ABSTRACT
Background
Safety-net hospital systems provide care to a large proportion of United States’ under- and uninsured population. We have witnessed delayed colorectal cancer (CRC) care in this population and sought to identify demographic and systemic differences in these patients compared to those in an insured health-care system.
Design, Patients, and Approach/Measurements
We collected demographic, socioeconomic, and clinical data from 2005–2007 on all patients with CRC seen at Parkland Health and Hospital System (PHHS), a safety-net health system and at Presbyterian Hospital Dallas System (Presbyterian), a community health system, and compared characteristics among the two health-care systems. Variables associated with advanced stage were identified with multivariate logistic regression analysis and odds ratios were calculated.
Results
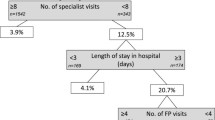
Three hundred and eighteen patients at PHHS and 397 patients at Presbyterian with CRC were identified. An overwhelming majority (75 %) of patients seen at the safety-net were diagnosed after being seen in the emergency department or at an outside facility. These patients had a higher percentage of stage 4 disease compared to the community. Patients within the safety-net with Medicare/private insurance had lower rates of advanced disease than uninsured patients (25 % vs. 68 %, p < 0.001). Insurance status and physician encounter resulting in diagnosis were independent predictors of disease stage at diagnosis.
Conclusions
A large proportion of patients seen in the safety-net health system were transferred from outside systems after diagnosis, thus leading to delayed care. This delay in care drove advanced stage at diagnosis. The data point to a pervasive and systematic issue in patients with CRC and have fundamental health policy implications for population-based CRC screening.


Similar content being viewed by others
REFERENCES
Levin B, Lieberman DA, McFarland B, et al. Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin 2008: CA.2007.0018.
Ransohoff DF, Sandler RS. Clinical practice. Screening for colorectal cancer. N Engl J Med 2002; 346(1): 40–4.
Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008; 149(9): 627–37.
CDC: Behavioral Risk Factor Surveillance System Survey Data. In: (CDC) CfDCaP, ed. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2007.
Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult U.S. population. Cancer 2004; 100(10): 2093–103.
Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev 2006; 15(2): 389–394.
Wardle J, McCaffery K, Nadel M, Atkin W. Socioeconomic differences in cancer screening participation: comparing cognitive and psychosocial explanations. Soc Sci Med 2004; 59(2): 249–61.
Cairns CP, Viswanath K. Communication and colorectal cancer screening among the uninsured: data from the Health Information National Trends Survey (United States). Cancer Causes Control 2006; 17(9): 1115–25.
Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med 2005; 20(11): 989–95.
Farmer MM, Bastani R, Kwan L, Belman M, Ganz PA. Predictors of colorectal cancer screening from patients enrolled in a managed care health plan. Cancer 2008; 112(6):1230–8.
Fernandez ME, Wippold R, Torres-Vigil I, et al. Colorectal cancer screening among Latinos from U.S. cities along the Texas–Mexico border. Cancer Causes Control 2008; 19(2): 195–206.
Geiger TM, Miedema BW, Geana MV, Thaler K, Rangnekar NJ, Cameron GT. Improving rates for screening colonoscopy: Analysis of the health information national trends survey (HINTS I) data. Surg Endosc 22(2):527–33.
Ko CW, Kreuter W, Baldwin LM. Persistent demographic differences in colorectal cancer screening utilization despite Medicare reimbursement. BMC Gastroenterol 2005; 5: 10.
Lewin M, Altman S, eds. America's Health Care Safety Net: Intact but Endangered: Washington, DC: Institute of Medicine, National Acadamies Press, 2000.
Goodman MJ, Ogdie A, Kanamori MJ, Canar J, O'Malley AS. Barriers and facilitators of colorectal cancer screening among Mid-Atlantic Latinos: focus group findings. Ethn Dis 2006; 16(1): 255–61.
Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med 2007; 5(6): 511–8.
Fiscella K, Holt K. Impact of primary care patient visits on racial and ethnic disparities in preventive care in the United States. J Am Board Fam Med 2007; 20(6): 587–97.
