Abstract
Background
Uncontrolled hypertension contributes to disparities in cardiovascular outcomes. Patient intervention strategies informed by behavioral economics and social psychology could improve blood pressure (BP) control in disadvantaged minority populations.
Objective
To assess the impact on BP control of an intervention combining short-term financial incentives with promotion of intrinsic motivation among highly disadvantaged patients.
Design
Randomized controlled trial.
Participants
Two hundred seven adults (98% African American or Latino) aged 18 or older with uncontrolled hypertension attending Federally Qualified Health Centers.
Intervention
Six-month intervention, combining financial incentives for measuring home BP, recording medication use, BP improvement, and achieving target BP values with counseling linking hypertension control efforts to participants’ personal reasons to stay healthy.
Main Measures
Primary outcomes: percentage achieving systolic BP (SBP) < 140 mmHg, percentage achieving diastolic BP (DBP) < 90 mmHg, and changes in SBP and DBP, all after 6 months. Priority secondary outcomes were SBP < 140 mmHg, DBP < 90 mmHg, and BP change at 12 months, 6 months after the intervention ended.
Key Results
After 6 months, rates of achieving target BP values for intervention and control subjects respectively was 57.1% vs. 40.2% for SBP < 140 mmHg (adjusted odds ratio (AOR) 2.53 (1.13–5.70)), 79.8% vs 70.1% for DBP < 90 mmHg (AOR 2.50 (0.84–7.44)), and 53.6% vs 40.2% for achieving both targets (AOR 2.04 (0.92–4.52)). However, at 12 months, the groups did not differ significantly in these 3 measures: 39.5% vs 35.0% for SBP (AOR 1.20 (0.51–2.83)), 68.4% vs 75.0% for DBP (AOR 0.70 (0.24–2.09)), and 35.5% vs 33.8% for both (AOR 1.03 (0.44–2.42)). Change in absolute SBP and DBP did not differ significantly between the groups at 6 or 12 months. Exploratory post hoc analysis revealed intervention benefit only occurred among individuals whose providers intensified their regimens, but not among those with intensification but no intervention.
Conclusions
The intervention achieved short-term improvement in SBP control in a highly disadvantaged population. Despite attempts to enhance intrinsic motivation, the effect was not sustained after incentives were withdrawn. Future research should evaluate combined patient/provider strategies to enhance such interventions and sustain their benefit.
Trial Registration
NCT01402453; http://clinicaltrials.gov/show/NCT01402453
Similar content being viewed by others
INTRODUCTION
Uncontrolled hypertension remains a substantial societal challenge. Its asymptomatic nature and delay in adverse complications reduce risk perception while medication cost and fear of side-effects deter treatment-seeking behavior.1 Interventions to improve hypertension control have emphasized screening,2,3,4,5,6 patient awareness of hypertension’s consequences,7 adjusting dosing schedules and packaging, other measures to improve adherence,8,9,10,11,12,13,14 physician awareness of need to treat,15, 16 and physician incentives to overcome therapeutic inertia and achieve recommended blood pressure (BP) treatment targets.17 The most successful interventions have been pharmacist team-based programs in large integrated health systems.18,19,20 While hypertension control in the USA has improved, BP remains > 140/90 mmHg (the standard definition of uncontrolled hypertension) among half of affected individuals.21 This challenge is especially pronounced among racial/ethnic minority populations, who are at greater risk for uncontrolled hypertension and its complications, and among socioeconomically disadvantaged persons facing many competing demands and limited resources.22
Financial incentives are a potentially promising approach to improving hypertension control. Provider incentives have been adopted widely in quality improvement efforts.23 In theory, financial incentives might help patients focus attention on treatment initially, but they may not have enduring impact on chronic conditions requiring long-term treatment if they cannot be continued for extensive periods.24
We hypothesized that monetary payments, designed using behavioral economics principles, would strongly incentivize behavior change and hypertension control among economically disadvantaged individuals, particularly if combined with an additional intervention element designed to prompt attribution of behavior changes to internal motivation—in this case, personal values, priorities, goals, and needs25, 26 that might also increase the chances of sustaining the effect after the intervention ended.
To test this hypothesis, we conducted a randomized trial of a patient-centered intervention, combining financial incentives with intrinsic motivation tools, to improve hypertension control among adults attending Federally Qualified Health Center clinics (FQHCs). For both the intervention and comparison groups, we provided educational materials, home BP monitors (and training in their use), and monthly clinic BP checks. Intervention participants also received contingent payments and an “identity intervention” designed to increase intrinsic motivation to achieve and sustain hypertension control.
