Abstract
Background
Osteoporosis guidelines recommend pharmacologic therapy based on 10-year risk of major osteoporotic fracture (MOF) and hip fracture, which may fail to account for patient-specific experiences and values.
Objective
We aimed to determine whether patient decisions to initiate osteoporosis medication agree with guideline-recommended intervention thresholds.
Design and Participants
This prospective cohort study included women aged ≥ 45 with age-associated osteoporosis who attended a group osteoporosis self-management consultation at a tertiary osteoporosis center.
Intervention
A group osteoporosis self-management consultation, during which participants received osteoporosis education and then calculated1 their 10-year MOF and hip fracture risk using FRAX and2 their predicted absolute fracture risk with therapy (assuming 40% relative reduction). Participants then made autonomous decisions regarding treatment initiation.
Main Measures
We evaluated agreement between treatment decisions and physician-set intervention thresholds (10-year MOF risk ≥ 20%, hip fracture risk ≥ 3%).
Key Results
Among 85 women (median [IQR] age 62 [58–67]), 27% accepted treatment (median [IQR] MOF risk, 15.1% [9.9–22.0]; hip fracture risk, 3.3% [1.3–5.3]), 46% declined (MOF risk, 9.5% [6.5–11.6]; hip fracture risk, 1.8% [0.6–2.3]), and 27% remained undecided (MOF risk, 14.0% [9.8–20.2]; hip fracture risk, 4.4% [1.7–4.9]). There was wide overlap in fracture risk between treatment acceptors and non-acceptors. Odds of accepting treatment were higher in women with prior fragility fracture (50% accepted; OR, 5.3; 95% CI, 1.9–15.2; p = 0.0015) and with hip fracture risk ≥ 3% (32% accepted; OR, 3.6; 95% CI, 1.4–9.2; p = 0.012), but not MOF risk ≥ 20% (47% accepted; OR, 3.0; 95% CI, 1.0–8.5; p = 0.105).
Conclusions
Informed decisions to start osteoporosis treatment are highly personal and not easily predicted using fracture risk. Guideline-recommended intervention thresholds may not permit sufficient consideration of patient preferences.
Similar content being viewed by others
INTRODUCTION
Much of chronic disease management aims to determine an individual’s likelihood of experiencing an untoward event (e.g., fracture, myocardial infarction, stroke) and take practical steps to reduce the odds of this happening. Within this paradigm, risk calculators and intervention thresholds based on absolute risk are commonly used as the premise for medical decisions. Medical guidelines exist to direct clinicians through this process and generally recommend interventions that are expected—in the view of the guideline authors—to decrease an individual’s risk of an event by a significant magnitude with an acceptably low risk of unintended side effects. These guidelines are designed to be widely applicable; as a result, recommended treatment intervention thresholds may be based on assumptions about patient preferences and values that are not always correct when applied to individual patients.1, 2 Consequently, patient preference is sometimes at odds with the physician-set recommendations of medical guidelines.
