ABSTRACT
OBJECTIVES
We employed a partnered research healthcare delivery redesign process to improve care for high-need, high-cost (HNHC) patients within the Veterans Affairs (VA) healthcare system.
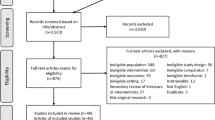
METHODS
Health services researchers partnered with VA national and Palo Alto facility leadership and clinicians to: 1) analyze characteristics and utilization patterns of HNHC patients, 2) synthesize evidence about intensive management programs for HNHC patients, 3) conduct needs-assessment interviews with HNHC patients (n = 17) across medical, access, social, and mental health domains, 4) survey providers (n = 8) about care challenges for HNHC patients, and 5) design, implement, and evaluate a pilot Intensive Management Patient-Aligned Care Team (ImPACT) for a random sample of 150 patients.
RESULTS
HNHC patients accounted for over half (52 %) of VA facility patient costs. Most (94 %) had three or more chronic conditions, and 60 % had a mental health diagnosis. Formative data analyses and qualitative assessments revealed a need for intensive case management, care coordination, transitions navigation, and social support and services. The ImPACT multidisciplinary team developed care processes to meet these needs, including direct access to team members (including after-hours), chronic disease management protocols, case management, and rapid interventions in response to health changes or acute service use. Two-thirds of invited patients (n = 101) enrolled in ImPACT, 87 % of whom remained actively engaged at 9 months. ImPACT is now serving as a model for a national VA intensive management demonstration project.
CONCLUSIONS
Partnered research that incorporated population data analysis, evidence synthesis, and stakeholder needs assessments led to the successful redesign and implementation of services for HNHC patients. The rigorous design process and evaluation facilitated dissemination of the intervention within the VA healthcare system.
IMPACT STATEMENT
Employing partnered research to redesign care for high-need, high-cost patients may expedite development and dissemination of high-value, cost-saving interventions.
Similar content being viewed by others
REFERENCES
Cohen S, Yu W. AHRQ Statistical Brief #354: The concentration and persistance in the level of health expenditures over time: Estimates for the US population, 2008-2009. 2012. http://meps.ahrq.gov/mepsweb/data_files/publications/st354/stat354.pdf. 8/29/14.
Mann C. Medicaid and CHIP: On the Road to Reform. Alliance for Health Reform/Kaiser Family Foundation. 2011. www.allhealth.org/briefingmaterials/KFFAlliance_FINAL-1971.ppt. 8/29/14.
Joynt K, Gawande AA, Orav E, Jha A. Contribution of preventable acute care spending to total spending for high-cost medicare patients. JAMA. 2013;309(24):2572–2578.
Conwell LJ, Cohen JW. AHRQ Statistical Brief #73: Characteristics of persons with high medical expenditures in the U.S. civilian noninstitutionalized population, 2002. 2005. http://meps.ahrq.gov/data_files/publications/st73/stat73.pdf. 8/29/14.
Sommers A, Cohen M. Medicaid's High Cost Enrollees: How Much Do They Drive Program Spending? Kaiser Commission for Medicaid and the Uninsured. D.C.: Washington; 2006.
Coughlin TA, Long SK. Health care spending and service use among high-cost Medicaid beneficiaries, 2002–2004. Inquiry Journal. 2009;46(4):405–17.
Zulman DM, Yoon J, Cohen DM, Wagner TH, Ritchie C, Asch SM. Multimorbidity and health care utilization among high-cost patients: Implications for care coordination. J Gen Intern Med. 2013;28(1):S123.
Silow-Carroll S, Edwards JN. Early Adopters of the Accountable Care Model: A Field Report on Improvements in Health Care Delivery. The Commonwealth Fund; New York, NY; 2013.
Hasselman D. Super-Utilizer Summit: Common Themes from Innovative Complex Care Management Programs. Center for Health Care Strategies, Inc. Hamilton, N.J. 2013.
Yee T, Lechner A, Carrier E. High-Intensity Primary Care: Lessons for Physician and Patient Engagment. National Institute for Health Care Reform. 2012;9.
Peterson D, Helfand M, Humphrey L, Christensen V, Carson S. Evidence Brief: Effectiveness of Intensive Primary Care Programs, VA-ESP Project #09-199; 2012.
