Abstract
Background
Pancreatic adenocarcinoma (PDAC) is an aggressive malignancy associated with poor outcomes. Surgical resection and receipt of multimodal therapy have been shown to improve outcomes in patients with potentially resectable PDAC; however treatment and outcome disparities persist on many fronts. The aim of this study was to analyze the relationship between rural residence and receipt of quality cancer care in patients diagnosed with non-metastatic PDAC.
Methods
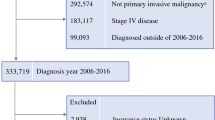
Using the National Cancer Database, patients with non-metastatic pancreatic cancer were identified from 2006–2016. Patients were classified as living in metropolitan, urban, or rural areas. Multivariable logistic regression was used to identify predictors of cancer treatment and survival.
Results
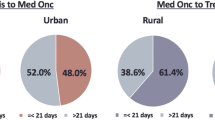
A total of 41,786 patients were identified: 81.6% metropolitan, 16.2% urban, and 2.2% rural. Rural residing patients were less likely to receive curative-intent surgery (p = 0.037) and multimodal therapy (p < 0.001) compared to their metropolitan and urban counterparts. On logistic regression analysis, rural residence was independently associated with decreased surgical resection [OR 0.82; CI 95% 0.69–0.99; p = 0.039] and multimodal therapy [OR 0.70; CI 95% 0.38–0.97; p = 0.047]. Rural residence independently predicted decreased overall survival [OR 1.64; CI 95% 1.45–1.93; p < 0.001] for all patients that were analyzed. In the cohort of patients who underwent surgical resection, rural residence did not independently predict overall survival [OR 0.97; CI 95% 0.85–1.11; p = 0.652].
Conclusions
Rural residence impacts receipt of optimal cancer care in patients with non-metastatic PDAC but does not predict overall survival in patients who receive curative-intent treatment.
Similar content being viewed by others
Data Availability
The National Cancer Database is available through the American College of Surgeons.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. https://doi.org/10.3322/caac.21708.
Strobel O, Neoptolemos J, Jäger D, Büchler MW. Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol. 2019;16(1):11-26. https://doi.org/10.1038/s41571-018-0112-1.
Ansari D, Tingstedt B, Andersson B, Holmquist F, Sturesson C, Williamsson C et al. Pancreatic cancer: yesterday, today and tomorrow. Future Oncol. 2016;12(16):1929-46. https://doi.org/10.2217/fon-2016-0010.
Ahola R, Sand J, Laukkarinen J. Centralization of Pancreatic Surgery Improves Results: Review. Scand J Surg. 2020;109(1):4-10. https://doi.org/10.1177/1457496919900411.
David JM, Kim S, Placencio-Hickok VR, Torosian A, Hendifar A, Tuli R. Treatment strategies and clinical outcomes of locally advanced pancreatic cancer patients treated at high-volume facilities and academic centers. Adv Radiat Oncol. 2019;4(2):302-13. https://doi.org/10.1016/j.adro.2018.10.006.
Gluth A, Werner J, Hartwig W. Surgical resection strategies for locally advanced pancreatic cancer. Langenbecks Arch Surg. 2015;400(7):757-65. https://doi.org/10.1007/s00423-015-1318-7.
Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011;98(4):485-94. https://doi.org/10.1002/bjs.7413.
Hartwig W, Werner J, Jäger D, Debus J, Büchler MW. Improvement of surgical results for pancreatic cancer. Lancet Oncol. 2013;14(11):e476-e85. https://doi.org/10.1016/s1470-2045(13)70172-4.
Hue JJ, Sugumar K, Markt SC, Hardacre JM, Ammori JB, Rothermel LD et al. Facility volume-survival relationship in patients with early-stage pancreatic adenocarcinoma treated with neoadjuvant chemotherapy followed by pancreatoduodenectomy. Surgery. 2021;170(1):207-14. https://doi.org/10.1016/j.surg.2020.12.003.
