were removed due to the lack of a statistically significant association with treatment status. Each UCMyRx patient was matched to one comparable usual care patient using the nearest neighbor matching method.20 Separate propensity score matching was done for each outcome. Post-matching there were no statistically significant differences between the UCMyRx and usual care groups (Table 2).
Outcomes
Our primary outcomes were pre- to post-index changes in HbA1c and SBP levels. The pre-index HbA1c was the closest value to the index date with a window of 365 days before the index date and 14 days after. The pre-index SBP was the mean of the 3 values closest to the index date with a 365-day window before and a 14-day window after. The post-index HbA1c was the closest value to 180 days after the index date with a window of 120 to 365 days after the index date. The post-index SBP was the mean of the 3 values closest to 365 days after the index date with a 120- to 450-day window after the index date.19
Statistical Analysis
R statistical software was used for all analyses. The unit of analysis was the patient. We calculate descriptive statistics for all variables in the models, across treatment status, using the t test and chi-squared test for continuous and dichotomous/categorical variables, respectively. To evaluate the effect of the UCMyRx program on HbA1c and SBP, we performed difference-in-differences (DID) analyses. The DID study design is well-suited to assess the effects of the UCMyRx intervention given that it is able to remove the influence of other interventions such as a system-wide diabetes care quality improvement initiative, provided both the UCMyRx and usual care groups are exposed to the intervention and both groups are affected by the intervention in the same way. The use of propensity score matching helps ensure that the UCMyRx and usual care groups are balanced on observable factors that may influence how they would respond to a given intervention.21 We used linear mixed effects models that include an indicator for time (post-index vs. pre-index) that was coded as “1” if the observation was from the post-index period and coded “0” otherwise, an indicator for group (UCMyRx vs. usual care) that was coded as “1” if the observation was from the UCMyRx group and coded as “0” otherwise and the interaction between time and group, among our matched samples.22 Specifically, the between-group differences in the change of the outcome variables, post-index, were estimated by the interaction effects. The models also included random effects to take into account data clustering within each pair of matched UCMyRx and usual care patients and data clustering within each patient. The “patient” random effects were nested within the “cluster” random effects.
Sensitivity Analyses
To assess if UCMyRx effects were stronger among individuals with worse cardiovascular risk factor control, we conducted analyses in which we limited our HbA1c and SBP samples to individuals that had HbA1c ≥ 9% and SBP ≥ 150 mmHg, at least once during the pre-index period, respectively. To assess if UCMyRx effect differences observed across populations with more or less controlled risk factors were statistically significant, we repeated analyses with the entire matched sample and included a risk indicator coded as “1” if the patient had worse risk factor control and coded “0” otherwise. A statistically significant interaction between the time, group, and risk indicators would indicate statistically significant differences in UCMyRx effects, across patient populations, with more or less controlled risk factors. To assess the impact of UCMyRx across patients with different levels of comorbidity, we ran analyses stratified by Charlson Comorbidity Index (CCI) tercile. To assess for a dose-response effect of UCMyRx, we ran analyses comparing individuals with face-to-face contacts and total contacts (face-to-face visits, telephone calls, and e-mails) above the median to those with the median or below, by incorporating an interaction between time and an indicator coded as “1” if the number of contacts was above the median and coded “0” otherwise, in a model that was limited to UCMyRx patients.
RESULTS
Patient Characteristics
Our sample sizes for the HbA1c and the SBP outcomes were 169 and 210, respectively. Descriptive statistics for each of our unmatched and matched analytic samples are shown in Table 2 (HbA1c sample) and Table 3 (SBP sample). The pre-index mean HbA1c for the sample used for the HbA1c analysis was 7.7% and the SBP for the sample used for the SBP analysis was 138.5 mmHg.
UCMyRx Characteristics
The mean and standard deviation for face-to-face visits for the HbA1c and SBP groups were 3.8 (5.5) and 3.6 (5.1), respectively. The median and interquartile range for face-to-face visits for both the HbA1c and SBP groups was 2 (1–4). The mean and standard deviation for total contacts (face-to-face visits, telephone, and e-mail) for the HbA1c and SBP groups were 7.1 (11.2) and 6.6 (10.4), respectively. The median and interquartile range for total contacts for both the HbA1c and SBP groups was 3 (2–8).
