Abstract
Background
Post-stroke care delivery may be affected by provider participation in Medicare Shared Savings Program (MSSP) Accountable Care Organizations (ACOs) through systematic changes to discharge planning, care coordination, and transitional care.
Objective
To evaluate the association of MSSP with patient outcomes in the year following hospitalization for ischemic stroke.
Design
Retrospective cohort
Setting
Get With The Guidelines (GWTG)–Stroke (2010–2014)
Participants
Hospitalizations for mild to moderate incident ischemic stroke were linked with Medicare claims for fee-for-service beneficiaries ≥ 65 years (N = 251,605).
Main Measures
Outcomes included discharge to home, 30-day all-cause readmission, length of index hospital stay, days in the community (home-time) at 1 year, and 1-year recurrent stroke and mortality. A difference-in-differences design was used to compare outcomes before and after hospital MSSP implementation for patients (1) discharged from hospitals that chose to participate versus not participate in MSSP or (2) assigned to an MSSP ACO versus not or both. Unique estimates for 2013 and 2014 ACOs were generated.
Key Results
For hospitals joining MSSP in 2013 or 2014, the probability of discharge to home decreased by 2.57 (95% confidence intervals (CI) = − 4.43, − 0.71) percentage points (pp) and 1.84 pp (CI = − 3.31, − 0.37), respectively, among beneficiaries not assigned to an MSSP ACO. Among discharges from hospitals joining MSSP in 2013, beneficiary ACO alignment versus not was associated with increased home discharge, reduced length of stay, and increased home-time. For patients discharged from hospitals joining MSSP in 2014, ACO alignment was not associated with changes in utilization. No association between MSSP and recurrent stroke or mortality was observed.
Conclusions
Among patients with mild to moderate ischemic stroke, meaningful reductions in acute care utilization were observed only for ACO-aligned beneficiaries who were also discharged from a hospital initiating MSSP in 2013. Only 1 year of data was available for the 2014 MSSP cohort, and these early results suggest further study is warranted.
Registration
None
Similar content being viewed by others
INTRODUCTION
Since 2010, at least 900 Accountable Care Organizations (ACOs) have formed over 1300 payment contracts with public and commercial payers; Medicare accounted for 563 of those contracts in 2017.1,2,3 ACO contracts aim to align economic incentives with coordination of care, population health management, and care management programs.4,5,6,7 The Centers for Medicare and Medicaid Services (CMS) implemented the Medicare Shared Savings Program (MSSP) to allow provider groups to retain a portion of the savings (or losses for the few ACOs participating in risk-bearing tracks) generated by the coordination of care for Medicare fee-for-service (FFS) beneficiaries, within the FFS reimbursement structure. These contract incentives are expected to shift ACO care from high-cost inpatient settings to home and outpatient settings. However, little is known about the impact of participation on post-discharge inpatient use following ischemic stroke for elderly Medicare beneficiaries.
At a cost of $30 billion annually, health services use remains high over the year following hospitalization for ischemic stroke, and post-acute care is typically provided in skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs), home health agencies, and/or outpatient rehabilitation settings.8, 9 One in five Medicare ischemic stroke patients is readmitted within 30 days, with higher rates among patients with multiple chronic conditions.9, 10 Post-stroke care delivery may be impacted by ACO strategies including discharge planning, care management, and transitions of care to reduce preventable rehospitalization.11,12,13,14,15,16,17,18,19 In addition, care management programs may improve anticoagulant persistence and adherence impacting long term clinical outcomes (e.g., recurrent stroke, mortality). However, it remains unknown whether hospital participation in ACO MSSP reduces resource utilization and improves longitudinal outcomes in ischemic stroke. Our objective was to evaluate the association of hospital MSSP participation and beneficiary MSSP assignment with health services use and clinical outcomes in the year following hospitalization for mild to moderate ischemic stroke.
METHODS
Our study used hospitalization data from the national registry Get With The Guidelines–Stroke (GWTG–Stroke) linked to Medicare FFS claims files in an observational, difference-in-differences study design. This study compared 1-year outcomes among (1) patients with incident mild or moderate ischemic stroke presenting at a hospital participating in an MSSP ACO contract (referred to as MSSP hospital) or assigned to an MSSP ACO by CMS (referred to as ACO-aligned) and (2) ischemic stroke patients with neither MSSP exposure.