In the case of osteoporosis, both US and Canadian guidelines recommend pharmacologic therapy when 10-year major osteoporotic fracture (MOF) risk is ≥ 20%, or in the setting of prior hip or vertebral fractures.3, 4 US guidelines also recommend treatment of individuals with 10-year risk of hip fracture ≥ 3% or densitometric osteoporosis (i.e., a T-score of ≤ − 2.5 at the spine or hip). First-line pharmacologic therapies for osteoporosis have been shown to reduce the relative risk of fragility fracture by 40–60%, depending on the population, the agent, and the fracture type.5 Despite the clear treatment recommendations outlined in osteoporosis guidelines and supported by strong evidence of efficacy, fewer than 20% of individuals deemed likely to benefit from therapy are treated,6,7,8 and more than half of treated patients stop taking their medication within 2 years.9,10,11 This observation is not unique to osteoporosis: low rates of guideline-concordant therapy have also been observed in patients at increased risk of myocardial infarction12, 13 or stroke.14
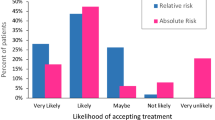
One potential explanation for these “treatment gaps” is that current physician-set intervention thresholds may fail to recognize the high degree of complexity involved in autonomous patient decisions,15, 16 specifically the weighing of risks and benefits according to individual patient experiences and values.17, 18 Existing literature indicates that patient decisions to accept guideline-recommended therapy are influenced by a multitude of factors, not all of which are mutually exclusive or easily explained. For example, in a large randomized controlled trial, higher osteoporosis knowledge scores and greater exercise self-efficacy were associated with an increased likelihood of non-adherence with pharmacologic therapy.19 Beliefs about medication efficacy and potential side effects, which may be influenced not only by osteoporosis knowledge and health literacy but also by personal experience, have also been repeatedly shown to influence osteoporosis treatment uptake.19, 20 In addition, the way in which fracture risk and the expected benefits of therapy are “framed” can influence treatment decisions: for example, patients are more likely to accept therapy when the anticipated benefits of treatment are presented in terms of relative risk reduction rather than absolute risk reduction.21 Of relevance, clinicians are also more likely to agree with guideline-recommended intervention thresholds when risk reduction is expressed in relative rather than absolute terms,21 indicating that this phenomenon is not limited to the lay population. Importantly, the average absolute fracture risk at which patients are willing to consider pharmacologic osteoporosis therapy remains higher than physician-set risk thresholds regardless of how the effects of treatment are framed.22 Patients who are contemplating antihypertensive16, 17 or lipid-lowering therapy23 have also been shown to have higher thresholds for treatment acceptance than physicians.
Medical guidelines may be ineffective at reducing adverse health outcomes when they make recommendations based upon a single risk threshold or risk factor, without consideration of the range of factors that may influence a patient’s acceptance and adherence. A better understanding of patient decisions to initiate or forego pharmacologic treatment could help clinicians better navigate the shared decision-making process and inform the development of future guidelines for chronic disease management. Accordingly, we prospectively evaluated autonomous decisions to accept or decline pharmacologic osteoporosis treatment, made by women with age-associated osteoporosis, and determined the rate of agreement with common guideline-recommended intervention thresholds.
METHODS
We conducted a prospective observational study of women with age-associated osteoporosis who attended a group self-management consult program (SCP) at our tertiary referral center (Calgary, Canada) for osteoporosis between May 2016 and October 2018.
Self-management Consult Program
Since 2016, our center has offered a novel group medical visit (the SCP) as an alternative to traditional one-on-one consultation for patients with age-associated osteoporosis but without significant medical comorbidity. The purpose of the SCP is to facilitate the shared decision-making process and empower patients to make educated and wholly autonomous, value-based treatment decisions. The program involves a multidisciplinary 2-h shared medical appointment (serving 5–10 patients) co-led by a nurse clinician and a specialist physician. Participants are provided with education about osteoporosis, consequences of fragility fracture, fracture risk factors, and detailed benefits and risks of the various pharmacologic treatments. Each patient is helped to estimate and record their 10-year risk of fracture using the FRAX calculator, and, using a pre-printed “fill-in-the-blank” consultation-style worksheet (Online Supplementary Appendix), calculates and records their absolute reduction in fracture risk should therapy be initiated (assuming a 40% relative risk reduction from baseline).5 Participants are then given time to record a decision regarding whether to initiate pharmacologic therapy.
In the SCP, patients receive an individualized fracture risk estimate. Comprehensive, detailed information is provided in an objective and standardized manner. There are multiple interpersonal interactions involving the physician, nurse, and other similar patients to facilitate learning from multiple viewpoints; however, the absence of private consultation precludes any patient from receiving direct advice which might over-emphasize the physician’s values. Prior to the SCP, patients attend a separate 2-h teaching session regarding the basics of osteoporosis and lifestyle interventions such that the total teaching and decision-making process includes more than 4 h of instruction and interaction.