METHODS
Design and Setting
The two-arm randomized controlled trial was conducted in three Los Angeles area FQHC sites serving indigent patients without insurance or with publicly provided insurance who were overwhelmingly Latino and African American.
Participants
The target population, clinic patients aged ≥ 18 years with uncontrolled hypertension, were recruited by waiting room signage and clinic staff. We screened for systolic BP (SBP) > 149 mmHg (10 mmHg above the target level) and/or diastolic BP (DBP) > 94 mmHg (5 mmHg above the target level) in two steps. After patients rested 5 min in a quiet room, trained research personnel measured seated BP from the dominant arm (at heart level) with an appropriately sized cuff using a validated automated oscillometric sphygmomanometer (Welch Allyn, Series 52,000, Arden, NC) to eliminate digit preference and minimize inter-observer variability. We discarded the first two of six readings, averaging the final four.27, 28 Participants averaging SBP > 149 mmHg and/or DBP > 94 mmHg were invited to return within 1 week for a second screening. We invited those remaining abnormal to provide written informed consent in Spanish or English for trial participation.
Study Procedures
We randomly allocated consenting participants 1:1 to intervention and comparison groups. Research staff did not interact with participants’ clinicians regarding BP control after randomization nor inform them of condition assignment. Both groups were administered in-person questionnaires at baseline and 6 and 12 months. Structured response items included demographic characteristics, clinical history including history of hypertension and hypertension treatment, current medications, health status (measured with the SF-12),29 self-efficacy (a 5-item version of the Medication Adherence Self-Efficacy Scale (MASES) adapted for use in hypertension,30, 31 Patient Activation Measure score (the PAM-6),32 6 items measuring social support (drawn from Medical Outcomes Study and the Lubben Social Network Scale-6),33, 34 access to care (6 items), and unmet needs (2 items derived from the HCSUS study).35 Intervention participants only were administered items to identify potential reasons to stay healthy or live longer (e.g., relationships, responsibilities to others, life goals and activities they enjoy) and were asked to provide pictures of loved ones, favored activities or representations of goals that we incorporated into personalized calendars for the identity (intrinsic motivation) manipulation. We asked members of both groups to return monthly for 6 months, and at months 9 and 12 for BP checks. Enrollment began in October 2011; follow-up was completed in January 2014. We provided both groups with digital home BP monitors (Lifesource or Meridian) that recorded measurements and dates, training by study staff in their use, and encouragement to use them, but only intervention participants received financial incentives for doing so (if they brought the monitor to the visit).
Payments to Participants
We offered intervention participants a combination of fixed payments, contingent payments, and lotteries: $10 per visit at months 1–6 for returning, and additional payments if they brought in their personalized calendar ($5) and BP monitor ($5). At each visit through 6 months, we also provided contingent payments of $2 per mm of SBP and DBP improvement from their values at study entry, up to achieving target clinic BP values (SBP < 140 mmHg or DBP < 90 mmHg) to a maximum of $50 per visit; if visit BP was in the target range, minimum payment was $30. The target level of < 140/90 was consistent with JNC 7’s Guideline goal for office BP, operative during the study period.36 To avoid inducing inappropriate measures to lower BP, no payment was given for improvement beyond BP 139/89 mmHg or for total (SBP plus DBP) improvement of > 25 mmHg from baseline values. Finally, because people tend to value lotteries offering low probability of reward more than the reward’s expected value37, making them cost-effective extrinsic motivators for complying with health-related behaviors,24 intervention participants also received one chance to draw a lottery card during each intervention visit (months one through 6) for each of 3 desired health behaviors: (1) recording hypertension medication use on the calendar on ≥ 50% of days in the preceding month, (2) measuring their BP on ≥ 50% of days in the month, and (3) achieving BP goals or improved BP relative to the previous visit. Lottery cards had values of $0 (83%), $20 (10%), $50 (5%), or $100 (2%). Winnings were combined with payments for BP improvement and other incentives and were provided in gift cards (additional detail in the online Appendix).
Comparison group participants received $20 at each study visit months 1 through 6 to assure adequate and comparable follow-up, but no contingent or lottery payments. Both groups received additional payments for completing study questionnaires and $20 per visit for returning for BP checks at 9 and 12 months (after the 6-month intervention had ended).