Post UCMyRx Visit Change in HbA1c and SBP
The results of our adjusted analyses are shown in Table 4. Patients exposed to the UCMyRx intervention experienced a significant − 0.40% (p value = 0.01) decline in HbA1c, relative to usual care patients. The median HbA1c change among UCMyRx patients was − 0.20% and the interquartile range was − 0.20 to − 0.90%. There was also an insignificant negative trend in SBP among UCMyRx-exposed patients (− .051 mmHg (p value = 0.74)).
Sensitivity Analyses
The analysis limited to individuals with HbA1c ≥ 9% shows a UCMyRx effect slightly larger than that observed in the initial analysis (− 0.45%, p value = 0.01 vs. − 0.40%, p value = 0.01); however, this difference in magnitude is not statistically significant (− 0.43, p value = 0.36). There is an insignificant negative trend among the population with SBP ≥ 150 mmHg, at least once during the pre-index period (− 0.50 mmHg, p value = 0.76). In CCI-stratified analyses, we found that the intervention effect on HbA1c is stronger (− 0.79%, p value = 0.00 vs. − 0.40%, p value = 0.01) among the tercile with the lowest comorbidity score (CC1 ≤ 5). UCMyRx effects are not statistically significant in the other terciles (5 ˂ CC1 ≤ 8 = − 0.30%, p value = 0.22; CCI > 8 = − 0.05%, p value = 0.84). We do not find statistically significant effects of the UCMyRx intervention on SBP in any CCI tercile. We found an insignificant trend towards stronger UCMyRx effects among the HbA1c subgroups with more face-to-face visits (− 0.372, p value = 0.065) and total contacts (− 0.369, p value = 0.066), respectively.
DISCUSSION
We conducted the first effectiveness study of a primary care–embedded clinical pharmacist–led intervention in a large healthcare system, among black patients with type 2 diabetes and found a statistically significant 0.4% reduction in HbA1c among the UCMyRx population and no impact on SBP, relative to usual care. We find an even stronger HbA1c effect among individuals with low levels of comorbidity and borderline stronger effects among individuals with more UCMyRx contacts.
A HbA1c reduction of 0.4% is consistent with what some studies have found for continuous glucose monitoring and insulin initiation.23, 24 Economic models have predicted that a 0.4% decrease in HbA1c would significantly reduce microvascular and macrovascular complications among diabetics, over 25 years, taking into account age, gender, risk factors, and pre-existing complications.25, 26 Given that blacks suffer more diabetes-related morbidity and mortality than nearly all other racial/ethnic subgroups, these findings are particularly important.
The effect on HbA1c that we find is roughly 50% of what has been observed in efficacy studies.14 Several factors may account for that. One factor may be that the mean HbA1c in our analytic sample is lower relative to that of other study populations (7.7% vs.11%). 14 We also have an older study population than what has been found in other studies, with a mean age of 63.7, relative to a mean age of 54 and 59 in the Rothman et al. and Jaber et al. studies, respectively.14, 15 Consequently, less stringent HbA1c treatment goals for some older patients may have manifested in a smaller mean HbA1c change associated with the UCMyRx intervention.27 Lastly, relative to other studies, our treatment populations had much less contact with clinical pharmacists. In the Rothman et al. study, the diabetes management team had a median of 45 contacts/care-related activities per patient, relative to 3 in this study for the HbA1c subsample.14
These findings must be interpreted in the context of important study limitations. Our DID analysis with propensity score–matched comparison group will only remove the influence of secular time trends from our UCMyRx effect-estimates if the secular time trends for the UCMyRx and usual care groups are the same.21 Propensity score matching helps to ensure the similarity of secular time trends across groups by matching study participants on observable characteristics; however, this approach does not address non-observable differences such as patient activation.28 Another limitation is that this analysis only looks at the short-term effects of the UCMyRx intervention. Lastly, this study was done in a large academic healthcare system; therefore, findings may be different in other types of settings.
