Abstract
Background
Although hypertension requiring medication (HTNm) is a well-known cardiovascular comorbidity, its association with postoperative outcomes is understudied. This study aimed to evaluate whether preoperative HTNm is independently associated with specific complications after pancreaticoduodenectomy.
Study Design
Adults undergoing elective pancreaticoduodenectomy were included from the 2014–2019 NSQIP-targeted pancreatectomy dataset. Multivariable regression models compared outcomes between patients with and without HTNm. Endpoints included significant complications, any complication, unplanned readmissions, length of stay (LOS), clinically relevant postoperative pancreatic fistula (CR-POPF), and cardiovascular and renal complications. A subgroup analysis excluded patients with diabetes, heart failure, chronic obstructive pulmonary disease, estimated glomerular filtration rate from serum creatinine (eGFRCr) < 60 ml/min per 1.73 m2, bleeding disorder, or steroid use.
Results
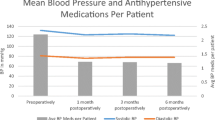
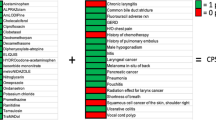
Among 14,806 patients, 52% had HTNm. HTNm was more common among older male patients with obesity, diabetes, congestive heart failure, chronic obstructive pulmonary disease, functional dependency, hard pancreatic glands, and cancer. After adjusting for demographics, preoperative comorbidities, and laboratory values, HTNm was independently associated with higher odds of significant complications (aOR 1.12, p = 0.020), any complication (aOR 1.11, p = 0.030), cardiovascular (aOR 1.78, p = 0.002) and renal (aOR 1.60, p = 0.020) complications, and unplanned readmissions (aOR 1.14, p = 0.040). In a subgroup analysis of patients without major preoperative comorbidity, HTNm remained associated with higher odds of significant complications (aOR 1.14, p = 0.030) and cardiovascular complications (aOR 1.76, p = 0.033).
Conclusions
HTNm is independently associated with cardiovascular and renal complications after pancreaticoduodenectomy and may need to be considered in preoperative risk stratification. Future studies are necessary to explore associations among underlying hypertension, specific antihypertensive medications, and postoperative outcomes to investigate potential risk mitigation strategies.



Similar content being viewed by others

Data Availability
The data that support the findings of this study is hosted by the American College of Surgeons on the ACS NSQIP Registry, available at https://www.facs.org/quality-programs/data-and-registries/acs-nsqip/.
Abbreviations
- HTNm:
-
Hypertension requiring medication
- ACS:
-
American College of Surgeons
- NSQIP:
-
National Surgical Quality Improvement Program
- CR-POPF:
-
Clinically relevant postoperative pancreatic fistula
- eGFRCr:
-
Estimated glomerular filtration rate from serum creatinine
- PE:
-
Pulmonary embolism
- DVT:
-
Deep vein thrombosis
- LOS:
-
Length of stay
- CHF:
-
Congestive heart failure
- COPD:
-
Chronic obstructive pulmonary disease
- ACE-I:
-
Angiotensin-converting enzyme inhibitors
References
Jakhmola CK, Kumar A. Whipple’s pancreaticoduodenectomy: Outcomes at a tertiary care hospital. Med J Armed Forces India. 2014;70(4):321-326. https://doi.org/10.1016/j.mjafi.2014.08.011
Greenblatt DY, Kelly KJ, Rajamanickam V, et al. Preoperative Factors Predict Perioperative Morbidity and Mortality After Pancreaticoduodenectomy. Ann Surg Oncol. 2011;18(8):2126-2135. https://doi.org/10.1245/s10434-011-1594-6
House MG, Fong Y, Arnaoutakis DJ, et al. Preoperative Predictors for Complications after Pancreaticoduodenectomy: Impact of BMI and Body Fat Distribution. J Gastrointest Surg. 2008;12(2):270-278. https://doi.org/10.1007/s11605-007-0421-7
