Abstract
Introduction
Marginal ulcer (MU) is a common complication following Roux-en-Y gastric bypass (RYGB) with an incidence rate of up to 25%. Several studies have evaluated different risk factors associated with MU with inconsistent findings. In this meta-analysis, we aimed to identify the predictors of MU after RYGB.
Methods
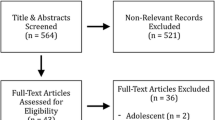
A comprehensive literature search of PubMed, Embase, and Web of Science databases was conducted through April 2022. All studies that used a multivariate model to assess risk factors for MU after RYGB were included. Pooled odds ratios (OR) with 95% confidence intervals (CI) for risk factors reported in ≥ 3 studies were obtained within a random-effects model.
Results
Fourteen studies with 344,829 patients who underwent RYGB were included. Eleven different risk factors were analyzed. Meta-analysis demonstrated that Helicobacter pylori (HP) infection (OR 4.97 [2.24–10.99]), smoking (OR 2.50 [1.76–3.54]), and diabetes mellitus (OR 1.80 [1.15–2.80]), were significant predictors of MU. Increased age, body mass index, female gender, obstructive sleep apnea, hypertension, and alcohol use were not predictors of MU. There was a trend of an increased risk of MU associated with nonsteroidal anti-inflammatory drugs (OR 2.43 [0.72–8.21]) and a lower risk of MU with proton pump inhibitors use (OR 0.44 [0.11–2.11]).
Conclusions
Smoking cessation, optimizing glycemic control, and eradication of HP infection reduce the risk of MU following RYGB. Recognition of predictors of MU after RYGB will allow physicians to identify high-risk patients, improve surgical outcomes, and reduce the risk of MU.





Similar content being viewed by others
References
Smith KB, Smith MS. Obesity Statistics. Prim Care. 2016;43(1):121–135, ix.
Giampaoli S, Vannucchi S. [Obesity and diabetes, a global problem: what does recent data tell us?]. Ig Sanita Pubbl. 2016;72(6):561-570.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964-973.
Alalwan AA, Friedman J, Park H, Segal R, Brumback BA, Hartzema AG. US national trends in bariatric surgery: A decade of study. Surgery. 2021;170(1):13-17.
Clapp B, Ponce J, DeMaria E, et al. American Society for Metabolic and Bariatric Surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surgery for Obesity and Related Diseases. 2022;18(9):1134-1140.
Maroun J, Li M, Oyefule O, et al. Ten year comparative analysis of sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch in patients with BMI ≥ 50 kg/m(2). Surg Endosc. 2022;36(7):4946-4955.
Coblijn UK, Goucham AB, Lagarde SM, Kuiken SD, van Wagensveld BA. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299-309.
Chung WC, Jeon EJ, Lee K-M, et al. Incidence and clinical features of endoscopic ulcers developing after gastrectomy. World J Gastroenterol. 2012;18(25):3260-3266.
Pantea M, Negovan A, Banescu C, et al. Factors Associated with Recurrent Ulcers in Patients with Gastric Surgery after More Than 15 Years: A Cross-Sectional Single-Center Study. Gastroenterology Research and Practice. 2018;2018:8319481.
Portela RC, Sharma I, Vahibe A, et al. Aspirin Use as a Risk Factor for Marginal Ulceration in Roux-en-Y Gastric Bypass Patients: A Meta-Analysis of 24,770 Patients. The American Surgeon. 2022:00031348221103647.
Wilson JA, Romagnuolo J, Byrne TK, Morgan K, Wilson FA. Predictors of endoscopic findings after Roux-en-Y gastric bypass. Am J Gastroenterol. 2006;101(10):2194-2199.
Azagury DE, Abu Dayyeh BK, Greenwalt IT, Thompson CC. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43(11):950-954.
Bhayani NH, Oyetunji TA, Chang DC, Cornwell EE, 3rd, Ortega G, Fullum TM. Predictors of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. J Surg Res. 2012;177(2):224-227.
Di Palma A, Liu B, Maeda A, Anvari M, Jackson T, Okrainec A. Marginal ulceration following Roux-en-Y gastric bypass: risk factors for ulcer development, recurrence and need for revisional surgery. Surg Endosc. 2021;35(5):2347-2353.
Bekhali Z, Sundbom M. Low Risk for Marginal Ulcers in Duodenal Switch and Gastric Bypass in a Well-Defined Cohort of 472 Patients. Obesity surgery. 2020;30(11):4422-4427.
Dittrich L, Schwenninger MV, Dittrich K, Pratschke J, Aigner F, Raakow J. Marginal ulcers after laparoscopic Roux-en-Y gastric bypass: analysis of the amount of daily and lifetime smoking on postoperative risk. Surg Obes Relat Dis. 2020;16(3):389-396.
El-Hayek K, Timratana P, Shimizu H, Chand B. Marginal ulcer after Roux-en-Y gastric bypass: what have we really learned? Surg Endosc. 2012;26(10):2789-2796.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283(15):2008–2012.
Sverdén E, Mattsson F, Sondén A, et al. Risk Factors for Marginal Ulcer After Gastric Bypass Surgery for Obesity: A Population-based Cohort Study. Ann Surg. 2016;263(4):733-737.