Participants
Participants were women ≥ 45 years referred for age-associated osteoporosis who elected to attend the SCP. The SCP inclusion criteria include: referral from a primary care provider with whom the patient is able to follow-up, able to sit in a classroom for 2 h, and able to make autonomous health decisions. Exclusion criteria include: known secondary osteoporosis/metabolic bone disease, non-ambulatory, history of cognitive impairment, or language difficulties expected to affect participation in the class. A telephone screening interview with an osteoporosis nurse clinician confirmed program suitability prior to enrolment. Informed consent was obtained from all participants prior to study enrollment, and the study received approval from the local Health Research Ethics Board.
Data Collection
Heights were measured using a Harpenden stadiometer and weights using an electronic scale. Clinical risk factors incorporated in the FRAX calculator (Online Supplementary Appendix) were self-reported by participants; a nurse clinician and osteoporosis specialist provided guidance and clarification regarding these risk factors as needed. Bone mineral density T-scores at the femoral neck were obtained from review of each participant’s most recent dual-energy X-ray absorptiometry (DXA) scan; all scans were performed in the community within 24 months leading up to the SCP visit. Each participant calculated their 10-year fracture risk estimates on an iPad, using FRAX for iOS (with bone mineral density), with guidance from the nurse and physician.
Following education and fracture risk estimation, participants were given specific questions intended to help them reflect on their personal values as related to fracture risk, in light of the consequences of fracture and benefits and risks of pharmacologic therapy. Participants were then asked to indicate whether they plan to initiate therapy, decline therapy, or remain undecided. Immediately following the SCP, participants completed a written questionnaire to evaluate perception of fracture risk and anticipated benefit of therapy, adequacy of information provided in the SCP, and confidence in treatment decision. Knowledge of osteoporosis was evaluated using a modified ten-question version of the validated Osteoporosis Knowledge Assessment Tool (OKAT),24 with 1 point awarded for each correct answer and a maximum possible score of 10.
Statistical Analyses
Participant characteristics were examined using descriptive statistics. Participants were then classified into one of three groups based on their choice of whether to initiate pharmacologic osteoporosis therapy: therapy acceptors, therapy decliners, and undecided. Between-group differences in fracture risk estimates were explored using the Kruskal-Wallis test; if between-group differences were identified, post hoc testing was undertaken using Dunn’s multiple comparisons test (with adjusted p values). Between-group differences in history of fragility fracture were assessed using a chi-squared test; Fisher’s exact tests were utilized for post hoc examination of differences. We then calculated the odds of being a therapy acceptor (vs therapy decliner or undecided) if the following treatment thresholds were fulfilled: 10-year MOF risk ≥ 20%, hip fracture risk ≥ 3%, prior fragility fracture. Statistical significance of calculated odds ratios was evaluated using Fisher’s exact tests.
Statistical tests were two-tailed and p values < 0.05 were considered statistically significant. Data analysis was undertaken using SAS v9.4 (SAS Institute, Cary, NC, USA) and Prism v7.01 (GraphPad Software Inc., La Jolla, CA, USA).
RESULTS
Characteristics of the study cohort are displayed in Table 1. A total of 85 women (median [IQR] age 62 [58–67] years) completed the SCP; 28 (32%) had a prior fragility fracture. FRAX 10-year risk estimates for MOF ranged from 3.8 to 37%; risk was ≥ 20% in 15 (17%). Ten-year risk estimates for hip fracture ranged from 0 to 14.4%; risk was ≥ 3% in 31 (37%). Following the SCP, 27% women chose to initiate pharmacologic therapy (therapy acceptors), 46% declined therapy (therapy decliners), and 27% remained undecided (undecided).
