Abstract
Background
Declining mortality has led to a rising number of persons living with HIV (PLWH) and concerns about a future shortage of HIV practitioners.
Aim
To develop an HIV Primary Care Track for internal medicine residents.
Setting
Academic hospital and community health center with a history of caring for PLWH and lesbian, gay, bisexual, and transgender (LGBT) patients.
Participants
Internal medicine residents.
Program Description
We enrolled four residents annually in a 3-year track with the goal of having each provide continuity care to at least 20 PLWH. The curriculum included small group learning sessions, outpatient electives, a global health opportunity, and the development of a scholarly project.
Program Evaluation
All residents successfully accrued 20 or more PLWH as continuity patients. Senior residents passed the American Academy of HIV Medicine certification exam, and 75 % of graduates took positions in primary care involving PLWH. Clinical performance of residents in HIV care quality measures was comparable to those reported in published cohorts.
Discussion
We developed and implemented a novel track to train medical residents in the care of PLWH and LGBT patients. Our results suggest that a designated residency track can serve as a model for training the next generation of HIV practitioners.
Similar content being viewed by others
INTRODUCTION
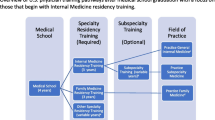
Mortality in persons living with HIV (PLWH) has fallen sharply with the availability of potent antiretroviral therapy (ART)1, although incident infections remain at 50,000 cases annually.2 As a result, HIV prevalence continues to rise steadily, with an estimated 1.2 million PLWH in the United States3. However, declining infectious disease fellowship applications4 and retiring first-generation HIV clinicians have led to concerns that the increase in the number of HIV-infected patients will result in a future shortage of practitioners, prompting a public call for solutions.5 , 6
As HIV infection has evolved into a chronic disease with well-tolerated therapies and an increased focus on long-term morbidities, primary care practitioners are well positioned to assume management of this patient population. However, care of PLWH involves unique challenges, leading to the question of whether generalists have the necessary training to manage ART, medication adherence, drug interactions, and opportunistic infections, while negotiating biopsychosocial issues for populations at high risk for HIV, including members of the lesbian, gay, bisexual, and transgender (LGBT) communities and people who use injection drugs. However, the training necessary to prepare internal medicine residency graduates in the care of these populations is generally lacking.7 – 9
PLWH have better outcomes when cared for by practitioners with more experience managing their complex needs. For example, generalists who managed fewer than 20 PLWH performed significantly worse on HIV-related quality measures, including engagement in care, viral load testing, and virologic suppression.10 Accordingly, a 20-patient cutoff is used as the eligibility threshold for taking the American Academy of HIV Medicine (AAHIVM) certification exam. Surveys have also shown that most internal medicine residents lack the opportunity to provide sufficient continuity care to PLWH8 and feel inadequately prepared to manage care for this population.9 Moreover, despite the disproportionate risk for HIV in men who have sex with men (MSM) and other members of LGBT communities, little time is dedicated to the unique health needs of these populations in medical curricula,11 , 12 leading the American Association of Medical Colleges to call for development of competency-based training across the continuum of medical education to fill this gap.13 To address these unmet training and workforce needs, we implemented a novel 3-year HIV Primary Care Track (HIV PCT) to train internal medicine residents in HIV medicine and LGBT health, with the unique goal of producing competent primary care practitioners for PLWH.
SETTING AND PARTICIPANTS
We developed an HIV PCT for residency training as a separate match under the National Resident Matching Program at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA. The resident continuity clinic was situated at Fenway Health, an affiliated community health center with a long tradition of caring for PLWH and members of the LGBT community. Development of the track was funded through a 5-year Health Resources and Services Administration (HRSA) grant.
Between 2011 and 2015, four medicine interns joined the HIV PCT each year, achieving a full cohort of 12 residents during the 2013–2014 academic year. In years with unfilled slots, we recruited interested interns via a post-match survey.
PROGRAM DESCRIPTION
Goal
The goal was to establish a pathway to train future practitioners to provide competent care for PLWH and persons identifying as LGBT.