Süsstrunk J, Wartmann L, Mattiello D, Köstler T, Zingg U. Incidence and Prognostic Factors for the Development of Symptomatic and Asymptomatic Marginal Ulcers After Roux-en-Y Gastric Bypass Procedures. Obes Surg. 2021;31(7):3005-3014.
Boerlage TCC, Wolvers PJD, Bruin SC, et al. Upper endoscopy after Roux-en-Y gastric bypass: diagnostic yield and factors associated with relevant findings. Surg Obes Relat Dis. 2020;16(7):868-876.
Coblijn UK, Lagarde SM, de Castro SM, Kuiken SD, van Tets WF, van Wagensveld BA. The influence of prophylactic proton pump inhibitor treatment on the development of symptomatic marginal ulceration in Roux-en-Y gastric bypass patients: a historic cohort study. Surg Obes Relat Dis. 2016;12(2):246-252.
Edholm D, Ottosson J, Sundbom M. Importance of pouch size in laparoscopic Roux-en-Y gastric bypass: a cohort study of 14,168 patients. Surg Endosc. 2016;30(5):2011-2015.
Schulman AR, Abougergi MS, Thompson CC. H. pylori as a predictor of marginal ulceration: A nationwide analysis. Obesity (Silver Spring). 2017;25(3):522-526.
Wennerlund J, Gunnarsson U, Strigård K, Sundbom M. Acid-related complications after laparoscopic Roux-en-Y gastric bypass: risk factors and impact of proton pump inhibitors. Surg Obes Relat Dis. 2020;16(5):620-625.
Rodrigo DC, Jill S, Daniel M, Kimberly C, Maher EC. Which Factors Correlate with Marginal Ulcer After Surgery for Obesity? Obes Surg. 2020;30(12):4821-4827.
Coblijn UK, Lagarde SM, de Castro SMM, Kuiken SD, van Wagensveld BA. Symptomatic Marginal Ulcer Disease After Roux-en-Y Gastric Bypass: Incidence, Risk Factors and Management. Obesity Surgery. 2015;25(5):805-811.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634.
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455-463.
Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007;21(7):1090-1094.
Suerbaum S, Michetti P. Helicobacter pylori Infection. New England Journal of Medicine. 2002;347(15):1175-1186.
Eastwood GL. The Role of Smoking in Peptic Ulcer Disease. Journal of Clinical Gastroenterology. 1988;10.
Endoh K, Leung FW. Effects of smoking and nicotine on the gastric mucosa: a review of clinical and experimental evidence. Gastroenterology. 1994;107(3):864-878.
Wu WK, Cho CH. The pharmacological actions of nicotine on the gastrointestinal tract. J Pharmacol Sci. 2004;94(4):348-358.
Carter J, Chang J, Birriel TJ, et al. ASMBS position statement on preoperative patient optimization before metabolic and bariatric surgery. Surg Obes Relat Dis. 2021;17(12):1956-1976.
Chow A, Neville A, Kolozsvari N. Smoking in bariatric surgery: a systematic review. Surg Endosc. 2021;35(6):3047-3066.
Kang X, Zurita-Macias L, Hong D, Cadeddu M, Anvari M, Gmora S. A comparison of 30-day versus 90-day proton pump inhibitor therapy in prevention of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(5):1003-1007.
Author information
Authors and Affiliations
Contributions
Study conception and design: Azizullah Beran, Barham K. Abu Dayyeh, and Omar M. Ghanem; collection and acquisition of data: Azizullah Beran, Mohammad Shaear, Reem Matar, and Saif Al-Mudares; analysis and interpretation of data: Azizullah Beran, Mohammad Shaear, Saif Al-Mudares, and Ray Portela; drafting and editing of manuscript: Azizullah Beran, Mohammad Shaear, Mohammad Al-Haddad, Ishna Sharma, and Marita Salame; critical revision: Marita Salame, Mohammad Al-Haddad, Benjamin Clapp, Barham K. Abu Dayyeh, and Omar M. Ghanem. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
IRB approval
This study was deemed exempt by the Institutional Review Board.
Conflict of interest
Dr. Barham Abu Dayyeh has received consulting fee from the Endogenex, Endo-TAGSS, Metamodix, and BFKW; consulting fee and grant/research support from USGI, Cairn Diagnostics, Aspire Bariatrics, Boston Scientific; speaker honorarium from Olympus, Johnson and Johnson; speaker honorarium and grant/research support from Medtronic, Endogastric solutions; and research support/grant from the Apollo Endosurgery, and Spatz Medical. All other authors (Azizullah Beran, Mohammad Shaear, Saif Al-Mudares, Ishna Sharma, Reem Matar, Mohammad Al-Haddad, Marita Salame, Ray Portela, Benjamin Clapp, and Omar M. Ghanem) do not have conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beran, A., Shaear, M., Al-Mudares, S. et al. Predictors of marginal ulcer after gastric bypass: a systematic review and meta-analysis. J Gastrointest Surg 27, 1066–1077 (2023). https://doi.org/10.1007/s11605-023-05619-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05619-7