Figure 1 illustrates the range of 10-year FRAX estimates for MOF and hip fracture risk, stratified by treatment decision. Median (IQR) MOF risk was 15.1% (9.9–22.0) for therapy acceptors, 9.5% (6.5–11.6) for therapy decliners, and 14.0% (9.8–20.2) for those who remained undecided. Median MOF risk varied between groups (p < 0.001 for between-group difference), being significantly lower in therapy decliners than therapy acceptors (adjusted p = 0.002) and the undecided group (adjusted p = 0.004). However, there was a wide overlap in range of estimated MOF risk between therapy acceptors (4.0–37.4%) and those who did not accept therapy or were undecided (3.8–20.8%). Median (IQR) hip fracture risk was 3.3% (1.3–5.3) for therapy acceptors, 1.8% (0.6–2.3) for therapy decliners, and 4.4% (1.7–4.9) for those who remained undecided (Fig. 1). Median hip fracture risk differed between groups (p < 0.001 for between-group difference) with post hoc testing demonstrating that risk was lower in therapy decliners than therapy acceptors (adjusted p = 0.012) and the undecided group (adjusted p = 0.003). The range of estimated hip fracture risk in therapy acceptors (0.4–14.4%) demonstrated considerable overlap with those who did not accept therapy or were undecided (0.0–8.4%).
Individual osteoporosis treatment decisions and corresponding 10-year FRAX estimates for major osteoporotic fracture (MOF) (a) and hip fracture (b), among women (n = 85) who attended an osteoporosis self-management program. Vertical dashed lines indicate common guideline-recommended intervention thresholds.
As shown in Table 1, prior fragility fracture was reported by 61% of therapy acceptors, 10% of therapy decliners, and 44% of those who were undecided (p < 0.001 for between-group difference). A history of fragility fracture was less common in therapy decliners than therapy acceptors (adjusted p < 0.0001) or the undecided group (adjusted p = 0.014).
Of the 23 therapy acceptors, 17 (74%) met one or more guideline-based treatment thresholds; the remaining 6 (26%) had MOF risk < 20%, hip fracture risk < 3%, and no history of fragility fracture. Table 2 indicates the odds of being a therapy acceptor (versus therapy decliner or undecided) if an individual’s FRAX estimate exceeded each of the selected risk thresholds or if they had a personal history of fragility fracture. Therapy was chosen in roughly half of participants meeting each intervention threshold, with the exception of the ≥ 3% 10-year hip fracture risk threshold; only 32% of participants who exceeded this threshold chose to initiate treatment. Having a prior fragility fracture or hip fracture risk ≥ 3% was associated with significantly higher odds of choosing treatment, while having a MOF risk ≥ 20% was not (Table 2).
Participant perceptions regarding fracture risk, anticipated benefit of pharmacologic therapy, whether information provided was adequate to facilitate a treatment decision, and confidence in their chosen treatment plan are shown in Table 1. The vast majority of participants (86%) felt that the SCP provided enough information to make a treatment decision, and most felt confident in their treatment decision (69%). Among the 28 participants with a prior history of fragility fracture, 64% indicated they were worried about their fracture risk, 46% felt treatment was likely to be of benefit, 86% felt they received enough information to make a decision, and 68% expressed confidence in their decision.
DISCUSSION
We examined decisions to accept or decline pharmacologic osteoporosis treatment, made wholly autonomously by women with age-associated osteoporosis following extensive education and individualized fracture risk assessment. Women who chose to initiate osteoporosis therapy had higher FRAX-estimated 10-year MOF and hip fracture risk than those who did not choose to initiate treatment. However, we found a wide overlap in 10-year fracture risk estimates between those who accepted therapy and those who declined or remained undecided, indicating considerable individual variation in treatment preferences that did not correspond to traditional physician-set intervention thresholds. Rather, our findings suggest that the decision to accept pharmacologic therapy is highly personal and likely to be influenced by past experiences, including prior fragility fracture.