Identity Intervention
The identity intervention was designed to promote internalization of motivation for controlling hypertension by associating healthy behaviors with personal values and needs.25 We provided participants with personalized calendars, containing images of loved ones, activities or life goals associated with being healthy that they identified, to use daily for recording medication use. A research associate met with intervention participants at months 1 through 6, prompting participants to talk about what improved BP would mean for loved ones, goals, activities, and responsibilities. When participants received lottery tickets and/or contingent payments for effort (measuring BP, taking medicine, bringing in calendars, and BP monitors) or results (improved BP), the research associate prompted them to relate that to reasons they identified for staying healthy or living longer (e.g., “so that you can dance at your daughter’s wedding,” or “…care for loved ones.”).26
Data on Hypertension Treatment
We abstracted clinic records and collected self-report information about hypertension medications and regimen changes or intensification from 167 of 173 participants (97%) completing 6 months follow-up and from 153 of 158 (97%) at 12 months, in addition to baseline self-reports.
Statistical Analysis
The study’s co-primary outcomes were intervention efficacy on SBP control rate and on DBP control rate (measured as group differences in the percentage achieving in-clinic BP target values after 6 months (SBP < 140 mmHg, DBP < 90 mmHg)), and absolute SBP and DBP reduction (although the intervention was structured only to lower BP to the point of hypertension control (139/89) and not to reward > 25 mm of total SBP plus DBP reduction). The study’s priority secondary outcome was sustainability of the intended intervention effect. This was measured by group differences in SBP and DBP control rates at 12 months (6 months after the intervention ended). We used mixed effects logistic regression models to assess these key outcomes and linear mixed effects models, with baseline BP as a key covariate, to test for intervention effects on SBP and DBP at 6 and 12 months. We assessed differences in patient-reported outcomes, using analysis of covariance (ANCOVA) models adjusting for baseline values. Our target sample size of 262, assuming standard deviations of 20%/15% for SBP/DBP and a completion rate of 75%, would have provided .80 power at the .05 significance level (two-sided test) to detect control rate differences of 60% vs 40% and .87 power to detect differences of 40% vs 20%. Our final sample (limited by clinic patient availability and study resources) was 207; the completion rate was 87.0% of the original target at 6 months and 80.4% at 12 months, for power respectively of .75 to .82 and .71 to .78 (online Appendix Table 1). We also conducted exploratory post hoc subgroup analyses of potential effects of nonrandom drug regimen intensification on group differences in BP and related outcomes. Intensification was defined as an increased dose of an existing hypertension medication, adding a new medication, or substituting a more potent medication. P values of < 0.05 were considered statistically significant. All analyses were performed using SAS v. 9.3 (SAS Institute Inc., Cary, NC).
The UCLA Institutional Review Board approved the research protocol.
RESULTS
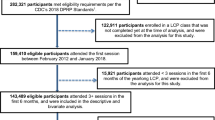
Cohort recruitment and retention are shown in Figure 1. Among 999 clinic patients initially screened, 531 did not meet the BP screening criteria or did not return for the second screening. Of 468 completing the second screening, 220 met BP eligibility criteria, of whom 207 consented and were enrolled: 103 randomly allocated to the intervention group and 104 to the comparison group. Eleven participants were lost to follow-up immediately after enrollment, and 38 others over the next 12 months. Thus, follow-up was 82.6% at 6 months and 76.3% at 12 months. Attrition did not differ significantly between study groups (P > 0.80). Of 49 participants not completing the study, 11 moved away from Southern California and two expired (one in each study arm). Excluding those lost immediately after enrollment, subjects attended 84.2% of intervention visits and 86.3% of control visits during the 6-month intervention. Participant payments at visits in months 1 to 6 averaged $74.43 (including $20.85 for lotteries and $31.32 for BP improvement) for intervention attendees and $23.33 for control attendees. Total study payments averaged $424.72 among intervention participants, including those lost to follow-up (range $40 to $846) (online Appendix).
The groups were well-matched on most baseline characteristics (Table 1), including rates of prior hypertension diagnosis (P = 0.21), prior hypertension treatment (P = 0.84), and current numbers of hypertension medicines (P = 0.39). Overwhelmingly Black or Latino, and having very low household incomes, most were immigrants and 2 in 5 were diabetics. Participants reported severe resource constraints: 41.2% had gone without health care when needing money for food, clothing or housing; 21.9% had forgone food, clothing or housing to pay for health care.