Data Sources
GWTG–Stroke provides a rich inventory of patient-level clinical factors and medical history to facilitate robust assessment of the impact of ACOs on stroke care. Hospitalization records from GWTG–Stroke registry for admissions in years 2010 to 2014 were linked to CMS denominator and inpatient claims files for years 2010 to 2014 using a validated algorithm.20 These data were merged with CMS MSSP provider- and beneficiary-level files for performance years 2013 and 2014, the Area Deprivation Index (ADI),21 and the Area Heath Resource File (AHRF) for years 2010 to 2014 to obtain county-level socioeconomic characteristics. Inpatient claims data available enabled follow-up of clinical outcomes through December 2014.
Study Population
Our population included Medicare FFS patients hospitalized in a hospital participating in the GWTG–Stroke registry between January 2010 and December 2014 who were > 65 years with a physician-adjudicated diagnosis of ischemic stroke, discharged alive, and linked to CMS claims. Patients with prior stroke were excluded to prevent differential shifts in stroke history between the treatment groups from biasing estimates. Additional exclusions included discharge disposition as Left Against Medical Advice (n = 838), or missing AHRF, race, or discharge disposition (n = 1881). To ensure the cohort survived long enough to benefit from ACO strategies, beneficiaries likely to have high mortality rates post-discharge were excluded, including discharge to hospice; comfort measures only during the hospitalization; severe stroke (National Institutes of Health Stroke Scale (NIHSS) score of ≥ 16); provider-reported limited life expectancy; or GWTG mortality risk prediction score > 0.15 (N = 54,128) (see online appendix).22
Measures
Exposure
Hospital and beneficiary ACO status measures were obtained from the CMS MSSP provider- and beneficiary-level files for 2013 and 2014. We defined two Hospital MSSP treatment groups by MSSP start year (2013 or 2014). The control group includes hospitals who did not initiate MSSP ACO contract during the study period. While the first MSSP ACOs began with staggered start dates in 2012, the 2012 ACOs performance period concluded at the end of the 2013 calendar year and CMS includes them in the 2013 performance year file. There was dramatic growth in participation with 106 new MSSP ACOs in 2013 and 193 in 2014.
The binary indicator for beneficiary ACO alignment was ascertained from the CMS MSSP assignment records. CMS assigns patients to an ACO if the plurality of their care was received from an ACO provider during the year using a claims based algorithm (42 CFR 425.402 - Basic assignment methodology). Assignment in the quarter prior to hospitalization was used to avoid selection bias for patients with short survival in the period directly following discharge (see online appendix).23 Of discharges from an MSSP hospital, 28.8% were ACO-aligned beneficiaries.
Outcomes
Measures of acute care use included discharge to home (binary, registry data), 30-day all-cause hospital readmissions (binary, claims data), length of index hospital stay (continuous, claims data), and days in the community, defined as days alive and not in an inpatient facility or SNF, also called “home-time” in the year following discharge (continuous, claims data).24 Clinical outcomes in the year following discharge included days to recurrent stroke and all-cause mortality. A recurrent stroke was identified by a principal diagnosis (ICD-9 codes 430, 431, 432, 433.x1, 434.x1, or 436) on an inpatient claim or observation stay in the year following discharge.25 All-cause, rather than stroke-specific, mortality was assessed because 44% of deaths following stroke are not stroke related and data for cause of death is limited.26 Days of follow-up were censored at the first non-FFS day after discharge, 1 year of follow-up, death, or end of study period (December 31, 2014).