Bodenheimer T. Strategies to Reduce Costs and Improve Care for High-Utilizing Medicaid Patients: Reflections on Pioneering Programs. Center for Health Care Strategies, Inc. 2013.
Reuben DB. Physicians in supporting roles in chronic disease care: The CareMore model. J Am Geriatr Soc. 2011;59(1):158–60.
Blash L, Chapman S, Dower C. The Special Care Center - A joint venture to address chronic disease. 2011. http://www.futurehealth.ucsf.edu/content/29/2010-11_the_special_care_center_a_joint_venture_to_address_chronic_disease.pdf. 8/29/14.
Milstein A, Kothari P. Are higher-value care models replicable? Health Affairs Blog. 2009. http://healthaffairs.org/blog/2009/10/20/are-higher-value-care-models-replicable/. 8/29/14.
Shumway M, Boccellari A, O'Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: Results of a randomized trial. Am J Emerg Med. 2008;26(2):155–64.
Sledge WH, Brown KE, Levine JM, Fiellin DA, Chawarski M, White WD, O'Connor PG. A randomized trial of primary intensive care to reduce hospital admissions in patients with high utilization of inpatient services. Disease Management. 2006;9(6):328–38.
Bell J, Mancuso D, Krupski T, Joesch JM, Atkins DC, Court B, West II, Roy-Byrne P. A randomized controlled trial of King County Care Partners’ Rethinking Care Intervention: Health and social outcomes up to two years post-randomization. 2012. http://www.chcs.org/media/RTC_Evaluation_TECHNICAL_REPORT_FINAL_3_15_12a.pdf. 8/29/14.
Brenner J. Reforming Camden's health care system—one patient at a time. Prescriptions for Excellence in Health Care. 2009;5:1–3.
Gawande A. The hot spotters: Can we lower medical costs by giving the neediest patients better care? The New Yorker; 2011.
Green SR, Singh V, O'Byrne W. Hope for New Jersey's city hospitals: The Camden Initiative. Perspect Health Inf Manag. 2010;7:1d.
Raven MC, Doran KM, Kostrowski S, Gillespie CC, Elbel BD. An intervention to improve care and reduce costs for high-risk patients with frequent hospital admissions: A pilot study. BMC Health Serv Res. 2011;11:270.
Dorr DA, Wilcox A, Burns L, Brunker CP, Narus SP, Clayton PD. Implementing a multidisease chronic care model in primary care using people and technology. Dis Manag. 2006;9(1):1–15.
Demakis JG, McQueen L, Kizer KW, Feussner JR. Quality Enhancement Research Initiative (QUERI): A collaboration between research and clinical practice. Med Care. 2000;38(6 Suppl 1):I17–25.
Oliver A. Public-sector health-care reforms that work? A case study of the U.S. Veterans Health Administration. Lancet. 2008;371(9619):1211–3.
O'Sullivan RG. Collaborative evaluation within a framework of stakeholder-oriented evaluation approaches. Eval Program Plann. 2012;35(4):518–22.
Yoon J, Scott J, Phibbs CS, Wagner TH. Recent trends in Veterans Affairs chronic condition spending. Popul Health Manag. 2011;14(6):293–8.
Yu W, Ravelo A, Wagner TH, Phibbs CS, Bhandari A, Chen S, Barnett PG. Prevalence and costs of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(3 Suppl):146S–167S.
Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs Associated With Multimorbidity Among VA Patients. Med Care. 2014;52(Suppl 3):S31–6.
Dorr D, Wilcox AB, Brunker CP, Burdon RE, Donnelly SM. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. J Am Geriatr Soc. 2008;56(12):2195–202.
Brown KE, Levine JM, Fiellin DA, O'Connor P, Sledge WH. Primary intensive care: Pilot study of a primary care-based intervention for high-utilizing patients. Dis Manag. 2005;8(3):169–77.
Lessler DS, Krupski A, Cristofalo M. King County Care Partners: A Community-Based Chronic Care Management System for Medicaid Clients with Co-Occurring Medical, Mental, and Substance Abuse Disorders. Comprehensive Care Coordination for Chronically III Adults: John Wiley & Sons, Inc.; 2011:339-348.
Okin RL, Boccellari A, Azocar F, Shumway M, O'Brien K, Gelb A, Kohn M, Harding P, Wachsmuth C. The effects of clinical case management on hospital service use among ED frequent users. Am J Emerg Med. 2000;18(5):603–8.
