Abstract
Background
In contrast to pancreatic ductal adenocarcinoma (PDAC), the risks of pancreatectomy for mucinous pancreatic cysts (MCs) are balanced against the putative goal of removing potentially malignant tumors. Despite undergoing similar operations, different rates of perioperative complications and morbidity between MC and PDAC patient populations may affect recommendations for resection. We therefore sought to compare the rates of postoperative complications between patients undergoing pancreatectomies for MCs or PDAC.
Methods
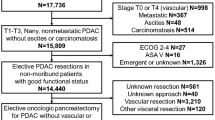
A prospectively maintained institutional database was used to identify patients who underwent surgical resection for MCs or PDAC from July 2011 to August 2019. Patient demographics, complications, and perioperative data were compared between groups.
Results
A total of 103 patients underwent surgical resection for MCs and 428 patients underwent resection for PDAC. Combined major 90-day postoperative complications were similar between MC and PDAC patients undergoing pancreaticoduodenectomy (PD, 32.5% vs. 20.0%, p = 0.068) or distal pancreatectomy (DP, 30.2% vs. 20.5%, p = 0.172). The most frequent complications were postoperative pancreatic fistula (POPF), abscess, and postoperative bleeding. The incidence of 90-day ISGPS Grade B/C POPF was higher in cyst patients undergoing PD (17.5% vs. 4.1%, p = 0.003) but not DP (25.4% vs. 20.5%, p = 0.473). No significant differences in operative time or length of stay between MCs and PDAC cohorts were observed.
Conclusions
POPFs occur more frequently and at higher grades in patients undergoing PD for MCs than for PDAC and should inform patient selection. Accordingly, the perioperative management of MC patients undergoing PD should emphasize POPF risk mitigation.

Similar content being viewed by others
Data Availability
The data supporting the findings and conclusions of this study is available within the article.
References
Megibow AJ, Baker ME, Morgan DE, Kamel IR, Sahani DV, Newman E, et al. Management of incidental pancreatic cysts: a white paper of the ACR Incidental Findings Committee. Journal of the American College of Radiology: JACR. 2017;14(7):911-23.
Fernández-del Castillo C, Targarona J, Thayer SP, Rattner DW, Brugge WR, Warshaw AL. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Archives of surgery (Chicago, Ill: 1960). 2003;138(4):427–3; discussion 33–4
Moris M, Bridges MD, Pooley RA, Raimondo M, Woodward TA, Stauffer JA, et al. Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2016;14(4):585-93.e3.
Gardner TB, Glass LM, Smith KD, Ripple GH, Barth RJ, Klibansky DA, et al. Pancreatic cyst prevalence and the risk of mucin-producing adenocarcinoma in US adults. The American journal of gastroenterology. 2013;108(10):1546-50.
Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR American journal of roentgenology. 2008;191(3):802-7.
Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. The American journal of gastroenterology. 2010;105(9):2079-84.
Zhang XM, Mitchell DG, Dohke M, Holland GA, Parker L. Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology. 2002;223(2):547-53.
Stark A, Donahue TR, Reber HA, Hines OJ. Pancreatic cyst disease: a review. Jama. 2016;315(17):1882-93.
Salvia R, Fernández-del Castillo C, Bassi C, Thayer SP, Falconi M, Mantovani W, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Annals of surgery. 2004;239(5):678–85; discussion 85–7.
Ferrone CR, Correa-Gallego C, Warshaw AL, Brugge WR, Forcione DG, Thayer SP, et al. Current trends in pancreatic cystic neoplasms. Archives of surgery (Chicago, Ill: 1960). 2009;144(5):448–54.
Shimizu Y, Yamaue H, Maguchi H, Yamao K, Hirono S, Osanai M, et al. Predictors of malignancy in intraductal papillary mucinous neoplasm of the pancreas: analysis of 310 pancreatic resection patients at multiple high-volume centers. Pancreas. 2013;42(5):883-8.
Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology: official journal of the International Association of Pancreatology (IAP) [et al]. 2012;12(3):183–97.
Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology: official journal of the International Association of Pancreatology (IAP) [et al]. 2017;17(5):738–53.
Wada K, Kozarek RA, Traverso LW. Outcomes following resection of invasive and noninvasive intraductal papillary mucinous neoplasms of the pancreas. American journal of surgery. 2005;189(5):632–6; discussion 7.
Schnelldorfer T, Sarr MG, Nagorney DM, Zhang L, Smyrk TC, Qin R, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Archives of surgery (Chicago, Ill: 1960). 2008;143(7):639–46; discussion 46.
Park JW, Jang JY, Kang MJ, Kwon W, Chang YR, Kim SW. Mucinous cystic neoplasm of the pancreas: is surgical resection recommended for all surgically fit patients? Pancreatology: official journal of the International Association of Pancreatology (IAP) [et al]. 2014;14(2):131–6.
Wasif N, Bentrem DJ, Farrell JJ, Ko CY, Hines OJ, Reber HA, et al. Invasive intraductal papillary mucinous neoplasm versus sporadic pancreatic adenocarcinoma: a stage-matched comparison of outcomes. Cancer. 2010;116(14):3369-77.
Poultsides GA, Reddy S, Cameron JL, Hruban RH, Pawlik TM, Ahuja N, et al. Histopathologic basis for the favorable survival after resection of intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma of the pancreas. Annals of surgery. 2010;251(3):470-6.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161(3):584-91.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761-8.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142(1):20-5.
Zhang H, Zhu F, Shen M, Tian R, Shi CJ, Wang X, et al. Systematic review and meta-analysis comparing three techniques for pancreatic remnant closure following distal pancreatectomy. The British journal of surgery. 2015;102(1):4-15.
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM, Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. Journal of the American College of Surgeons. 2013;216(1):1-14.
Denbo JW, Slack RS, Bruno M, Cloyd JM, Prakash L, Fleming JB, et al. Selective perioperative administration of pasireotide is more cost-effective than routine administration for pancreatic fistula prophylaxis. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2017;21(4):636-46.
Denbo JW, Bruno M, Dewhurst W, Kim MP, Tzeng CW, Aloia TA, et al. Risk-stratified clinical pathways decrease the duration of hospitalization and costs of perioperative care after pancreatectomy. Surgery. 2018;164(3):424-31.
Duconseil P, Périnel J, Autret A, Adham M, Sauvanet A, Chiche L, et al. Resectable invasive IPMN versus sporadic pancreatic adenocarcinoma of the head of the pancreas: should these two different diseases receive the same treatment? A matched comparison study of the French Surgical Association (AFC). European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2017;43(9):1704-10.
Newhook TE, LaPar DJ, Lindberg JM, Bauer TW, Adams RB, Zaydfudim VM. Morbidity and mortality of pancreaticoduodenectomy for benign and premalignant pancreatic neoplasms. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2015;19(6):1072-7.
Hwang RF, Wang H, Lara A, Gomez H, Chang T, Sieffert N, et al. Development of an integrated biospecimen bank and multidisciplinary clinical database for pancreatic cancer. Annals of surgical oncology. 2008;15(5):1356-66.
Balachandran A, Bhosale PR, Charnsangavej C, Tamm EP. Imaging of pancreatic neoplasms. Surgical oncology clinics of North America. 2014;23(4):751-88.
Katz MH, Wang H, Balachandran A, Bhosale P, Crane CH, Wang X, et al. Effect of neoadjuvant chemoradiation and surgical technique on recurrence of localized pancreatic cancer. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2012;16(1):68–78; discussion -9.
Newhook TE, Vega EA, Vreeland TJ, Prakash L, Dewhurst WL, Bruno ML, et al. Early postoperative drain fluid amylase in risk-stratified patients promotes tailored post-pancreatectomy drain management and potential for accelerated discharge. Surgery. 2020;167(2):442-7.