Covariates
Patient data provided by GWTG–Stroke included age, race (White, Black, Asian, and other), gender, Hispanic ethnicity, Medicaid dual eligible status, medical history (current smoker, hypertension, diabetes, myocardial infarction, heart failure, and atrial fibrillation), stroke severity as measured by NIHSS, and health status at discharge including laboratory values (continuous), ability to ambulate (binary), and the Modified Rankin Scale (categorical). Chronic kidney disease was defined using estimated creatinine clearance (categorical).27 Models include 5-year age categories as well as the interaction of sex and age group to allow for nonlinear effects of age.28, 29 Characteristics missing more than 1% of values were imputed using multiple imputation by fully conditional specification (online appendix).30
Hospital factors include number of beds (continuous), census region (categorical), and binary indicators for rural status, teaching hospital, primary stroke center, and for-profit ownership. Market factors include continuous measures for proportion of residents > 65 years, number of primary care physicians/10,000 residents, proportion of households in poverty, and total population (log).
ACO Characteristics
ACO characteristics included primary care focus (> 10 vs. ≤ 10 primary care providers/1000 beneficiaries), specialty focused (> 10 vs. ≤ 10 specialists/1000 beneficiaries), and size (> 20,000 vs. ≤ 20,000 beneficiaries), MSSP market penetration (> 30% vs. ≤ 30% of hospital discharges aligned with any MSSP ACO), and ACO care continuity (beneficiary assigned vs. not assigned to the same MSSP ACO in which the hospital participates).
Statistical Analyses
A difference-in-differences (DD) design was used to estimate the changes in the outcome in the ACO group from baseline to the post-ACO periods compared with controls. The DD method controls for unobserved differences between the treatment and control groups at baseline that do not change during the study period, and the parallel trend assumption is supported in prior studies of MSSP.28, 29, 31,32,33,34,35 The interaction of the hospital MSSP treatment group (no MSSP, 2013 MSSP, 2014 MSSP) and patient admission year (2010–2014) defines three DD estimates: (1) for 2013 MSSP hospitals in the year 2013, (2) for 2013 MSSP hospitals in the year 2014, and (3) for 2014 MSSP hospitals in the year 2014. The base year of 2010 was selected as the reference year to ensure the comparison year completely preceded program implementation. MSSP ACOs may begin implementing ACO strategies prior to the MSSP start date in preparation, which would bias results towards the null. The interaction of hospital MSSP treatment group with beneficiary ACO alignment allows the effect of beneficiary MSSP status to vary by hospital MSSP status. To evaluate effect modification, we added an interaction of binary ACO characteristics with the DD.
Binary outcomes (discharge home and readmission) were modeled using logistic regression and confidence intervals for predicted probabilities were generated with the delta method. Negative binomial models with a log link were used to estimate length of index hospital stay and days in the community. For home-time, an offset for log of the proportion of follow-up time within 1 year after index discharge was used to account for time at risk during the follow-up period.36 Cox proportional hazards models were used to evaluate time to event outcomes (e.g., recurrent stroke and mortality). Statistical models included hospital referral regions (HRRs) fixed effects to control for the unobserved, time-invariant differences in regional usage patterns. We considered using a non-independent correlation structure to model clustering of patient outcomes within the hospital; however, hospital id explained too little of the residual variation (< 5%). Standard errors were adjusted using the Huber-White method to allow for potential clustering by HRR. Year and month fixed effects were also included to account for changes over time and seasonal variation in outcomes.37
We used SAS, version 9.4 (SAS Institute), and STATA, version 15 (StataCorp LLC), for statistical analyses. We defined statistical significance as p value less than 0.05 (2-sided). [Redacted] institutional review board determined that the study did not involve human subjects and was thus exempt from review.
RESULTS
Table 1 compares patient, hospital, and country characteristics for beneficiaries discharged from MSSP hospitals (n = 273) versus at non-MSSP hospitals (n = 1490) prior to the implementation of the MSSP (January 2010 to April 2012). Differences in patient characteristics were small (< 2 percentage points) in the pre-period, except patients at MSSP hospitals are more likely to have private insurance (e.g., Veterans Affairs or supplemental Medicare policy) with 41% versus 36% in the non-MSSP group. Relative to non-MSSP hospitals, MSSP hospitals were larger, more urban, more likely to be a teaching hospital, and located in counties with lower poverty rates and higher rates of primary care physicians. Differential changes in the MSSP group in the post-MSSP period were observed primarily among hospital and county characteristics rather than patient characteristics.