American College of Surgeons, National Surgical Quality Improvement Program (NSQIP) Surgical Risk Calculator. https://riskcalculator.facs.org/RiskCalculator/. Accessed 14 Apr 2022
User Guide for the 2019 ACS NSQIP Participant Use Data File (PUF). American College of Surgeons, National Surgical Quality Improvement Program; 2020. https://www.facs.org/-/media/files/quality-programs/nsqip/nsqip_puf_userguide_2019.ashx. Accessed 14 Apr 2022
Al Abbas AI, Borrebach JD, Pitt HA, et al. Development of a Novel Pancreatoduodenectomy-Specific Risk Calculator: an Analysis of 10,000 Patients. J Gastrointest Surg. 2021;25(6):1503-1511. https://doi.org/10.1007/s11605-020-04725-0
Gleeson EM, Shaikh MF, Shewokis PA, et al. WHipple-ABACUS, a simple, validated risk score for 30-day mortality after pancreaticoduodenectomy developed using the ACS-NSQIP database. Surgery. 2016;160(5):1279-1287. https://doi.org/10.1016/j.surg.2016.06.040
Benedetto U, Sciarretta S, Roscitano A, et al. Preoperative Angiotensin-Converting Enzyme Inhibitors and Acute Kidney Injury After Coronary Artery Bypass Grafting. Ann Thorac Surg. 2008;86(4):1160-1165. https://doi.org/10.1016/j.athoracsur.2008.06.018
Tuman KJ, McCarthy RJ, O’Connor CJ, Holm WE, Ivankovich AD. Angiotensin-Converting Enzyme Inhibitors Increase Vasoconstrictor Requirements After Cardiopulmonary Bypass. Anesth Analg. 1995;80(3): 473-9. https://doi.org/10.1097/00000539-199503000-00007
Zhang Y, Ma L. Effect of preoperative angiotensin-converting enzyme inhibitor on the outcome of coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2015;47(5):788-795. https://doi.org/10.1093/ejcts/ezu298
O’Neal JB, Billings FT, Liu X, et al. Effect of Preoperative Beta-Blocker Use on Outcomes Following Cardiac Surgery. Am J Cardiol. 2017;120(8):1293-1297. https://doi.org/10.1016/j.amjcard.2017.07.012
Dorans KS, Mills KT, Liu Y, He J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7(11):e008888. https://doi.org/10.1161/JAHA.118.008888
Raval MV, Pawlik TM. Practical Guide to Surgical Data Sets: National Surgical Quality Improvement Program (NSQIP) and Pediatric NSQIP. JAMA Surg. 2018;153(8):764. https://doi.org/10.1001/jamasurg.2018.0486
About ACS NSQIP. American College of Surgeons. https://www.facs.org/quality-programs/acs-nsqip. Accessed 14 Apr 2022
User Guide for the 2020 ACS NSQIP Participant Use Data File (PUF). American College of Surgeons, National Surgical Quality Improvement Program; 2021. https://www.facs.org/-/media/files/quality-programs/nsqip/pt_nsqip_puf_userguide_2020.ashx. Accessed 5 Jan 2023
User Guide for the 2014 ACS NSQIP Participant Use Data File (PUF). American College of Surgeons, National Surgical Quality Improvement Program; 2015. https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2014.ashx. Accessed 5 Jan 2023
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161(3):584-591. https://doi.org/10.1016/j.surg.2016.11.014
Inker LA, Eneanya ND, Coresh J, et al. New Creatinine- and Cystatin C–Based Equations to Estimate GFR without Race. N Engl J Med. 2021;385(19):1737-1749. https://doi.org/10.1056/NEJMoa2102953
Misra S. Systemic hypertension and non-cardiac surgery. Indian J Anaesth. 2017;61(9):697. https://doi.org/10.4103/ija.IJA_377_17
Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019;322(13):1294-1304. https://doi.org/10.1001/jama.2019.14745
Belmont PJ, Goodman GP, Kusnezov NA, et al. Postoperative myocardial infarction and cardiac arrest following primary total knee and hip arthroplasty: rates, risk factors, and time of occurrence. J Bone Joint Surg Am. 2014;96(24):2025-2031. https://doi.org/10.2106/JBJS.N.00153
Ritchey MD, Gillespie C, Wozniak G, et al. Potential need for expanded pharmacologic treatment and lifestyle modification services under the 2017 ACC/AHA Hypertension Guideline. J Clin Hypertens. 2018;20(10):1377-1391. https://doi.org/10.1111/jch.13364