Although common guideline-based intervention thresholds (i.e., 10-year risk of MOF ≥ 20%, hip fracture ≥ 3%) were not mentioned at the SCP visit, we found a three to fourfold increase in the odds of accepting pharmacologic osteoporosis therapy when fracture risk exceeded each of these thresholds. However, fewer than half of participants exceeding these thresholds ultimately accepted treatment, suggesting that many patients who meet physician-set risk thresholds for pharmacologic treatment do not perceive, on a personal level, the benefits of therapy to outweigh the risks. Our findings echo recent work by Kalluru, who found many postmenopausal women are unwilling to consider osteoporosis medications unless 5-year fracture risk exceeds 50–60%.22 Similarly, patients contemplating initiation of antihypertensive16, 17 and lipid-lowering medication23 tend to have higher risk thresholds for treatment than physicians.
Current data indicate low rates of treatment uptake6,7,8 and adherence9,10,11 in individuals who meet guideline-based criteria for pharmacologic therapy to reduce the risk of untoward events. This “treatment gap” has been attributed to lack of identification of high-risk individuals and inadequate patient education, particularly regarding expected risks and benefits of therapy.25 However, even among patients who have been identified as likely to benefit from pharmacologic therapy, uptake and adherence remain low. For example, after implementation of a Canadian population–based fracture liaison service, which identified individuals with a recent fragility fracture and contacted them by telephone in addition to providing notification to their primary care physicians, treatment uptake remained below 20%.26 Findings from the Global Longitudinal Study of Osteoporosis in Women (GLOW) suggest that low rates of treatment acceptance may not be entirely related to inadequate education, either. In the GLOW, women with a prior fragility fracture (mean age 75 years) were randomized to receive a direct-to-patient video intervention (5–15 min in length) or usual care. At 6-month follow-up, osteoporosis medications were used by only 11.7% in the intervention group and 11.4% in the usual care group.27 Cram and colleagues28 examined concordance of pharmacologic treatment uptake with US guidelines,4 observing that approximately 33% of individuals meeting one or more intervention threshold initiated therapy within a year of fracture risk evaluation; delivery of a tailored patient activation letter and educational brochure did not increase treatment uptake. A randomized controlled trial evaluating the effects of an osteoporosis decision aid found that, among individuals deemed to be at high risk of fracture (10-year risk > 30%), antiresorptive therapy was initiated in only 40% of those who received the decision aid intervention compared with 33% in those who did not.29
In our study, participants received more than 4 h of intensive education, including an interactive discussion of medication risks and benefits. Following the SCP, our cohort demonstrated a good knowledge of general osteoporosis principles. Taken in the context of the existing literature, our finding that 47–50% of women who met local guideline-based intervention thresholds accepted therapy suggests that the combined education and consultation experience of the SCP can improve treatment uptake compared with the status quo,6, 26 and also in comparison to educational27, 28 and shared decision-making interventions29 delivered in isolation. Further exploration is required to determine which component(s) of our educational intervention have the greatest impact on treatment decisions, and whether the SCP would have similar effects on treatment uptake in other chronic medical conditions.
Importantly, our observations also indicate that even after intensive education, many “high risk” individuals will still choose to forego therapy. This raises the possibility that physicians, when interpreting the evidence and clinical practice guidelines with population health in mind, may set expectations for treatment uptake that are unrealistic where individual patients are considered. For example, while physician-set intervention thresholds have the potential for benefit from population health and cost-effectiveness standpoints, at the individual level, taking a medication for several years to reduce one’s MOF risk from 20 to 12% or hip fracture risk from 3 to 1.8% may not be considered sufficiently beneficial compared with one’s reasons against accepting therapy. This may be in part because physicians are used to synthesizing information about risk reduction in terms of relative rather than absolute risk reduction, which may bias recommendations towards treatment. Sinsky et al. have shown that physicians (and patients) are less likely to agree with guideline-based intervention thresholds when presented with information about absolute risk reduction (e.g., a reduction in fracture risk from 20 to 12%) than relative risk reduction (e.g., a 40% reduction in fracture risk).21 Our SCP is novel in that patients are provided with information about both relative and absolute risks and then make wholly autonomous treatment decisions, without being subjected to framing of risks or physician value judgements. In this setting, a non-trivial proportion of well-informed patients will disagree with physician-set intervention thresholds for fracture prevention. These decisions should be viewed as reasonable and appropriate within the context of person-centered, preference-sensitive care.