Difference-in-Differences Results
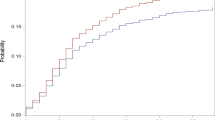
Prior to implementation of the MSSP, trends in predicted utilization and clinical outcomes were not significantly (p value < 0.05; online appendix, Table S2) different for hospitals joining MSSP in 2013 or 2014 compared with hospitals not joining MSSP during the study period (Fig. 1). Hospital participation in MSSP was associated with reduced discharge to home, but was not associated with changes in readmission, length of stay, or home-time (Fig. 2). Relative to hospitals not participating in MSSP in 2014, the probability of discharge to home decreased by 2.57 (95% confidence intervals (CI) = − 4.43, − 0.71) percentage points (pp) for hospitals joining MSSP in 2013 and 1.84 pp (CI = − 3.31, − 0.37) for hospitals joining MSSP in 2014. This significant result persisted in models with and without beneficiary ACO alignment and interactions. Hospital participation in MSSP was not associated with mortality or recurrent stroke within 1 year of hospitalization for incident ischemic stroke (online appendix, Table S3).
Trends in patient outcomes by hospital MSSP ACO implementation year (with 95% CI). MSSP, Medicare Shared Savings Program; CI, 95% confidence interval. Days in the community was calculated as days alive and not in an inpatient or skilled nursing facility. Adjusted models controlled for patient demographics, health status at discharge, medical history, hospital factors, county factors, no evaluation and management visit the year prior to incident stroke and fixed effects for hospital referral region, and year/month of admission.
Difference-in-differences estimates for MSSP versus non-MSSP hospitals and estimates for the association of ACO-aligned beneficiaries with outcomes (with 95% CI). CI, 95% confidence intervals. Days in the community is defined as days not in an inpatient or skilled nursing facility. All models were adjusted for patient demographics, health status at discharge, medical history, hospital factors, county factors, no evaluation and management visit the year prior to incident stroke and fixed effects for Hospital Referral Region, and year/month of admission.
ACO-Aligned Beneficiary Results
For patients discharged from hospitals joining MSSP in 2013, beneficiary ACO alignment versus not was associated with reduced length of index hospital stay, increased discharge to home, increased number of days in the community (Fig. 3). Specifically, probability of discharge to home increased by 1.87 pp (CI = 0.83, 2.91)), length of stay decreased by 0.17 (CI − 0.27, − 0.06) days, and days in the community increased by 3.25 (CI 1.03, 5.48) days. Beneficiary ACO alignment was not significantly associated with changes in utilization for patients discharged from hospitals in the 2014 MSSP cohort. For patients discharged from non-MSSP hospitals, ACO alignment versus not was associated only with discharge to home, with an increase of 0.91 pp (CI = 0.04, 1.78). No evidence of an association between beneficiary ACO alignment and recurrent stroke or mortality was observed.
ACO Characteristics
ACO characteristics associated with higher rates of home-time in the 90 day post-acute period were size greater than 20,000 lives (IRR = 1.03; 95% CI = 1.01, 1.06), care continuity for ACO-aligned beneficiaries hospitalized within their ACO (IRR = 1.03; 95% CI = 1.00, 1.05), and hospital MSSP penetration greater than 30% (IRR = 1.02; 95% CI 1.11, 1.05). No significant differences were found by number of providers, number of specialists, or market factors (Fig. 4).
Estimates for potential moderators of the relationship between MSSP hospital status and home-time with 95% confidence intervals.*Value > 75th vs. ≤ 75th percentile. PCP, primary care physician. Care continuity (binary) is non-zero when the beneficiary is aligned with the same ACO providing acute stroke care during hospitalization. MSSP market penetration (continuous) is the proportion of hospital discharges where the beneficiary is aligned with any MSSP ACO. Area deprivation and PCP supply are county-level factors from the Area Deprivation Index and Area Health Resource File respectively.
DISCUSSION
We evaluated the association of hospital MSSP participation and beneficiary ACO alignment with acute care use and clinical outcomes in the year following hospitalization for mild to moderate severity ischemic stroke. MSSP was not associated with clinical outcomes including mortality, recurrent stroke, and 30-day all-cause readmission. Meaningful reductions in acute care utilization and increased home-time were observed only for beneficiaries assigned to an MSSP ACO and discharged from a hospital joining the MSSP in 2013. Among beneficiaries not assigned to an MSSP ACO, hospital MSSP status was associated with reduced probability of discharge to home.