Venkatesan S, Jørgensen ME, Manning HJ, et al. Preoperative chronic beta-blocker prescription in elderly patients as a risk factor for postoperative mortality stratified by preoperative blood pressure: a cohort study. Br J Anaesth. 2019;123(2):118-125. https://doi.org/10.1016/j.bja.2019.03.042
Miller BC, Christein JD, Behrman SW, et al. A Multi-Institutional External Validation of the Fistula Risk Score for Pancreatoduodenectomy. J Gastrointest Surg. 2014;18(1):172-180. https://doi.org/10.1007/s11605-013-2337-8
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM. A Prospectively Validated Clinical Risk Score Accurately Predicts Pancreatic Fistula after Pancreatoduodenectomy. J Am Coll Surg. 2013;216(1):1-14. https://doi.org/10.1016/j.jamcollsurg.2012.09.002
Butturini G, Daskalaki D, Molinari E, Scopelliti F, Casarotto A, Bassi C. Pancreatic fistula: definition and current problems. J Hepatobiliary Pancreat Surg. 2008;15(3):247-251. https://doi.org/10.1007/s00534-007-1301-y
Lermite E, Pessaux P, Brehant O, et al. Risk factors of pancreatic fistula and delayed gastric emptying after pancreaticoduodenectomy with pancreaticogastrostomy. J Am Coll Surg. 2007;204(4):588-596. https://doi.org/10.1016/j.jamcollsurg.2007.01.018
Zorbas K, Wu J, Reddy S, Esnaola N, Karachristos A. Obesity affects outcomes of pancreatoduodenectomy. Pancreatol Off J Int Assoc Pancreatol IAP Al. 2021;21(4):824-832. https://doi.org/10.1016/j.pan.2021.02.019
Jiang HY, Kohtakangas EL, Asai K, Shum JB. Predictive Power of the NSQIP Risk Calculator for Early Post-Operative Outcomes After Whipple: Experience from a Regional Center in Northern Ontario. J Gastrointest Cancer. 2018;49(3):288-294. https://doi.org/10.1007/s12029-017-9949-2
Eshuis WJ, van der Gaag NA, Rauws EAJ, et al. Therapeutic delay and survival after surgery for cancer of the pancreatic head with or without preoperative biliary drainage. Ann Surg. 2010;252(5):840-849. https://doi.org/10.1097/SLA.0b013e3181fd36a2
Yang F, Jin C, Zou C, et al. Delaying surgery after preoperative biliary drainage does not increase surgical morbidity after pancreaticoduodenectomy. Surgery. 2019;166(6):1004-1010. https://doi.org/10.1016/j.surg.2019.07.012
Fuks D, Piessen G, Huet E, et al. Life-threatening postoperative pancreatic fistula (grade C) after pancreaticoduodenectomy: incidence, prognosis, and risk factors. Am J Surg. 2009;197(6):702-709. https://doi.org/10.1016/j.amjsurg.2008.03.004
Funding
P.C.C. was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, UCSF-CTSI Grant Number TL1 TR001871, and the National Cancer Institute, National Institutes of Health, Grant Number T32CA25107001. M.Y. is funded by the National Clinician Scholars Program.
Author information
Authors and Affiliations
Contributions
All authors listed have contributed substantially to this work, from conceptualization and design to analysis and interpretation of the data. All authors were involved in either drafting or critically revising the manuscript. Statistical analysis was performed by J. Lin under the supervision of P. Conroy, J. Feng, and M. Adam.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Disclaimer
These contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
This work was accepted for oral presentation at the Scientific Forum of the American College of Surgeons Clinical Congress 2022, to be held in San Diego, CA, from October 16 to 20, 2022.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lin, J.J., Conroy, P.C., Romero-Hernandez, F. et al. Hypertension Requiring Medication Use: a Silent Predictor of Poor Outcomes After Pancreaticoduodenectomy. J Gastrointest Surg 27, 328–336 (2023). https://doi.org/10.1007/s11605-022-05577-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05577-6