Importantly, we observed that a quarter of participants remained uncertain about their preferred treatment plan following the SCP. This highlights that decisions to initiate osteoporosis therapy are not straightforward and may require more than 4 h of education and self-reflection to complete. As with informed consent, patients have been shown to perceive decision-making as a fluid, ongoing process.30 In the context of osteoporosis, perceptions of fracture risk and the need to take osteoporosis medications may change over time,31 although among women with 10-year fracture risk > 20% who declined pharmacologic therapy, Scoville and colleagues found that decisions to refuse therapy remained consistent 6 months later.32 Our results raise questions about the feasibility of brief office visits to make osteoporosis management decisions; further development of patient-oriented resources and programs such as the SCP may be necessary in order to meet patients’ need for decision assistance.
In contrast to the “high risk” patients who declined therapy, we observed a quarter of individuals in the present study who opted to initiate pharmacologic therapy did not meet any traditional intervention thresholds for MOF or hip fracture risk and had no personal history of fragility fracture. Although pharmacologic treatment of low-risk individuals is not uncommon and has been described previously,33 we are not aware of any studies that have examined patient-driven (rather than physician-driven) decisions to start therapy in the low-risk setting. More research is required to understand the motivating factors for treatment initiation in this population.
Our findings should be interpreted in the context of some limitations. Study participants were relatively young, healthy postmenopausal women with the ability to make autonomous decisions regarding medical care. Our results may not be generalizable to older, frailer individuals. We used a validated tool to assess osteoporosis knowledge; this tool does not assess understanding of risk, which is an important consideration when making decisions regarding preventative therapy. Also, our data regarding decisions to initiate pharmacologic therapy is collected immediately following the SCP. However, some individuals make their decision at a later time (i.e., after discussion with family, friends, primary care provider), and the present data do not capture how an initial decision may be modified or reversed following outside discussion; longitudinal follow-up is underway to answer this question. Even in the context of these limitations, the present study represents an important contribution as the first to evaluate wholly autonomous osteoporosis treatment decisions in a cohort of women who have received individualized fracture risk assessments and extensive education.
CONCLUSIONS
While the use of risk-based intervention thresholds in medical guidelines may be appropriate from population health and cost-effectiveness standpoints, current recommendations are frequently at odds with the preferences of informed and educated patients. Following individualized fracture risk assessment, extensive education, and an autonomous decision-making process, less than half of women with age-associated osteoporosis who are considered “high risk” by commonly recommended treatment thresholds accept anti-fracture therapy, and over a quarter of women who do not meet treatment thresholds will choose to initiate pharmacologic therapy, with wide overlap in 10-year fracture risk estimates between therapy acceptors and decliners. Further study is required to characterize the personal experiences and values that influence these treatment decisions, although personal history of fragility fracture appears to be a strong motivating factor. Without patient “buy-in”, physician-led efforts to increase treatment uptake may fail over the long term. While increased physician training in shared decision-making and the development of programs that deliver consultative services in conjunction with extensive patient education may be helpful in addressing this problem, a shift in the way that clinical practice guidelines are interpreted and applied is also required: when a well-informed patient disagrees with medical guidelines, this should be viewed as appropriate and acceptable.