The observed increase in discharge to home and days in the community in the year following incident stroke for ACO-aligned beneficiaries aligns with evidence that ACOs reduce intensity of health services use among Medicare beneficiaries; however, the difference was not consistently observed and depended on hospital MSSP participation.31, 34, 38, 39 Given the incentives for cost containment in MSSP, the reductions in discharge to home among MSSP hospitals for non-aligned beneficiaries were unexpected. In hospitalized Medicare beneficiaries, MSSP has been associated with increases in discharge to home and reductions in hospital readmissions from SNF.40, 41 Conversely, two other studies found small but significant increases in readmissions among subgroups of clinically vulnerable patients, in which stroke was a top diagnosis group, and surgical patients.28, 42, 43
Our findings suggest the potential benefit of the MSSP for hospitalized ACO-aligned beneficiaries is strengthened by hospital MSSP participation. In 2014, about half of ACOs included an ACO, and only 10% of hospitals participated in a Medicare ACO.44 Hospitals participating in the MSSP may have greater data sharing capacity and better discharge planning to support care coordination within the ACO. While acute care providers in ACOs may focus on internal care processes that impact ACO-aligned and non-aligned beneficiaries alike, non-acute ACO providers often employ external patient support personnel.19 Through these added programs, ACO-aligned patients may receive different services and have different outcomes than non-aligned patients receiving similar care from the same ACO providers. There is a need for more evidence to understand how ACOs are impacting care through acute and outpatient care pathways.
The high level of guideline concordance among GWTG–Stroke hospitals may leave limited room for improvement. GWTG–Stroke initiation has been associated with sustained accelerated increase in discharge home in the first 18 months.45 In this context, increasing discharge to home beyond the high baseline rates may not benefit patients who need higher intensity post-acute care. Furthermore, use of higher intensity care post-acute care settings like inpatient or skilled nursing rehabilitation settings has been associated with improved patient outcomes and may represent better quality of care despite the increased cost.46 Reductions in discharge to home may reflect the persistent quality improvement efforts beyond the MSSP in this sample of hospitals.
ACOs use population health management strategies and systemic changes to improve care that may take years to implement. The lack of significant findings for the group of hospitals joining ACOs in 2014 may be driven by the lack of data post ACO implementation as we have only 1 year of data. Additionally, early ACO savings have resulted from small shifts among large segments of the patient population rather than relatively smaller segments of high-cost patient groups.47, 48 Of the 33 MSSP quality measures in 2013–2014, two relate to patients with ischemic vascular disease—targeting the completion of lipid profiles and low-density lipoprotein control via use of aspirin or other anti-thrombotics.49 New quality measures that may impact patients with stroke are being phased in during 2017 to 2019, including (1) all-cause unplanned admissions for patients with multiple chronic conditions, (2) documentation of current medications, and (3) medication reconciliation post-discharge.50 The implementation of these measures may increase the impact of MSSP on care transitions and post-acute care. These positive early results in the first cohort of the MSSP suggest further study is warranted.
There are several limitations of our study. MSSP provided a pathway for gradually assuming risk for nascent ACO systems, and these early results may not reflect the potential impact of systemic improvements that require years to implement fully. While the short pre-period available in these data is a limitation, the lack of significant differences in pre-trends in combination with prior studies demonstrating similar trends between MSSP versus not supports the use of the DD design in this context. Our models controlled for health status at discharge, which would underestimate the total effect if acute care quality improved with MSSP despite the high baseline quality of care at participating hospitals. Participation in the GWTG–Stroke registry is voluntary and larger and urban hospitals are more likely to participate, so the generalizability of these results to smaller, more rural institutions is limited.51 Patient ACO alignment is not randomized, and assignment may be correlated with differences between the treatment and control groups that are not captured by the observable characteristics—for example, education level or socioeconomic status—however, models were adjusted for county-level socioeconomic factors to mitigate the potential for bias. Furthermore, adjustment for critical factors like stroke severity to evaluate clinical outcomes improves on claims-only studies of MSSP with limited controls for case mix and severity.