Arango NP, Prakash LR, Chiang YJ, Dewhurst WL, Bruno ML, Ikoma N, et al. Risk-stratified pancreatectomy clinical pathway implementation and delayed gastric emptying. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2021;25(9):2221-30.
Newton AD, Newhook TE, Bruno ML, Prakash L, Chiang YJ, Arango NP, et al. Iterative Changes in Risk-Stratified Pancreatectomy Clinical Pathways and Accelerated Discharge After Pancreaticoduodenectomy. J Gastrointest Surg. 2022;26(5):1054–62.
Schwarz L, Bruno M, Parker NH, Prakash L, Mise Y, Lee JE, et al. Active surveillance for adverse events within 90 days: the standard for reporting surgical outcomes after pancreatectomy. Annals of surgical oncology. 2015;22(11):3522-9.
Porembka MR, Hall BL, Hirbe M, Strasberg SM. Quantitative weighting of postoperative complications based on the accordion severity grading system: demonstration of potential impact using the American College of Surgeons National Surgical Quality Improvement Program. Journal of the American College of Surgeons. 2010;210(3):286-98.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8-13.
Tzeng CW, Fleming JB, Lee JE, Wang X, Pisters PW, Vauthey JN, et al. Yield of clinical and radiographic surveillance in patients with resected pancreatic adenocarcinoma following multimodal therapy. HPB: the official journal of the International Hepato Pancreato Biliary Association. 2012;14(6):365–72.
Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, et al. Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy: analysis of 2026 resections from the international, multi-institutional Distal Pancreatectomy Study Group. Annals of surgery. 2019;269(1):143-9.
Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M, Maupin G, Bassi C, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy in 1,507 patients: a report from the Pancreatic Anastomotic Leak Study Group. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2007;11(11):1451–8; discussion 9.
Wellner UF, Kayser G, Lapshyn H, Sick O, Makowiec F, Höppner J, et al. A simple scoring system based on clinical factors related to pancreatic texture predicts postoperative pancreatic fistula preoperatively. HPB: the official journal of the International Hepato Pancreato Biliary Association. 2010;12(10):696–702.
Tzeng CW, Katz MH, Fleming JB, Lee JE, Pisters PW, Holmes HM, et al. Morbidity and mortality after pancreaticoduodenectomy in patients with borderline resectable type C clinical classification. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2014;18(1):146–55; discussion 55–6.
Tzeng CW, Fleming JB, Lee JE, Xiao L, Pisters PW, Vauthey JN, et al. Defined clinical classifications are associated with outcome of patients with anatomically resectable pancreatic adenocarcinoma treated with neoadjuvant therapy. Annals of surgical oncology. 2012;19(6):2045-53.
Katz MH, Pisters PW, Evans DB, Sun CC, Lee JE, Fleming JB, et al. Borderline resectable pancreatic cancer: the importance of this emerging stage of disease. Journal of the American College of Surgeons. 2008;206(5):833–46; discussion 46–8.
Funding
This work was supported by National Institutes of Health T32 CA 009599 and the MD Anderson Cancer Center support grant (P30 CA016672).
Author information
Authors and Affiliations
Contributions
Conception and design, and/or acquisition of data, and/or analysis and interpretation of data: all authors. Drafting the article or revising it critically for important intellectual content: all authors. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Permissions
All material presented in the above manuscript is original.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting Presentation: The Society for Surgery of the Alimentary Tract (SSAT) Virtual 62nd Annual Meeting, May 21–23, 2021.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Donovan, E.C., Prakash, L.R., Chiang, YJ. et al. Incidence of Postoperative Complications Following Pancreatectomy for Pancreatic Cystic Lesions or Pancreatic Cancer. J Gastrointest Surg 27, 319–327 (2023). https://doi.org/10.1007/s11605-022-05534-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05534-3