Subjects entered the trial with marked systolic hypertension and less marked diastolic hypertension, representing stage 2 hypertension (significantly elevated BP requiring medication therapy plus lifestyle modification) by both JNC 7 and 2017 ACC/AHA guideline criteria.36, 38 Mean baseline BP was 162.3(± 14.5)/91.6(± 14.2) mmHg among intervention group participants and 161.8(± 14.1)/88.7(± 12.8) mmHg among comparison group participants.
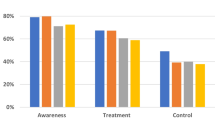
Logistic regression revealed that intervention participants were significantly more likely to achieve SBP < 140 mmHg.at 6 months (57.1%, vs. 40.2%, (P = 0.02), controlling for age, gender, education, race/ethnicity, born in the USA, and diabetes (Table 2). At 12 months (6 months after the intervention ended), 39.5% of intervention participants and 35.0% of comparison participants had normal range SBP (P = 0.68) (Table 2). DBP fell by lesser amounts: nearly half were normal at baseline and over 70% at 6 and 12 months. There were nonsignificant trends toward greater control in intervention participants at 6 months of DBP (79.8%, vs. 70.1%, P = 0.10), and of both SBP and DBP (53.6% vs. 40.2%, P = 0.08), but not at 12 months for either of these outcomes (Table 2). Mean BP fell to 141.9(± 16.6)/81.1(± 13.9) mmHg in intervention participants vs. 146.1(± 18.9)/80.4(± 15.0) mmHg in the comparison group at 6 months (P = 0.18 by linear regression of SBP difference in differences, controlling for these same variables). Differences in reduction of SBP at 12 months and DBP at 6 and 12 months were not significant (Table 3). Both intention-to-treat and completer analyses, with and without the same adjustments, yielded similar results (data not reported).
Intervention participants significantly improved relative to comparison participants in physical health (SF-12) (P = 0.008) at 6 months, and in self-efficacy scores at 12 months (P = 0.03) (Table 4). Intervention subjects’ BP monitors recorded BP measurements on ≥ 15 days in the month before 77.6% of all visits in months 1 to 6.
The exploratory post hoc analysis found that improved SBP control in intervention relative to comparison participants was highly significant in the subset of subjects whose regimens were intensified (67% among intervention participants vs. 35% among comparison participants, P = 0.02), but not among those whose regimens were not intensified (53% vs 46% respectively, P = 0.51). At 6 months, mean SBP fell by 29 mmHg in intensified intervention participants vs 18 mmHg in intensified comparison participants (P = 0.02); among those not intensified, SBP fell 15 mmHg and 16 mmHg, respectively (P = 0.89). Also, the intervention effect on self-efficacy scores was limited to participants in whom drug regimens had been intensified (online Appendix Table 2). No analyses revealed significant benefit of intensification overall (without respect to experimental group assignment).
DISCUSSION
To address the challenging problem of hypertension control among disadvantaged populations,39 we completed a randomized trial of a novel behavior theory-based intervention combining monetary incentives with intrinsic motivation tools to promote specific patient behaviors (self-measurement of BP, medication adherence, and clinic visits) and BP reduction, to achieve and sustain recommended BP targets. In our severely disadvantaged cohort of Latino and African American safety-net clinic patients, we found a significant intervention effect on SBP control after 6 months, with trends in control of DBP and of both SBP and DBP that fell short of being statistically significant: a clinic SBP of < 140 mmHg was achieved by 17% more of intervention participants than comparison participants. The intervention effect did not persist after both components of the intervention were withdrawn. This finding compares favorably with a recent study of Medicaid patients with hypertension, in which financial incentives alone did not affect BP control, although most patients in that study were normotensive at study entry.40
At first glance, the intervention effect seems modest: absolute SBP improved only about a nonsignificant 4 mmHg more in intervention than comparison participants, but we note that the intervention was designed to reach the target level of hypertension control and did not reward improvement beyond that level. The 57% of intervention group patients achieved SBP control is less than the > 80% achieved in Kaiser-Permanente’s population (with providers implementing a system-wide BP medication intensification protocol20), but our manipulation was strictly patient-centered, with no intervention on care intensity, quality, or structure. This said, in our population, the SBP control achieved by the intervention is an important accomplishment for several reasons. Typical of FQHCs, participants were largely unemployed, impoverished, and had low educational attainment. Many were recent immigrants. They had high rates of serious comorbid conditions that compete with hypertension for theirs and their providers’ attention, and severely constrained resources for allocation to health care, which also may inhibit cognitive resources to cope with disease.41 Such populations are poorly represented in most hypertension trials. In such high-risk individuals, even modest BP improvements can substantially reduce risk of complications and death.