Chu QD, Hsieh MC, Gibbs JF, Wu XC. Social determinants of health associated with poor outcome for rural patients following resected pancreatic cancer. J Gastrointest Oncol. 2021;12(6):2567-78. https://doi.org/10.21037/jgo-20-583.
Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomarkers Prev. 2013;22(10):1657-67. https://doi.org/10.1158/1055-9965.epi-13-0404.
Bertens KA, Massman JD, 3rd, Helton S, Garbus S, Mandelson MM, Lin B et al. Initiation of adjuvant therapy following surgical resection of pancreatic ductal adenocarcinoma (PDAC): Are patients from rural, remote areas disadvantaged? J Surg Oncol. 2018;117(8):1655-63. https://doi.org/10.1002/jso.25060.
Markossian TW, Hines RB. Disparities in late stage diagnosis, treatment, and breast cancer-related death by race, age, and rural residence among women in Georgia. Women Health. 2012;52(4):317-35. https://doi.org/10.1080/03630242.2012.674091.
Walker EJ, Ko AH. Beyond first-line chemotherapy for advanced pancreatic cancer: an expanding array of therapeutic options? World J Gastroenterol. 2014;20(9):2224-36. https://doi.org/10.3748/wjg.v20.i9.2224.
Alvarez MA, Anderson K, Deneve JL, Dickson PV, Yakoub D, Fleming MD et al. Traveling for Pancreatic Cancer Care Is Worth the Trip. Am Surg. 2021;87(4):549-56. https://doi.org/10.1177/0003134820951484.
Kirkegård J, Ladekarl M, Fristrup CW, Hansen CP, Sall M, Mortensen FV. Urban versus rural residency and pancreatic cancer survival: A Danish nationwide population-based cohort study. PLoS One. 2018;13(8):e0202486. https://doi.org/10.1371/journal.pone.0202486.
Canale TD, Cho H, Cheung WY. A population-based analysis of urban-rural disparities in advanced pancreatic cancer management and outcomes. Med Oncol. 2018;35(8):116. https://doi.org/10.1007/s12032-018-1173-9.
About the National Cancer Database. ACS. https://www.facs.org/quality-programs/cancer-programs/national-cancer-database/about/#:~:text=Some%2072%20percent%20of%20all,registries%20across%20the%20United%20States. Accessed December 22, 2022.
Rural-Urban Continuum Codes [database on the Internet]. Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed: December 23, 2022
Complex Adult and Pediatric Surgery. Hospital and Surgery Center Ratings | Leapfrog Group. https://ratings.leapfroggroup.org/measure/hospital/complex-adult-and-pediatric-surgery. Accessed 23 Dec 2022
Meguid RA, Ahuja N, Chang DC. What constitutes a "high-volume" hospital for pancreatic resection? J Am Coll Surg. 2008;206(4):622.e1-9. https://doi.org/10.1016/j.jamcollsurg.2007.11.011.
Chang DC, Zhang Y, Mukherjee D, Wolfgang CL, Schulick RD, Cameron JL et al. Variations in referral patterns to high-volume centers for pancreatic cancer. J Am Coll Surg. 2009;209(6):720-6. https://doi.org/10.1016/j.jamcollsurg.2009.09.011.
Participant User Files. ACS. https://www.facs.org/quality-programs/cancer-programs/national-cancer-database/puf/.
Coffman A, Torgeson A, Lloyd S. Correlates of Refusal of Surgery in the Treatment of Non-metastatic Pancreatic Adenocarcinoma. Ann Surg Oncol. 2019;26(1):98-108. https://doi.org/10.1245/s10434-018-6708-y.
Cheung MC, Yang R, Byrne MM, Solorzano CC, Nakeeb A, Koniaris LG. Are patients of low socioeconomic status receiving suboptimal management for pancreatic adenocarcinoma? Cancer. 2010;116(3):723-33. https://doi.org/10.1002/cncr.24758.