Among patients with mild to moderate ischemic stroke, meaningful reductions in acute care utilization were observed only for ACO-aligned beneficiaries who were also discharged from a hospital initiating MSSP in 2013. This study is one of the first to account for both the hospital MSSP participation and patient ACO alignment for hospitalized patients. Although changes in post-stroke care are inconsistent across MSSP cohorts, ACOs with participating hospitals may benefit stroke patients.
References
McClellan M, Saunders R. Growth Of ACOs And Alternative Payment Models In 2017. Health Affairs Blog. http://www.healthaffairs.org/do/10.1377/hblog20170628.060719/full/. Published 2017. Accessed July 1, 2019.
Muhlestein D, McClellan M. Accountable Care Organizations In 2016: Private And Public-Sector Growth And Dispersion. http://healthaffairs.org/blog/2016/04/21/accountable-care-organizations-in-2016-private-and-public-sector-growth-and-dispersion/. Published 2016. July 1, 2019.
Muhlestein D, Gardner P, William C, de Lisle K. Projected Growth of Accountable Care Organizations. https://leavittpartners.com/whitepaper/projected-growth-of-accountable-care-organizations/ Leavitt Partners 2015. Accessed July 1, 2019.
McClellan M, McKethan AN, Lewis JL, Roski J, Fisher ES. A national strategy to put accountable care into practice. Health Aff (Millwood). 2010;29(5):982–990.
Fisher ES, Shortell SM, Kreindler SA, Van Citters AD, Larson BK. A framework for evaluating the formation, implementation, and performance of accountable care organizations. Health Aff (Millwood). 2012;31(11):2368–2378.
Marcoux RM, Larrat EP, Vogenberg FR. Accountable Care Organizations: An Improvement Over HMOs? P T. 2012;37(11):629–650.
Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. N Engl J Med. 2015;372(10):897–899.
Tai W, Kalanithi L, Milstein A. What can be achieved by redesigning stroke care for a value-based world? Expert Rev Pharmacoecon Outcomes Res. 2014;14(5):585–587.
Johnson BH, Bonafede MM, Watson C. Short- and longer-term health-care resource utilization and costs associated with acute ischemic stroke. Clinicoecon Outcomes Res. 2016;8:53–61.
Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke. 2013;44(12):3429–3435.
Tsai JP, Rochon PA, Raptis S, Bronskill SE, Bell CM, Saposnik G. A prescription at discharge improves long-term adherence for secondary stroke prevention. J Stroke Cerebrovasc Dis. 2014;23(9):2308–2315.
Thrift AG, Kim J, Douzmanian V, et al. Discharge is a critical time to influence 10-year use of secondary prevention therapies for stroke. Stroke. 2014;45(2):539–544.
Bushnell CD, Olson DM, Zhao X, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011;77(12):1182–1190.
Burke JP, Sander S, Shah H, Zarotsky V, Henk H. Impact of persistence with antiplatelet therapy on recurrent ischemic stroke and predictors of nonpersistence among ischemic stroke survivors. Curr Med Res Opin. 2010;26(5):1023–1030.
Prvu Bettger J, Alexander KP, Dolor RJ, et al. Transitional care after hospitalization for acute stroke or myocardial infarction: a systematic review. Ann Intern Med. 2012;157(6):407–416.
Olson DM, Bettger JP, Alexander KP, et al. Transition of care for acute stroke and myocardial infarction patients: from hospitalization to rehabilitation, recovery, and secondary prevention. Evid Rep Technol Assess (Full Rep). 2011(202):1–197.
Hohmann C, Neumann-Haefelin T, Klotz JM, Freidank A, Radziwill R. Adherence to hospital discharge medication in patients with ischemic stroke: a prospective, interventional 2-phase study. Stroke. 2013;44(2):522–524.
Brummel A, Lustig A, Westrich K, et al. Best practices: improving patient outcomes and costs in an ACO through comprehensive medication therapy management. J Manag Care Spec Pharm. 2014;20(12):1152–1158.