References
Ubel PA. Medical Facts versus Value Judgements - Toward Preference-Sensitive Guidelines. N Engl J Med. 2015;372(26). https://doi.org/10.1056/NEJMp1504245
Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ. 1999;318(7182):527-30. https://doi.org/10.1136/bmj.318.7182.527
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182(17):1864-73. https://doi.org/10.1503/cmaj.100771
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int 2014;25(10):2359-81. https://doi.org/10.1007/s00198-014-2794-2
Reid IR. Efficacy, effectiveness and side effects of medications used to prevent fractures. J Intern Med 2015;277(6):690-706. https://doi.org/10.1111/joim.12339
Leslie WD, Giangregorio LM, Yogendran M, Azimaee M, Morin S, Metge C, et al. A population-based analysis of the post-fracture care gap 1996-2008: the situation is not improving. Osteoporos Int 2012;23(5):1623-9. https://doi.org/10.1007/s00198-011-1630-1
Kanis JA, Borgstrom F, Compston J, Dreinhofer K, Nolte E, Jonsson L, et al. SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 2013;8:144. https://doi.org/10.1007/s11657-013-0144-1
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD. Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 2014;29(9):1929-37. https://doi.org/10.1002/jbmr.2202
Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, et al. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc 2006;81(8):1013-22. https://doi.org/10.4065/81.8.1013
Burden AM, Paterson JM, Solomon DH, Mamdani M, Juurlink DN, Cadarette SM. Bisphosphonate prescribing, persistence and cumulative exposure in Ontario, Canada. Osteoporos Int 2012;23(3):1075-82. https://doi.org/10.1007/s00198-011-1645-7
Modi A, Sajjan S, Insinga R, Weaver J, Lewiecki EM, Harris ST. Frequency of discontinuation of injectable osteoporosis therapies in US patients over 2 years. Osteoporos Int 2017;28(4):1355-63. https://doi.org/10.1007/s00198-016-3886-y
Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med 2012;125(9):882-7 e1. https://doi.org/10.1016/j.amjmed.2011.12.013
Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 2005;165(10):1147-52. https://doi.org/10.1001/archinte.165.10.1147
Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why Do Patients With Atrial Fibrillation Not Receive Warfarin? Arch Intern Med 2000;160(1):41. https://doi.org/10.1001/archinte.160.1.41
Montgomery AA, Harding J, Fahey T. Shared decision making in hypertension: the impact of patient preferences on treatment choice. Fam Pract 2001;18(3):309-13.
McAlister FA, Connor AM, Wells G, Grover SA, Laupacis A. When should hypertension be treated? The different perspectives of Canadian family physicians and patients. Can Med Assoc J 2000;163(4):403.
Steel N. Thresholds for taking antihypertensive drugs in different professional and lay groups: questionnaire survey. Bmj. 2000;320(7247):1446-7. https://doi.org/10.1136/bmj.320.7247.1446
Neuner JM, Schapira MM. The importance of physicians’ risk perception in osteoporosis treatment decision making. J Clin Densitom 2012;15(1):49-54. https://doi.org/10.1016/j.jocd.2011.07.008
Hall SF, Edmonds SW, Lou Y, Cram P, Roblin DW, Saag KG, et al. Patient-reported reasons for nonadherence to recommended osteoporosis pharmacotherapy. J Am Pharm Assoc (2003). 2017;57(4):503-9. https://doi.org/10.1016/j.japh.2017.05.003
Lindsay BR, Olufade T, Bauer J, Babrowicz J, Hahn R. Patient-reported barriers to osteoporosis therapy. Arch Osteoporos 2016;11(1):1-8.