The positive intervention effect occurred despite substantial BP improvement in comparison participants, a common finding in hypertension trials, due to regression to the mean42 and the Hawthorne effect of study participation.43 Moreover, in this trial, the control condition was an active comparator, receiving financial incentives (to assure adequate follow-up) for frequent BP checks, and training and equipment for BP self-measurement, which enhances medication adherence.44 These interventions likely constituted a significant behavioral intervention.
Monetary payment can induce short-term (and sometimes longer-term) health behavior changes, such as smoking cessation and healthy eating45, 46 but impact on medical conditions requiring long-term medication use is mixed47,48,49,50,51,52 For example, use of lotteries increased short-term warfarin adherence, but the effect disappeared after the incentive was removed.24 Sustained benefit in chronic disease care may require continued payments (particularly in populations with many competing demands and challenges), or additional interventions to promote patient attribution of behavior change to internal motivation,26 or to influence clinician behavior.50 Our incentive payments were substantial relative to participants’ very low incomes (averaging > 4% of annual income). This may have enhanced their salience. An undermining or “crowding out” effect of external rewards on intrinsic motivation, identified in some social psychology and economics studies,53, 54 is heterogeneous and has not been reported in medical care studies that have looked for such effects52, 55,56,57 In our study, the initial effect on SBP control was not sustained after the intervention ended, even though we combined the external motivator (contingent and lottery payments) with an internal one. Improvement at 12 months in self-efficacy for BP medication adherence could suggest more enduring effects of the intervention on attitudes to controlling their BP, even if they did not translate into sustained improved BP control, but that finding should be interpreted cautiously, since self-efficacy did not differ at 6 months, and intrinsic motivation was not measured directly.
Besides achieving short-term SBP improvement in high-risk, highly disadvantaged minority patients by deploying a theory-based behavioral intervention along with financial incentives, the study’s strengths include high cohort retention and rigorous assessment of BP outcomes.
Our study also has important limitations. We bundled two interventions to maximize chances of demonstrating an effect. Differentiating their effects would require more than two study arms, exceeding our budgetary constraints. An effective, combined intervention may prove clinically useful in very challenging populations, even though additional studies would be needed to assess whether fewer intervention elements would suffice. The study was powered to detect, at the P = 0.05 confidence level, differences in BP normalization rates of about 20%. Powering the study to detect smaller differences potentially beneficial to health would require a larger sample size per study arm than our budget allowed. We note further that participants and study personnel could not be blinded to condition assignment, though assignment information was not shared with participants’ medical providers and clinic staff. Without engaging providers and clinic staff in the intervention or in implementing a clinic-wide team-based BP medication intensification protocol (as in the recent SBP Intervention Trial58), the effect on hypertension control was modest and not sustained after the intervention ended.
The post hoc analysis findings on medication intensification must be interpreted cautiously; it was not planned a priori, and intensification was not randomized. The associations observed suggest that patient interventions to improve and sustain BP control may require additional measures to assure that providers respond to uncontrolled BP with guideline-directed regimen adjustments.
Despite these limitations, we found that behaviorally informed incentives plus an intervention designed to increase intrinsic motivation to sustain good health increased the likelihood of achieving SBP normalization in a disadvantaged minority population. Additional refinements are needed to develop a more potent and sustainable patient-centered intervention that coordinates intrinsic and extrinsic patient motivators with improvement in quality and intensity of medical care.
Future studies should investigate the impact of intensifying and/or extending the identity intervention, extending the period of provision of financial incentives, or both, and whether interventions targeting behavior of both patients and providers are more effective than those directed at either one alone. For example, a study could assess coupling a patient-centered behavioral intervention in highly disadvantaged patients with a system intervention to overcome physician inertia in intensifying BP regimens, as was accomplished using pharmacists in a recent trial among black male barber shop clients.59 While patient and provider interventions in hypertension care are somewhat costly, these costs are likely to be dwarfed by reduction of downstream costs of treating hypertensive complications—non-fatal stroke, myocardial infarction, heart failure, end-stage kidney disease—and the social and economic costs of higher morbidity.
References
Victor RG, Leonard D, Hess P, et al. Factors Associaed with Hypertension Awareness, Treatment, and Control in Dallas County, Texas, Arch Intern Med. 2008;168(12):1285–93.