Lewis VA, Tierney KI, Fraze T, Murray GF. Care Transformation Strategies and Approaches of Accountable Care Organizations. Med Care Res Rev. 2017 1077558717737841.
Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking Inpatient Clinical Registry Data to Medicare Claims Data Using Indirect Identifiers. Am Heart J. 2009;157(6):995–1000.
Singh GK. Area Deprivation and Widening Inequalities in US Mortality, 1969–1998. In: Am J Public Health. Vol 93.2003:1137–1143.
Smith EE, Shobha N, Dai D, et al. Risk score for in-hospital ischemic stroke mortality derived and validated within the Get With the Guidelines-Stroke Program. Circulation. 2010;122(15):1496–1504.
Christensen EW, Payne NR. Effect of Attribution Length on the Use and Cost of Health Care for a Pediatric Medicaid Accountable Care Organization. JAMA Pediatr. 2016;170(2):148–154.
Myles PS, Shulman MA, Heritier S, et al. Validation of days at home as an outcome measure after surgery: a prospective cohort study in Australia. BMJ Open. 2018.7(8):e015828. doi: https://doi.org/10.1136/bmjopen-2017-015828
Kumamaru H, Judd SE, Curtis JR, et al. Validity of claims-based stroke algorithms in contemporary Medicare data: reasons for geographic and racial differences in stroke (REGARDS) study linked with medicare claims. Circ Cardiovasc Qual Outcomes. 2014;7(4):611–619.
Hartmann A, Rundek T, Mast H, et al. Mortality and causes of death after first ischemic stroke: the Northern Manhattan Stroke Study. Neurology. 2001;57(11):2000–2005.
Levey AS, Stevens LA, Schmid CH, et al. A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med. 2009;150(9):604–612.
Colla CH, Lewis VA, Kao LS, O’Malley AJ, Chang CH, Fisher ES. Association Between Medicare Accountable Care Organization Implementation and Spending Among Clinically Vulnerable Beneficiaries. JAMA Intern Med. 2016;176(8):1167–1175.
Huskamp HA, Greenfield SF, Stuart EA, et al. Effects of Global Payment and Accountable Care on Tobacco Cessation Service Use: An Observational Study. J Gen Intern Med. 2016;31(10):1134–1140.
Liu Y, De A. Multiple Imputation by Fully Conditional Specification for Dealing with Missing Data in a Large Epidemiologic Study. Int J Stat Med Res. 2015;4(3):287–295.
Nyweide DJ, Lee W, Cuerdon TT, et al. Association of Pioneer Accountable Care Organizations vs traditional Medicare fee for service with spending, utilization, and patient experience. Jama. 2015;313(21):2152–2161.
Rosenthal MB, Landrum MB, Robbins JA, Schneider EC. Pay for Performance in Medicaid: Evidence from Three Natural Experiments. Health Serv Res. 2016;51(4):1444–1466.
Kautter J, Pope GC, Leung M, et al. Evaluation of the Medicare Physician Group Practice Demonstration: Final Report. Research Triangle Park, North Carolina: RTI International, Inc;2012.
McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early Performance of Accountable Care Organizations in Medicare. N Engl J Med. 2016;374(24):2357–2366.
Schwartz AL, Chernew ME, Landon BE, McWilliams JM. Changes in Low-Value Services in Year 1 of the Medicare Pioneer Accountable Care Organization Program. JAMA Intern Med. 2015;175(11):1815–1825.
O’Brien EC, Xian Y, Xu H, et al. Hospital Variation in Home-Time After Acute Ischemic Stroke: Insights From the PROSPER Study (Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research). Stroke. 2016;47(10):2627–2633.
Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD. “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
Centers for Medicare and Medicaid Services. Medicare Accountable Care Organizations 2015 Performance Year Quality and Financial Results. https://www.cms.gov/newsroom/fact-sheets/medicare-accountable-care-organizations-2015-performance-year-quality-and-financial-results. Published 2016. Accessed July 1, 2019.
Kaufman BG, Spivack BS, Stearns SC, Song PH, O’Brien EC. Impact of Accountable Care Organizations on Utilization, Care, and Outcomes: A Systematic Review. Med Care Res Rev. 2017 1077558717745916.