Objectives
Our program objectives were:
-
1)
To establish a new match for residents in an HIV PCT
-
2)
To identify a core faculty of preceptors with expertise in HIV medicine and LGBT health
-
3)
To recruit at least 20 HIV-infected patients per resident as continuity patients
-
4)
To develop a comprehensive curriculum addressing HIV and LGBT health for track residents
-
5)
To prepare track residents for certification as HIV specialists
-
6)
To develop objective structured clinical examinations (OSCEs) to formatively assess specialized skills
Curriculum
HIV PCT residents held their weekly continuity clinic at Fenway Health, with core faculty serving as preceptors. Residents were expected to establish a patient panel that included at least 20 PLWH. They were also given several references, including a locally produced HIV manual,14 the Fenway Guide to LGBT Health,15 the AAHIVM Fundamentals of HIV Medicine,16 and a subscription to AIDS Clinical Care. In addition to the standard HIV ambulatory care intern curriculum, HIV PCT residents participated in a weekly conference consisting of didactic, case-based discussions on HIV/LGBT care and related issues, including management of a new HIV diagnosis, starting ART, pre- and post-exposure prophylaxis, HIV resistance testing and managing virologic failure, sexually transmitted infections (STI), contraception and family planning, aging and HIV, addiction medicine, and primary care of LGBT patients. HIV PCT residents were also invited to a weekly interdisciplinary conference attended by primary care HIV practitioners, infectious disease specialists, and an HIV case manager, and completed online case modules developed by the International Antiviral Society—USA.17 In addition, outpatient electives in infectious diseases and HIV-related fields such as substance abuse and public health were encouraged, as was participation in a global health rotation in a high-HIV-prevalence region (e.g., Botswana). Finally, residents were required to complete a project culminating in a presentation at an academic meeting. Upon completing residency, participants were expected to take the AAHIVM certification exam. A curricular map is provided in Table 1.
Program Evaluation
We designed a comprehensive program evaluation in three domains—learner-centered, patient-centered, and institution-centered—along Kirkpatrick’s levels of evaluation (Table 2). The institutional review board at Fenway Health approved the project as quality improvement. Program evaluation metrics were largely descriptive rather than comparative: Track residents represented motivated trainees, which would have introduced self-selection bias if compared to a control group of residents. Additionally, HIV PCT residents’ clinic and assessment experiences had no equivalents in the categorical track.
To assess learner attitudes toward the curriculum, we conducted yearly surveys of resident perceptions and focus groups to assess resident satisfaction. The survey instrument was developed by program faculty in an iterative and collaborative manner and was piloted prior to use. Tabulation of survey results indicated that the majority of interns entering the program had career interests aligned with the goals of the HIV PCT, including a reported desire to practice primary care (88 %), infectious disease (63 %), HIV care (88 %), and care of an underserved population (88 %).
We conducted focus groups at the end of each academic year with open-ended questions focused on the educational and professional impact of the program. A thematic analysis of audio recordings from the focus groups identified several key motifs. Residents remarked on the uniqueness of the Fenway patients, which provided a vastly different perspective on HIV compared to previous experiences with PLWH. The opportunity to care for transgender patients in particular provided an unparalleled clinical experience, as summed up by one resident: “The specialized training I’ve got is in LGBT primary care, and the track should probably be renamed HIV and LGBT primary care.” Additionally, the HIV PCT had an unexpectedly path-shifting impact on residents’ careers. One resident articulated, “[It] altered [my career]. I wouldn’t have ever expected to work with this population when I was in med school. I would have said that I would have ended up still at a community health center but probably with a Hispanic population or inner city population. I never would have expected to start working with LGBT [individuals].”
We also assessed resident learning using the AAHIVM certification exam; seven of our first eight graduates took the exam, all of whom passed. To provide formative feedback to residents on their knowledge and skills, we held OSCEs at the end of each academic year. OSCE stations were thematically linked and increased in complexity across all years of training; topics included preconception/contraception, STIs, HIV management, and LGBT health. Resident OSCE scores from faculty and standardized patients were high; however, the cases allowed us to identify specific areas for resident improvement and curricular refinement. For instance, relatively poor performance by male residents on cases addressing women’s health needs led us to provide additional experiences for male HIV PCT residents in a women’s health clinic.