This study makes a number of contributions to the literature. Foremost, this study shows that even when delivered at an intensity levels lower than what has been observed in RCTs and among patient populations not meeting stringent selection criteria, a primary care–embedded clinical pharmacist–led intervention leads to meaningful improvements in HbA1c levels, among blacks with type 2 diabetes, relative to usual care. Interventions such as UCMyRx may prove more financially feasible for a diverse range of medical practices to adopt, relative to the intervention strategies used in the RCTs. Secondly, given that the effect of UCMyRx on HbA1c was commiserate with what has been observed for interventions such as insulin initiation and prescription oral medications (lowest comorbidity tercile effects) with fewer adverse effects, it will be important for health insurance companies to reimburse appropriately for these interventions. Another benefit of interventions like UCMyRx is the ability to help unburden physicians while improving the quality of diabetes care for patients. Lastly, UCMyRx increases patient self-management opportunities by addressing structural barriers that preclude engagement in care, which are highly prevalent among the black patient population, irrespective of health insurance coverage status. Consequently, interventions such as UCMyRx may help reduce diabetes disparities among blacks.
CONCLUSION
Using a difference-in-differences study design with a propensity-matched comparison group, we found that a primary care–embedded clinical pharmacist–led intervention in a large healthcare system led to a significant reduction in HbA1c among black patients with type 2 diabetes, relative to usual care.
References
Association, A. D. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018 May;41(5):917–928. doi:https://doi.org/10.2337/dci18-0007.
Canedo, J. R., Miller, S. T., Schlundt, D., Fadden, M. K. & Sanderson, M. Racial/Ethnic Disparities in Diabetes Quality of Care: the Role of Healthcare Access and Socioeconomic Status. J. Racial Ethn. Health Disparities. 2018 Feb;5(1):7–14.
Goode, P. Diabetes Disparities in African Americans: A Cry for Help to Primary Care Providers. J Health Dispar Res Prac. 2017 10(4):61–66.
Jensen, G. A. & Li, Y. Long-run health effects of cost-related non-adherence to prescribed medications among adults in late midlife. J. Pharm. Health Serv. Res. 2012 May 3:85–93.
Goyal, A. et al. Racial Differences in the Attainment of Cardiovascular Risk Factor Goals Among Insured Adults with Diabetes Mellitus. J. Am. Coll. Cardiol. 2010 March 55: A142.E1332.
Holland, A. T. et al. Racial/ethnic differences in control of cardiovascular risk factors among type 2 diabetes patients in an insured, ambulatory care population. J. Diabetes Complications. 2013 Jan-Feb 27(1): 34–40.
Peek, M. E., Cargill, A. & Huang, E. S. Diabetes Health Disparities. Med. Care Res. Rev. 2007 Oct;64(5 Suppl):101S–156S.
Gerber, B. S., Cho, Y. I., Arozullah, A. M. & Lee, S.-Y. D. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am. J. Geriatr. Pharmacother. 2010 Apr;8(2):136–145.
Trinacty, C. M. et al. Racial differences in long-term adherence to oral antidiabetic drug therapy: a longitudinal cohort study. BMC Health Serv. Res. 2009 Feb;9:24.
Zhang, J. X., Lee, J. U. & Meltzer, D. O. Risk factors for cost-related medication non-adherence among older patients with diabetes. World J. Diabetes. 2014 Dec;5(6):945–950.
Osborn, C. Y. et al. Health literacy explains racial disparities in diabetes medication adherence. J. Health Commun. 2011;16 Suppl 3:268–278.
Kurlander, J. E., Kerr, E. A., Krein, S., Heisler, M. & Piette, J. D. Cost-related nonadherence to medications among patients with diabetes and chronic pain: factors beyond finances. Diabetes Care. 2009 Dec;32(12):2143–2148.
Adams, A. S., Banerjee, S. & Ku, C. J. Medication adherence and racial differences in diabetes in the USA: an update. Diabetes Manag. 2015;5:79–87.
Rothman, R. L. et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am. J. Med. 2005 Mar;118(3):276–284.