McWilliams JM, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in Postacute Care in the Medicare Shared Savings Program. JAMA Intern Med. 2017;177(4):518–526.
Winblad U, Mor V, McHugh JP, Rahman M. ACO-Affiliated Hospitals Reduced Rehospitalizations From Skilled Nursing Facilities Faster Than Other Hospitals. Health Aff (Millwood). 2017;36(1):67–73.
Colla CH, Lewis VA, Kao LS, O’Malley AJ, Chang CH, Fisher ES. Notice of Retraction and Replacement: Colla et al. Association between Medicare accountable care organization implementation and spending among clinically vulnerable beneficiaries. JAMA Internal Medicine. 2016;176(8):1167–1175. JAMA Intern Med. 2017.
Schoenfeld AJ, Sturgeon DJ, Blucher JA, Haider AH, Kang JD. Alterations in 90-Day Morbidity, Mortality and Readmission Rates Following Spine Surgery in Medicare Accountable Care Organizations (2009-2014). Spine J. 2018.
Colla CH, Lewis VA, Tierney E, Muhlestein DB. Hospitals Participating In ACOs Tend To Be Large And Urban, Allowing Access To Capital And Data. Health Aff (Millwood). 2016;35(3):431–439.
Song S, Fonarow GC, Olson DM, et al. Association of Get With The Guidelines-Stroke Program Participation and Clinical Outcomes for Medicare Beneficiaries With Ischemic Stroke. Stroke. 2016;47(5):1294–1302.
Alcusky M, Ulbrict CM, Lapane KL. Post-Acute Care Setting, Facility Characteristics, and Post-Stroke Outcomes: A Systematic Review. Arch Phys Med Rehabil. 2017.
Fang MC, Perraillon MC, Ghosh K, Cutler DM, Rosen AB. Trends in Stroke Rates, Risk, and Outcomes in the United States, 1988–2008. Am J Med. 2014;127(7):608–615.
McWilliams JM, Chernew ME, Landon BE. Medicare ACO Program Savings Not Tied To Preventable Hospitalizations Or Concentrated Among High-Risk Patients. Health Affairs. 2017: 36(12) https://doi.org/10.1377/hlthaff20170814.
RTI International. Accountable Care Organization 2014 Program Analysis Quality Performance Standards Narrative Measure Specifications. Report for Centers for Medicare & Medicaid Services. 2014. https://www.healthreform.ct.gov/ohri/lib/ohri/work_groups/quality/2014-09-03/aco_narrative_measures_specs_1.pdf. Accessed July 1, 2019.
Centers for Medicare & Medicaid Services. Quality Measure Benchmarks for the 2016 and 2017 Reporting Years. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/MSSP-QM-Benchmarks-2016.pdf. Published 2016. Accessed July 1, 2019.
Reeves MJ, Fonarow GC, Smith EE, et al. Representativeness of the Get With The Guidelines-Stroke Registry: comparison of patient and hospital characteristics among Medicare beneficiaries hospitalized with ischemic stroke. Stroke. 2012;43(1):44–49.
Funding
Internal funding for this study was provided by the Duke Clinical Research Institute. The GWTG–Stroke program is currently supported in part by a charitable contribution from Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership and the American Heart Association Pharmaceutical Roundtable. GWTG–Stroke has been funded in the past through support from Boehringer-Ingelheim and Merck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
ECO: Research grants from BMS, Novartis, Janssen, and GSK
GCF: Research Patient Centered Outcomes Research Institute, Consultant to Janssen
YX: Research funding from the American Heart Association, Daiichi Sankyo, Janssen Pharmaceuticals, and Genentech. Honorarium from Brain Canada
All remaining authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 73 kb)
Rights and permissions
About this article
Cite this article
Kaufman, B.G., O’Brien, E.C., Stearns, S.C. et al. The Medicare Shared Savings Program and Outcomes for Ischemic Stroke Patients: a Retrospective Cohort Study. J GEN INTERN MED 34, 2740–2748 (2019). https://doi.org/10.1007/s11606-019-05283-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05283-1