Wilber JA, Barrow JG. Hypertension--a community problem. Am J Med. 1972;52(5):653–63.
Stamler J, Stamler R, Riedlinger WF, Algera G, Roberts RH. Hypertension screening of 1 million Americans. Community Hypertension Evaluation Clinic (CHEC) program, 1973 through 1975. JAMA. 1976;235(21):2299–306.
Blood pressure studies in 14 communities. A two-stage screen for hypertension. JAMA. 1977;237(22):2385–91.
Radice M, Alberti D, Alli C, Avanzini F, Di Tullio M, Mariotti G, et al. Long-term efficacy of screening for hypertension in a community. J Hypertens. 1985;3(3):255–9.
Cooke CJ, Meyers A. The Role of Community Volunteers in Health Interventions: a Hypertension Screening and Follow-Up Program. Am J Public Health. 1983;73(2):193–4.
Ambrosio GB, Strasser T, Dowd JE, Tuomilehto J, Nissinen A, Froment A, et al. Effects of Interventions on Community Awareness and Treatment of Hypertension: Results of a WHO Study. Bull World Health Organ. 1988;66(1):107–13.
Baird MG, Bentley-Taylor MM, Carruthers SG, Dawson KG, Laplante LE, Larochelle P, et al. A Study of Efficacy, Tolerance and Compliance of Once-Daily Versus Twice-Daily Metoprolol (Betaloc) in Hypertension. Betaloc Compliance Canadian Cooperative Study Group. Clin Invest Med. 1984;7(2):95–102.
Becker LA, Glanz K, Sobel E, Mossey J, Zinn SL, Knott KA. A Randomized Trial of Special Packaging of Antihypertensive Medications. J Fam Pract. 1986;22(4):357–61.
Brown BG, Bardsley J, Poulin D, Hillger LA, Dowdy A, Maher VM, et al. Moderate Dose, Three-Drug Therapy with Niacin, lovastatin, and Colestipol to Reduce Low-Density Lipoprotein Cholesterol <100 mg/dl in Patients with Hyperlipidemia and Coronary Artery Disease. Am J Cardiol. 1997;80(2):111–5.
Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, et al. A Telecommunications System for Monitoring and Counseling Patients with Hypertension. Impact on Medication Adherence and Blood Pressure Control. Am J Hypertens. 1996;9(4 Pt 1):285–92.
Girvin B, McDermott BJ, Johnston GD. A Comparison of Enalapril 20 mg Once Daily versus 10 mg Twice Daily in Terms of Blood Pressure Lowering and Patient Compliance. J Hypertens. 1999;17(11):1627–31.
Haynes RB, Sackett DL, Gibson ES, Taylor DW, Hackett BC, Roberts RS, et al. Improvement of Medication Compliance in Uncontrolled Hypertension. Lancet. 1976;1(7972):1265–8.
Johnson AL, Taylor DW, Sackett DL, Dunnett CW, Shimizu AG. Self-recording of Blood Pressure in the Management of Hypertension. Can Med Assoc J. 1978;119(9):1034–9.
Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National Study of Physician Awareness and Adherence to Cardiovascular Disease Prevention Guidelines. Circulation. 2005;111(4):499–510.
Hagemeister J, Schneider CA, Barabas S, Schadt R, Wassmer G, Mager G, et al. Hypertension Guidelines and Their Limitations--the Impact of Physicians' Compliance as Evaluated by Guideline Awareness. J Hypertens. 2001;19(11):2079–86.
Millett C, Gray J, Bottle A, Majeed A. Ethnic Disparities in Blood Pressure Management in Patients with Hypertension after the Introduction of Pay for Performance. Ann Fam Med. 2008;6(6):490–6.
Tsuyuki RT, Houle SKD, Charrois TL, Kolber MR, Rosenthal MM, Lewanczuk R, et al. A Randomized Trial of the Effect of Pharmacist Prescribing on Improving Blood Pressure in the Community: The Alberta Clinical Trial in Optimizing Hypertension (RxACTION). Circulation. 2015;132(2):93–100.
Victor RG. Expanding Pharmacists’ Role in the Era of Health Care Reform. Am J Health Syst Pharm. 2012;69(22):1959.
Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved Blood Pressure Control Associated with a Large-Scale Hypertension Program. JAMA. 2013;310(7):699–705.
Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;386(9995):801–12.
Mullainthan S, Shafir E. Scarcity: Why Having so Little Means so Much. New York, Times Books, Henry Holt and Company, 2013.