Thobie A, Mulliri A, Bouvier V, Launoy G, Alves A, Dejardin O. Same Chance of Accessing Resection? Impact of Socioeconomic Status on Resection Rates Among Patients with Pancreatic Adenocarcinoma-A Systematic Review. Health Equity. 2021;5(1):143-50. https://doi.org/10.1089/heq.2019.0099.
Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010;145(7):634-40. https://doi.org/10.1001/archsurg.2010.118.
Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P. Challenges of Rural Cancer Care in the United States. Oncology (Williston Park). 2015;29(9):633-40.
Shapiro M, Chen Q, Huang Q, Boosalis VA, Yoon CH, Saund MS et al. Associations of Socioeconomic Variables With Resection, Stage, and Survival in Patients With Early-Stage Pancreatic Cancer. JAMA Surg. 2016;151(4):338-45. https://doi.org/10.1001/jamasurg.2015.4239.
Moaven O, Richman JS, Reddy S, Wang T, Heslin MJ, Contreras CM. Healthcare disparities in outcomes of patients with resectable pancreatic cancer. Am J Surg. 2019;217(4):725-31. https://doi.org/10.1016/j.amjsurg.2018.12.007.
Makar M, Worple E, Dove J, Hunsinger M, Arora T, Oxenberg J et al. Disparities in Care: Impact of Socioeconomic Factors on Pancreatic Surgery: Exploring the National Cancer Database. Am Surg. 2019;85(4):327-34.
Tohme S, Kaltenmeier C, Bou-Samra P, Varley PR, Tsung A. Race and Health Disparities in Patient Refusal of Surgery for Early-Stage Pancreatic Cancer: An NCDB Cohort Study. Ann Surg Oncol. 2018;25(12):3427-35. https://doi.org/10.1245/s10434-018-6680-6.
Abraham A, Al-Refaie WB, Parsons HM, Dudeja V, Vickers SM, Habermann EB. Disparities in pancreas cancer care. Ann Surg Oncol. 2013;20(6):2078-87. https://doi.org/10.1245/s10434-012-2843-z.
Khan H, Heslin MJ, Crook ED, Mehari K, Johnston FM, Fonseca AL. Fragmentation of Care in Pancreatic Cancer: Effects on Receipt of Care and Survival. J Gastrointest Surg. 2022;26(12):2522-33. https://doi.org/10.1007/s11605-022-05478-8.
Raman V, Adam MA, Turner MC, Moore HG, Mantyh CR, Migaly J. Disparity of Colon Cancer Outcomes in Rural America: Making the Case to Travel the Extra Mile. J Gastrointest Surg. 2019;23(11):2285-93. https://doi.org/10.1007/s11605-019-04270-5.
Fonseca AL, Cherla D, Kothari AN, Tzeng CD, Heslin MJ, Mehari KR et al. Association of Medicaid Expansion with Pancreatic Cancer Treatment and Outcomes: Evidence from the National Cancer Database. Ann Surg Oncol. 2022;29(1):342-51. https://doi.org/10.1245/s10434-021-10709-4.
Morris BB, Rossi B, Fuemmeler B. The role of digital health technology in rural cancer care delivery: A systematic review. J Rural Health. 2022;38(3):493-511. https://doi.org/10.1111/jrh.12619.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B et al. Using the National Cancer Database for Outcomes Research: A Review. JAMA Oncol. 2017;3(12):1722-8. https://doi.org/10.1001/jamaoncol.2016.6905.
Author information
Authors and Affiliations
Contributions
KA, AF were involved in data acquisition and analysis, KA, HK, LH, DC, KM, MH and AF were involved in conceptualization, design and methodology. KA, HK, LH, DC, VC, KM, MH, and AF were involved in manuscript preparation, edition, and revision.
Corresponding author
Ethics declarations
Conflicts of Interest
All authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amin, K., Khan, H., Hearld, L.R. et al. Association between Rural Residence and Processes of Care in Pancreatic Cancer Treatment. J Gastrointest Surg 27, 2155–2165 (2023). https://doi.org/10.1007/s11605-023-05764-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05764-z