Sinsky CA, Foreman-Hoffman V, Cram P. The impact of expressions of treatment efficacy and out-of-pocket expenses on patient and physician interest in osteoporosis treatment: implications for pay-for-performance programs. J Gen Intern Med 2008;23(2):164-8. https://doi.org/10.1007/s11606-007-0490-z
Kalluru R, Petrie KJ, Grey A, Nisa Z, Horne AM, Gamble GD, et al. Randomised trial assessing the impact of framing of fracture risk and osteoporosis treatment benefits in patients undergoing bone densitometry. BMJ Open 2017;7(2):e013703. https://doi.org/10.1136/bmjopen-2016-013703
Wouters H, Van Dijk L, Van Geffen EC, Geers HC, Souverein PC, Bouvy ML, et al. Do the benefits of statins outweigh their drawbacks? Assessing patients’ trade-off preferences with conjoint analysis. Int J Cardiol 2014;176(3):1220-2. https://doi.org/10.1016/j.ijcard.2014.07.219
Winzenberg TM, Oldenburg B, Frendin S, Jones G. The design of a valid and reliable questionnaire to measure osteoporosis knowledge in women: the Osteoporosis Knowledge Assessment Tool (OKAT). BMC Musculoskelet Disord 2003;4:17. https://doi.org/10.1186/1471-2474-4-17
Khosla S, Shane E. A Crisis in the Treatment of Osteoporosis. J Bone Miner Res 2016;31(8):1485-7. https://doi.org/10.1002/jbmr.2888
Majumdar SR, Lier DA, Hanley DA, Juby AG, Beaupre LA, Team S-P. Economic evaluation of a population-based osteoporosis intervention for outpatients with non-traumatic non-hip fractures: the “Catch a Break” 1i [type C] FLS. Osteoporos Int 2017;28(6):1965-77. https://doi.org/10.1007/s00198-017-3986-3
Danila MI, Outman RC, Rahn EJ, Mudano AS, Redden DT, Li P, et al. Evaluation of a Multimodal, Direct-to-Patient Educational Intervention Targeting Barriers to Osteoporosis Care: A Randomized Clinical Trial. J Bone Miner Res 2018;33(5):763-72. https://doi.org/10.1002/jbmr.3395
Cram P, Wolinsky FD, Lou Y, Edmonds SW, Hall SF, Roblin DW, et al. Patient-activation and guideline-concordant pharmacological treatment after bone density testing: the PAADRN randomized controlled trial. Osteoporos Int 2016;27(12):3513-24. https://doi.org/10.1007/s00198-016-3681-9
Montori VM, Shah ND, Pencille LJ, Branda ME, Van Houten HK, Swiglo BA, et al. Use of a decision aid to improve treatment decisions in osteoporosis: the osteoporosis choice randomized trial. Am J Med 2011;124(6):549-56. https://doi.org/10.1016/j.amjmed.2011.01.013
Fraenkel L, McGraw S. Participation in medical decision making: the patients’ perspective. Med Decis Mak 2007;27(5):533-8. https://doi.org/10.1177/0272989X07306784
Wozniak LA, Johnson JA, McAlister FA, Beaupre LA, Bellerose D, Rowe BH, et al. Understanding fragility fracture patients’ decision-making process regarding bisphosphonate treatment. Osteoporos Int 2017;28(1):219-29. https://doi.org/10.1007/s00198-016-3693-5
Scoville EA, Ponce de Leon Lovaton P, Shah ND, Pencille LJ, Montori VM. Why do women reject bisphosphonates for osteoporosis? A videographic study. PLoS One. 2011;6(4):e18468. https://doi.org/10.1371/journal.pone.0018468
Fenton JJ, Robbins JA, Amarnath AD, Franks P. Osteoporosis overtreatment in a regional health care system. JAMA Intern Med 2016;176(3):391-3. https://doi.org/10.1001/jamainternmed.2015.6020
Funding
This research was funded by a grant from Alberta Innovates Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all participants prior to study enrollment, and the study received approval from the local Health Research Ethics Board.
Conflict of Interest
EOB reports receiving honoraria from Eli Lilly and Amgen for serving on their Scientific Advisory Boards, and has received research funding from Amgen. All remaining authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Materials
ESM 1
(DOCX 32 kb)
Rights and permissions
About this article
Cite this article
Billington, E.O., Feasel, A.L. & Kline, G.A. At Odds About the Odds: Women’s Choices to Accept Osteoporosis Medications Do Not Closely Agree with Physician-Set Treatment Thresholds. J GEN INTERN MED 35, 276–282 (2020). https://doi.org/10.1007/s11606-019-05384-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05384-x