Houle SK, McAlister FA, Jackevicius CA, Chuck AW, Tsuyuki RT. Does Performance-Based Remuneration for Individual Health Care Practitioners Affect Patient Care?: A Systematic Review. Ann Intern Med. 2012;157(12):889–99.
Volpp KG, Loewenstein G, Troxel AB, Doshi J, Price M, Laskin M, et al. A Test of Financial Incentives to Improve Warfarin Adherence. BMC Health Serv Res. 2008;8:272. doi: https://doi.org/10.1186/1472-6963-8-272
Ryan RM, Deci EL. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am Psychol. 2000;55(1):68–78.
Cialdini R. B., Eisenberg N. E., Green B. L., Rhoads K., Bator R. Undermining the Undermining Effect of Reward on Sustained Interest. J Appl Soc Psychol. 1998;28(3):249–63.
Victor RG, Haley RW, Willett DL, Peshock RM, Vaeth PC, Leonard D, et al. The Dallas Heart Study: a Population-Based Probability Sample for the Multidisciplinary Study of Ethnic Differences in Cardiovascular Health. Am J Cardiol. 2004;93(12):1473–80.
Victor RG, Ravenell JE, Freeman A, et al. Effectiveness of a Barber-Based Intervention for Improving Hypertension Control in Black Men: The barber-1 study: a Cluster Randomized Trial. Arch Intern Med. 2011;171(4):342–50.
Cote I, Gregoire JP, Moisan J, Chabot I. Quality of Life in Hypertension: the SF-12 Compared to the SF-36. Can J Clin Pharmacol = Journal Canadien de Pharmacologie Clinique. 2004;11(2):e232–8.
Fernandez S, Chaplin W, Schoenthaler AM, Ogedegbe G. Revision and Validation of the Medication Adherence Self-Efficacy Scale (MASES) in Hypertensive African Americans. J Behav Med. 2008;31(6):453–62.
Warren-Findlow J, Seymour RB, Brunner Huber LR. The Association Between Self-Efficacy and Hypertension Self-Care Activities Among African American Adults. J Commun Health. 2012;37(1):15–24.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv Res. 2004;39(4 Pt 1):1005–26.
Crooks VC, Lubben J, Petitti DB, Little D, Chiu V. Social Network, Cognitive Function, and Dementia Incidence Among Elderly Women. Am J Public Health. 2008;98(7):1221–7.
Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The Eight-Item Modified Medical Outcomes Study Social Support Survey: Psychometric Evaluation Showed Excellent Performance. J Clin Epidemiol. 2012;65(10):1107–16.
Cunningham WE, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, et al. The Impact of Competing Subsistence Needs and Barriers on Access to Medical Care for Persons with Human Immunodeficiency Virus Receiving Care in the United States. Med Care. 1999;37(12):1270–81.
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, Maryland, United States Department of Health Services, National Institutes of Health, National Heart, Lung, and Blood Institute Publication No. 04–5230, 2004.
Tversky A, Kahneman D. Advances in Prospect Theory: Cumulative representation of Uncertainty. J Risk Uncertain. 1992;5(4):297–323.
American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2017, 23976; https://doi.org/10.1016/j.jacc.2017.07.74. Correction J Am Coll Cardiol 2018;71:e127–248.5
Worldwide Trends in Blood Pressure from 1975 to 2015: a Pooled Analysis of 1479 Population-Based Measurement Studies with 19·1 Million Participants. Lancet. 2017;389(10064):37–55.
VanEpps EM, Troxel AB, Villamil E, Saulsgiver KA, Zhu J, Chin J-Y, et al. Financial Incentives for Chronic Disease Management: Resultd and Limitations of 2 Randomized Clinical Trials With New York Medicaid Patioents. Am J Health Promot 2018;32(7):1537–43.
Mani A, Mullainathan S, Shafir E, Zhao J. Poverty Impedes Cognitive Function. Science 2013;341(6149):976–80.
Pocock SJ, Bakris G, Bhatt DL, Brar S, Fahy M, Bersh BJ. Regression to the mean in SYMPLICITY HTN-3. J Am Coll Cardiol. 2016;68(18):2016–2025.
Wilhelm M, Winkler A, Rief W, Doerning BK. Effect of placebo groups on blood pressure in hypertension: a meta-analysis of beta-blocker trials. J Am Soc Hypertension 2016;10(12):917–929.
Souza WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of Blood Pressure for Control of Blood Pressure Levels and Adherence to Treatment. Arq Bras Cardiol. 2012;98(2):167–74.