The program also successfully achieved a resident continuity patient panel size of 20 or more PLWH: on average, the panels of the eight HIV PCT graduates included 21.9 PLWH. Only one resident, who joined the track in her second year, graduated with a panel of 17 PLWH.
We examined the impact of our curriculum in various ways. First, we examined 2-year performance on several core HRSA HIV/AIDS Bureau measures18 (Table 3). HRSA has not published benchmarks for these measures and provides only comparison data that differ by cohort, methodology, and date range, depending on the specific quality measure. Overall, however, HIV PCT resident performance on assessed quality measures was broadly comparable to these published comparison group data.18 We also assessed patient satisfaction from PLWH who identified track residents as their primary practitioner, using an instrument extensively employed in our other clinics and modified for the Fenway population. Data tabulated from 120 surveys collected over 2 years showed that patients had high levels of satisfaction with the care their HIV PCT residents provided (see Online Appendix for more detailed results). To address our objective of developing a core faculty, we expanded the number of preceptors from 7 to 12, and broadened the resident training experience to a second Fenway Health site with new preceptors. Finally, we examined workforce development and found that six of our first eight HIV PCT graduates took positions in primary care involving care of PLWH.
DISCUSSION
We developed and implemented a residency track to train residents in providing competent care for PLWH and persons identifying as LGBT. Our novel accomplishments were a dedicated residency track in HIV, continuity care for at least 20 PLWH, a training site uniquely serving PLWH and LGBT patients, and a curriculum attentive to healthcare determinants in these underserved communities, including stigmatization, mental health, and substance abuse. Additionally, our focus on a primary care perspective differentiated our program from standard ID fellowship programs which, in addition to requiring 2–3 years post-residency, are designed to train consultative subspecialists and generally do not address primary care skills that are necessary to practice outpatient HIV medicine. Our early success in training AAHIVM-certified graduates who choose careers in HIV medicine and primary care supports ongoing use of this model to train the next generation of HIV practitioners. We have previously published manuscripts on our OSCEs,19 , 20 and presented a description of our track at the 2015 national meeting of the Infectious Diseases Society of America.21 A small number of other residency programs have established HIV medicine pathways,22 , 23 one of which has shown that the majority of their recent graduates (5 of 7) have also pursued careers caring for PLWH,22 giving further credence to the success of this model.
Lessons Learned
While implementing our residency curriculum, we encountered several challenges instructive for those attempting to design similar programs. First, although more than 2000 PLWH receive care at Fenway Health, resident HIV panel accrual has been more difficult than anticipated, due to patient reluctance to disrupt pre-existing relationships with faculty practitioners. It was particularly challenging for female residents to build panels, as Fenway MSM patients express a preference for male practitioners. Second, we learned that recruiting medical students into a specialized track can be problematic at a time when career goals are often not yet established and there is a fear of being “pigeonholed.” We found that proactively discussing the track with new interns immediately after arrival helped allay fears about limiting career options. Finally, financial sustainability has been a concern. While the majority of the resources necessary to sustain the track after the grant ends have been accommodated with existing resources, some aspects of the curriculum, such as annual OSCEs ($4400 last year), may require supplemental funding.
In summary, we developed an innovative 3-year program to train residents in primary care for PLWH and persons identifying as LGBT. Our favorable clinical outcomes and success in producing AAHIVM-certified graduates who have selected primary care practice and related fields involving the care of PLWH suggest that a focused residency track can be an effective strategy for training the next generation of HIV practitioners. In the future, we will further investigate the clinical outcomes of PLWH who have HIV PCT resident practitioners and track career trajectories of graduates to confirm their ongoing focus on caring for PLWH.
References
Samji H, Cescon A, Hogg RS, et al. North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEASO. PLoS One. 2013;8, e81355.
Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6, e17502.
Centers for Disease Control and Prevention. Prevalence of Diagnosed and Undiagnosed HIV Infection—United States, 2008–2012. MMWR. 2015;64:657–62.
National Resident Matching Program, Results and Data: Specialties Matching Service 2015 Appointment Year. National Resident Matching Program, Washington, DC. 2015.