Jaber, L. A., Halapy, H., Fernet, M., Tummalapalli, S. & Diwakaran, H. Evaluation of a Pharmaceutical Care Model on Diabetes Management. Ann. Pharmacother. 1996 Mar;30(3):238–243.
Singal, A. G., Higgins, P. D. R. & Waljee, A. K. A Primer on Effectiveness and Efficacy Trials. Clin. Transl. Gastroenterol. 2014 Jan;5:e45.
Ackermann, R. T. et al. Evaluating Diabetes Health Policies Using Natural Experiments: The Natural Experiments for Translation in Diabetes Study. Am. J. Prev. Med. 2015 Jun;48(6):747–754.
Joish, V. N., Malone, D. C., Wendel, C., Draugalis, J. R. & Mohler, M. J. Development and Validation of a Diabetes Mellitus Severity Index: A Risk-Adjustment Tool for Predicting Health Care Resource Use and Costs. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2005 May;25(5):676–684.
Ryan, J. G., Fedders, M., Jennings, T., Vittoria, I. & Yanes, M. Clinical outcomes and incremental costs from a medication adherence pilot intervention targeting low-income patients with diabetes at risk of cost-related medication nonadherence. Clin. Ther. 2014 Dec;36(12):1991–2002.
Stuart, E. A. Matching methods for causal inference: A review and a look forward. Stat. Sci. Rev. J. Inst. Math. Stat. 2010 Feb;25(1):1–21.
Zhou, H., Taber, C., Arcona, S. & Li, Y. Difference-in-Differences Method in Comparative Effectiveness Research: Utility with Unbalanced Groups. Appl. Health Econ. Health Policy. 2016 Aug;14(4):419–429.
Winter, B. Linear models and linear mixed effects models in R with linguistic applications. 2013: ArXiv13085499 Cs.
Bailey, T. S., Zisser, H. C. & Garg, S. K. Reduction in hemoglobin A1C with real-time continuous glucose monitoring: results from a 12-week observational study. Diabetes Technol. Ther. 2007 Jun;9(3):203–210.
Bhattacharya, R., Zhou, S., Wei, W., Ajmera, M. & Sambamoorthi, U. A Real-World Study of the Effect of Timing of Insulin Initiation on Outcomes in Older Medicare Beneficiaries with Type 2 Diabetes Mellitus. J. Am. Geriatr. Soc. 2015 May;63(5):893–901.
Baxter, M. et al. Estimating the impact of better management of glycaemic control in adults with Type 1 and Type 2 diabetes on the number of clinical complications and the associated financial benefit. Diabet. Med. 2016 Nov;33(11):1575–1581.
Palmer, A. J. et al. The CORE Diabetes Model: Projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr. Med. Res. Opin. 2004 Aug;20 Suppl 1:S5–26.
Kalyani, R. R., Golden, S. H. & Cefalu, W. T. Diabetes and Aging: Unique Considerations and Goals of Care. Diabetes Care. 2017 Apr;40(4):440–443.
Stuart, E. A. et al. Using propensity scores in difference-in-differences models to estimate the effects of a policy change. Health Serv. Outcomes Res. Methodol. 2014 Dec;14(4):166–182.
Acknowledgments
The authors thank Richard Maranon and Janet Chon for providing additional insight into the UcMyRx program and for providing feedback on the manuscript.
Funding
Dr. Carol M. Mangione received support from the University of California at Los Angeles (UCLA), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under National Institutes of Health (NIH)/NIA under Grant P30AG021684, and the Delivery System Reform Incentive Pool (DSRIP) under a Grant from the Centers for Medicare & Medicaid Services (CMS). Dr. Mangione holds the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine, which partially supported her work. Dr. Carol M. Mangione is a member of the United States Preventive Services Task Force (USPSTF). This research was supported by NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
This article does not necessarily represent the views and policies of the USPSTF.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Narain, K.D.C., Doppee, D., Li, N. et al. An Effectiveness Evaluation of a Primary Care–Embedded Clinical Pharmacist–Led Intervention Among Blacks with Diabetes. J GEN INTERN MED 35, 2569–2575 (2020). https://doi.org/10.1007/s11606-020-05750-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-05750-0