Cahill K, Hartmann-Boyce J, Perera R. Incentives for smoking cessation. Cochrane Database Syst Rev. 2015;(5):CD004307.
Mantzari E, Vogt F, Shemilt I, Wei Y, Higgins JPT, Marteau TM. Personal financial incentives for changing habitual health-related behaviors: A systematic review and meta-analysis. Prev Med. 2015;75:75–85.
Thirumurthy H. Asch Da Volpp K: The uncertain effect of financial incentives to improve health behaviors. JAMA. 2019;25. https://doi.org/10.1001/jama.2019.2560.
Volpp KG, Troxel AB, Mehta SJ et al. Effect of electronic reminders, financial incentives, and social support on outcomes after myocardial infarction. JAMA Intern Med. 2017;177(8):1093–1101
Liu T, Volpp KG, Asch DA. The association of financial incentives for low density lipoprotein cholesterol reduction with patient activation and motivation. Prev Med Rep. 2019;14:100841. doi: https://doi.org/10.1016/j.pmedr.2019.100841.
Asch DA, Troxel AB, Stewart WF et al. Effect of financial incentives to physicians, patients, or both on lipid levels. A randomized trial. JAMA. 2015;314(18):1926–35
Sen AP, Sewell TB, Riley EB et al. Financial incentives for home-based health monitoring. A randomized trial. J Gen Intern Med. 2014; 29(5):770–7
Czaicki NL, Dow WH, Njau PF, McCoy SI. Do incentives undermine intrinsic motivation? Increases in motivation within an incentive-based intervention for people living with HIV in Tanzania. PLOS One. 2018. Available at: https://doi.org/10.1371/journal.pone.0196616. Accessed July 10, 2019.
Promberger M, Marteau TM. When do financial incentives reduce intrinsic motivation? Comparing behaviors in psychological and economic literature. Health Psychol. 2013;32(9):950–7
Murayama K, Matsumoto M, Izuma K, Matdsumoto K. Neural basis of the undermining effect of monetary reward on intrinsic motivation. PNAS. 2010; 107(49):20911–6
Shah N. Introduction. In Cohen IG, Lynch HF, Robertson CT (eds). Nudging Health: Health Law and Behavioral Economics. Baltimore, Johns Hopkins University Press 2016:187–9.
Underhill K. Extrinsic incentives, intrinsic motivation, and motivational crowding out in health law and policy. In Cohen IG, Lynch HF, Robertson CT (eds). Nudging Health: Health Law and Behavioral Economics. Baltimore, Johns Hopkins University Press 2016:190–201.
Sen AP, Hffman D, Loewenstein G, Asch DA, Kullgren JT, Volpp KG. Do financial incentives reduce intrinsic motivation for weight loss? Underhill K. Extrinsic incentives, intrinsic motivation, and motivational crowding out in health law and policy. In Cohen IG, Lynch HF, Robertson CT (eds). Nudging Health: Health Law and Behavioral Economics. Baltimore, Johns Hopkins University Press 2016:202–16.
Drawz PE, Pajewski NM, Bates JT, et al. Effect of Intensive Versus Standard Clinic-Based Hypertension Management on Ambulatory Blood Pressure: Results From the SPRINT Ambulatory Blood Pressure Study. Hypertension. 2017;69(1):42–50.
Victor RG, Lynch K, Li N, et al. A Cluster-Randomized Trial of Blood-Pressure Reduction in Black Barbershops. N Engl J Med. 2018;378(14)1291–1301.
Acknowledgments
Dr. Ronald G. Victor made numerous invaluable contributions to the design of the study, interpretation of the results, and development and critical review of the manuscript prior to his death on September 10, 2018.
Funding
This project was funded by the NIH (RC4-AG039077 from the National Institute on Aging and UL1-TR001881 from the National Center for Advancing Translational Sciences). The sponsors had no role in the design and conduct of the study, nor in the collection, management, analysis, or interpretation of the data, nor in the preparation, review, or approval of the manuscript, nor in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Ronald G. Victor is deceased.
Electronic Supplementary Material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Shapiro, M.F., Shu, S.B., Goldstein, N.J. et al. Impact of a Patient-Centered Behavioral Economics Intervention on Hypertension Control in a Highly Disadvantaged Population: a Randomized Trial. J GEN INTERN MED 35, 70–78 (2020). https://doi.org/10.1007/s11606-019-05269-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05269-z