Powell-Griner E, Bolen J, Bland S. Health care coverage and use of preventive services among the near elderly in the United States. Am J Public Health 1999; 89(6): 882–6.
Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Prev Med 2003; 37(5): 475–84.
Sudano JJ, Jr., Baker DW. Intermittent lack of health insurance coverage and use of preventive services. Am J Public Health 2003; 93(1): 130–7.
The Uninsured in Texas. 5/5/2008 ed: Texas Medical Association, 2008.
Examination and treatment for emergency medical conditions and women in active labor. 131: S13902-S13904. Congressional Record: Congressional Record, 1985.
Ansell DA, Schiff RL. Patient dumping. Status, implications, and policy recommendations. JAMA 1987; 257(11): 1500–2.
Schiff RL, Ansell D. Federal anti-patient-dumping provisions: the first decade. Ann Emerg Med 1996; 28(1): 77–9.
Schiff RL, Ansell DA, Schlosser JE, Idris AH, Morrison A, Whitman S. Transfers to a public hospital. A prospective study of 467 patients. N Engl J Med 1986; 314(9): 552–7.
Sloane D. Cancer epidemiology in the United States: racial, social, and economic factors. Methods Mol Biol 2009; 471: 65–83.
Halpern MT, Pavluck AL, Ko CY, Ward EM. Factors Associated with Colon Cancer Stage at Diagnosis. Dig Dis Sci 2009; 54: 2680–93.
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol 2008; 9(3): 222–31.
Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin 2004; 54(2): 78–93.
Rapid Response Surveillance Studies. National Cancer Institute.
American Community Survey: Accuracy of the Data. In: Bureau USC, ed.
Carrasquillo O, Pati S. The role of health insurance on Pap smear and mammography utilization by immigrants living in the United States. Prev Med 2004; 39(5): 943–50.
Korda RJ, Butler JRG, Clements MS, Kunitz SJ. Differential impacts of health care in Australia: trend analysis of socioeconomic inequalities in avoidable mortality. Int J Epidemiol 2007; 36(1):157–65.
Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the veterans health administration and patients in a national sample. Ann Intern Med 2004; 141(12): 938–45.
Parkland Hospital. Parkland Hospital at a Glance: Who We Are. http://www.parklandhospital.com/whoweare/at_a_glance/. Accessed April 4, 2012.
Pestonjee S et al. The Reading Level Determination Study: Parkland Health & Hospital System. Parkland Health & Hospital System, 1998. http://www.parklandhospital.com/patients_visitors/health_information/pdf/Rdg%20Stdy%20Abstr.pdf. Accessed April 12, 2012.
DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2007. U.S. Census Bureau, Current Population Reports. Washington, DC: U.S. Government Printing Office, 2008; 60–235.
Bundorf MK, Pauly MV. Is health insurance affordable for the uninsured? J Health Econ 2006; 25(4): 650–73.
United States Department of Health and Human Services: Healthy people 2010: understanding and improving health, 2nd ed. Washington, DC: US Government Printing Office, 2000.
Acknowledgments
The authors would like to thank the staff at the Parkland Health and Hospital System and Presbyterian Health System tumor registries for their assistance. We thank Drs. Chul Ahn and Lei Xuan for statistical assistance. We wish to specifically thank Dr. Ron Anderson for insightful comments and suggestions.
This work was supported the NIH (CTSA grant UL1 RR024982-02 and by NIH training grant T32DK07745 (to JS).
Conflict of Interest
Disclosure information: The authors certify that we have no financial arrangements (e.g., consultancies, stock ownership, equity interests, patent-licensing arrangements, research support, major honoraria, etc.) with a company whose product figures prominently in this manuscript or with a company making a competing product. To the best of our knowledge, no conflict of interest, financial or other, exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, J.P., Valdes, M. & Rockey, D.C. Transferred and Delayed Care of Patients with Colorectal Cancer in a Safety-Net Hospital System—Manifestations of a Distressed Healthcare System. J GEN INTERN MED 27, 1142–1149 (2012). https://doi.org/10.1007/s11606-012-2040-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2040-6