Brown RS, Peikes D, Peterson G, Schore J, Razafindrakoto CM. Six features of Medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Aff (Millwood). 2012;31(6):1156–66.
Boult C, Murphy EK. New models of comprehensive health care for people with chronic conditions. In: IOM, ed. Living Well with Chronic Illness: A Call for Public Action. Washington, D.C.: The National Academies Press; 2012:285-318.
Smith S, Soubhi H, Fortin M, Hudon C, O'Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2012(1469-493X).
Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy SM, Shojania K, Reston JT, Adams AS, Angood PB, Bates DW, Bickman L, Carayon P, Donaldson L, Duan N, Farley DO, Greenhalgh T, Haughom JL, Lake E, Lilford R, Lohr KN, Meyer GS, Miller MR, Neuhauser DV, Ryan G, Saint S, Shortell SM, Stevens DP, Walshe K. The Top Patient Safety Strategies That Can Be Encouraged for Adoption Now. Annals of Internal Medicine. 2013;158(5_Part_2):365-368.
California Healthcare Foundation, California Quality Collaborative. Complex Care Management Toolkit. 2012. http://www.calquality.org/storage/documents/cqc_complexcaremanagement_toolkit_final.pdf. 8/29/14.
Humboldt IPA Priority Care. Domain Assessment Tool. 2011. http://www.calquality.org/programs/clinicalcare/meteor/documents/1.2.2Humboldt_DomainsScoringLevels.pdf. 8/29/14.
Rosland AM, Nelson K, Sun H, Dolan ED, Maynard C, Bryson C, Stark R, Shear JM, Kerr E, Fihn SD, Schectman G. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263–72.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
Fitzpatrick JL. Commentary–collaborative evaluation within the larger evaluation context. Eval Program Plann. 2012;35(4):558–63.
Wang L, Porter B, Maynard C, Evans G, Bryson C, Sun H, Gupta I, Lowy E, McDonell M, Frisbee K, Nielson C, Kirkland F, Fihn SD. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368–73.
Rodriguez-Campos L. Advances in collaborative evaluation. Eval Program Plann. 2012;35(4):523–8.
Perneger T. Ten reasons to conduct a randomized study in quality improvement. Int J Qual Health Care. 2006;18(6):395–6.
Bamberger JM, Rugh J, Mabry LS. RealWorld Evaluation: Working Under Budget, Time, Data, and Political Constraints, 2nd edition. SAGE Publications; 2011
Acknowledgements
Contributors
Authors would like to acknowledge Drs. Ian Tong and James Hallenbeck, Ms. Kalkidan Asrat, Ms. Lien Nguyen, and Ms. Jessica Radmilovic for their contributions to ImPACT’s design and implementation; Drs. Alan Glaseroff and Ann Lindsay from Stanford Coordinated Care for serving as clinical advisors to the ImPACT program; Danielle Cohen, Valerie Meausoone, and Cindie Slightam for data management and program evaluation support; and Ava Wong and Cindie Slightam for assistance with manuscript preparation. VA Palo Alto data acquisition and analysis was supported by Robert Chang, Robert King, Chi Pham, Lakshmi Ananth, and the Veterans Affairs Women’s Health Evaluation Initiative. Views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs.
Funders
ImPACT program development and implementation was supported by the VA Office of Specialty Care Transformation (Specialty/Surgical Care Neighborhood Team Based Model Pilot Program). ImPACT program evaluation was supported by VA HSR&D (PPO 13-117). Dr. Zulman is supported by a VA HSR&D Career Development Award (CDA 12-173). Dr. Shaw is supported in part by VA Office of Academic Affairs and HSR&D funds. Dr. Breland is supported by the VA Office of Affiliations and VA HSR&D Service in conjunction with a VA HSR&D Advanced Fellowship Program.
Prior Presentations
None.
Conflicts of Interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zulman, D.M., Ezeji-Okoye, S.C., Shaw, J.G. et al. Partnered Research in Healthcare Delivery Redesign for High-Need, High-Cost Patients: Development and Feasibility of an Intensive Management Patient-Aligned Care Team (ImPACT). J GEN INTERN MED 29 (Suppl 4), 861–869 (2014). https://doi.org/10.1007/s11606-014-3022-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3022-7