Health Resources and Services Administration. Workforce Capacity in HIV. HRSA Care Action. 2010:1–12.
Committee on Screening and Access to Care, Institute of Medicine. HIV Screening and Access to Care: Health Care System Capacity for Increased HIV Testing and Provision of Care. National Academies Press, 2011.
Philips K, Cofrancesco J, Sisson S, Wu A, Bass E, Berkenblit B. A multicenter study of internal medicine residents’ perceptions of training, competence, and performance in outpatient HIV care. AIDS Patient Care STDs. 2010;24:159–64.
Adams J, Chacko K, Guiton G, Aagaard E. Training internal medicine residents in outpatient HIV care: a survey of program directors. J Gen Intern Med. 2010;25:977–81.
Prasad R, D’Amico F, Wilson S, et al. Training family medicine residents in HIV primary care: a national survey of program directors. Fam Med. 2014;46:527–31.
O’Neill M, Karelas G, Feller D, et al. The HIV workforce in New York state: does patient volume correlate with quality? Clin Infect Dis. 2015;61:1871–79.
Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306:971–77.
Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med. 2014;21:608–11.
Hollenbach A, Eckstrand KL, Dreger A, eds. Implementing Curricular and Institutional Climate Changes to Improve Health Care for Individuals Who Are LGBT, Gender Nonconforming, or Born with DSD. AAMC; Washington, D.C. 2014.
Makadon H, Mayer K, Potter, J, Goldhammer H, eds. The Fenway Guide to Lesbian, Gay, Bisexual and Transgender Health, 2nd ed. American College of Physicians, 2015.
Libman H. HIV manual. Boston: Healthcare Associates, Beth Israel Deaconess Medical Center; 2014.
American Academy of HIV Medicine. Fundamentals of HIV Management. American Academy of HIV Medicine, 2012.
International Antiviral Society - USA. Cases on the Web. 2016. Available at: https://www.iasusa.org/cow. Accessed 4/24/16.
Health Resources Services Administration HIV/AIDS Bureau. HIV HAB Performance Measures. 2013. Available at: http://hab.hrsa.gov/deliverhivaidscare/habperformmeasures.html. Accessed 4/24/16.
Fessler D, Huang G. Relaying an HIV diagnosis: a standardized patient case. MedEdPORTAL; 2014. Available at: www.mededportal.org/publication/9717.
Potter J, Fessler D, Huang G, Baker J, Dearborn H, Libman H. OSCE station: challenging pelvic exam. MedEdPORTAL; 2015. Available at: www.mededportal.org/publication/10256.
Fessler D, Huang G, Potter J, Baker J, Libman H. Development and Implementation of a Novel HIV Primary Care Track for Internal Medicine Residents [Abstract 442]. Poster presented at IDWeek; San Diego; 2015 Oct 7–11.
Budak J, Volkman K, Wood B, Dhanireddy S. Building HIV Workforce Capacity through an Innovative HIV Medicine Pathway within an Internal Medicine Residency [Abstract 426]. Poster presented at IDWeek; San Diego; 2015 Oct 7–11.
Barakat L, Yamahiro A, Sadigh KS, et al. The changing face of HIV care: Expanding HIV training in internal medicine residency. Oral presentation presented at SGIM New England Regional Meeting; New Haven, CT; 2016 Mar 11.
Acknowledgments
The authors would like to acknowledge the important contributions of Drs. Alex Gonzalez, Steven Boswell, C. Christopher Smith, and Eileen Reynolds in the support of our residency program, and Christina Thuerwachter and Hillary Dearborn for their administrative contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funders
Health Resources and Services Administration, grant number D5FHP20672.
Conflicts of Interest
Grace C. Huang owns stock and stock options in Pfizer Inc.
Howard Libman has served as a consultant for Gilead Sciences Inc. and has provided expert testimony in legal cases.
All other authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Fessler, D.A., Huang, G.C., Potter, J. et al. Development and Implementation of a Novel HIV Primary Care Track for Internal Medicine Residents. J GEN INTERN MED 32, 350–354 (2017). https://doi.org/10.1007/s11606-016-3878-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-016-3878-9