Abstract
Purpose
We aimed to compare the efficacy of hepatic resection and percutaneous ablation for resectable caudate HCC within Milan criteria and to investigate the prognostic factors.
Methods
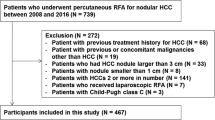
Between August 2006 and August 2020, a total of 67 eligible patients with resectable caudate HCC within Milan criteria in three centers were retrospectively analyzed and divided into hepatic resection group (n = 46) and percutaneous ablation group (n = 21). Recurrence-free survival (RFS) and overall survival (OS) rates were compared between groups of hepatic resection and percutaneous ablation for these resectable caudate HCC patients with Kaplan–Meier curves and log-rank test. Univariable and multivariable Cox regression analyses were performed to identify the prognostic factors of RFS and OS.
Results
The 1-, 3-, and 5-year OS rates were 97.6%, 83.6%, and 71.5% for the hepatic resection group, and 89.4%, 58.5%, and 48.8% for the percutaneous ablation group (P = 0.032). The corresponding RFS rates were 77.6%, 47.9%, and 42.6% for the hepatic resection group, and 40.5%, 23.2%, and 15.4% for the percutaneous ablation group (P = 0.010). According to the univariable and multivariable analyses, tumor type (first recurrence) (HR = 3.54; 95%CI, 1.49–8.37; P = 0.004) was a significant independent prognostic factor of RFS for caudate HCC patients after resection or ablation, while total bilirubin (HR = 1.02; 95%CI, 1.01–1.04; P = 0.006) and treatment strategy (HR = 5.97; 95%CI, 1.48–24.12; P = 0.012) were significant independent prognostic factors of OS.
Conclusions
Hepatic resection appears to outperform percutaneous ablation for caudate HCC patients within Milan criteria.




Similar content being viewed by others
References
World Health Organization. Projections of mortality and causes of death, 2016 to 2060. http://www.who.int/healthinfo/global_burden_disease/projections/en/.
Yamamoto T, Kubo S, Shuto T, Ichikawa T, Ogawa M, Hai S, Sakabe K, Tanaka S, Uenishi T, Ikebe T, Tanaka H, Kaneda K, Hirohashi K. Surgical strategy for hepatocellular carcinoma originating in the caudate lobe. Surgery. 2004;135:595-603.
Miyayama S, Yamashiro M, Hattori Y, Orito N, Matsui K, Tsuji K, Yoshida M, Matsui O. Angiographic evaluation of feeding arteries of hepatocellular carcinoma in the caudate lobe of the liver. Cardiovasc Intervent Radiol. 2011;34:1244-1253.
Liu P, Yang JM, Niu WY, Kan T, Xie F, Li DQ, Wang Y, Zhou YM. Prognostic factors in the surgical treatment of caudate lobe hepatocellular carcinoma. World J Gastroenterol. 2010;16:1123-1128.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699.
Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH, Dematteo RP. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Annals of surgery. 2003;238:315-323.
Takayama T, Midorikawa Y, Higaki T, Nakayama H, Moriguchi M, Aramaki O, Yamazaki S, Aoki M, Kogure K, Makuuchi M. Algorithm for Resecting Hepatocellular Carcinoma in the Caudate Lobe. Ann Surg. 2021 Jun 1;273:e222-e229.
Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ, Lin XJ, Lau WY. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Annals of surgery. 2006;243:321-328.
Kariyama K, Nouso K, Wakuta A, Kishida M, Nishimura M, Wada N, Higashi T. Percutaneous radiofrequency ablation for treatment of hepatocellular carcinoma in the caudate lobe. AJR Am J Roentgenol. 2011;197:W571-W575.
Nishigaki Y, Tomita E, Hayashi H, Suzuki Y, Iritani S, Kato T, Yamada T. Efficacy and safety of radiofrequency ablation for hepatocellular carcinoma in the caudate lobe of the liver. Hepatol Res. 2013;43:467-474.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236.
Liu B, Long J, Wang W, Huang T, Xie X, Chen S, Huang G, Jiang C, Ye J, Long H, Xie X, Kuang M. Predictive factors of treatment outcomes after percutaneous ablation of hepatocellular carcinoma in the caudate lobe: a retrospective study. BMC Cancer. 2019;19:699.
Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314.
Bruix J, Reig M, Sherman M. Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology. 2016;150:835-53.
Kulik LM, Atassi B, van Holsbeeck L, Souman T, Lewandowski RJ, Mulcahy MF, Hunter RD, Nemcek AA Jr, Abecassis MM, Haines KG 3rd, Salem R. Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol. 2006;94:572-86.
Sangro B, Iñarrairaegui M, Bilbao JI. Radioembolization for hepatocellular carcinoma. J Hepatol. 2012;56:464-73.
Zhou Y, Zhang X, Wu L, Xu D, Li B. Surgical outcomes of hepatocellular carcinoma originating from caudate lobe. ANZ journal of surgery. 2013;83:275-279.
Ibrahim SM, Kulik L, Baker T, Ryu RK, Mulcahy MF, Abecassis M, Salem R, Lewandowski RJ. Treating and downstaging hepatocellular carcinoma in the caudate lobe with yttrium-90 radioembolization. Cardiovascular and interventional radiology. 2012;35:1094-1101.
Salem R, Gordon AC, Mouli S, Hickey R, Kallini J, Gabr A, Mulcahy MF, Baker T, Abecassis M, Miller FH, Yaghmai V, Sato K, Desai K, Thornburg B, Benson AB, Rademaker A, Ganger D, Kulik L, Lewandowski RJ. Y90 Radioembolization Significantly Prolongs Time to Progression Compared With Chemoembolization in Patients With Hepatocellular Carcinoma. Gastroenterology. 2016;151:1155-1163.
Gil-alzugaray B, Chopitea A, Iñarrairaegui M, Bilbao JI, Rodriguez-fraile M, Rodriguez J, Benito A, Dominguez I, D'avola D, Herrero JI, Quiroga J, Prieto J, Sangro B. Prognostic factors and prevention of radioembolization-induced liver disease. Hepatology. 2013;57:1078-1087.
Kumon M. Anatomical Study of the Caudate Lobe with Special Reference to Portal Venous and Biliary Branches Using Corrosion Liver Casts and Clinical Application. Liver Cancer. 2017;6:161-170.
Sakamoto Y, Nara S, Hata S, Yamamoto Y, Esaki M, Shimada K, Kosuge T. Prognosis of patients undergoing hepatectomy for solitary hepatocellular carcinoma originating in the caudate lobe. Surgery. 2011;150:959-967.
Shimada S, Kamiyama T, Yokoo H, Orimo T, Nagatsu A, Ohata T, Kamachi H, Taketomi A. Prognoses and Clinicopathological Characteristics for Hepatocellular Carcinoma Originating from the Caudate Lobe After Surgery. World Journal of Surgery. 2019;43:1085-1093.
Zhou XF, Xia Q, Xie SJ. The Clinical Efficacy of Surgical Removal of Hepatocellular Carcinoma in Caudate Lobe in the Chinese Population: A Case-control Study. Surg Laparosc Endosc Percutan Tech. 2020;30:351-355.
Liu F, Wei Y, Li B. Laparoscopic Isolated Total Caudate Lobectomy for Hepatocellular Carcinoma Located in the Paracaval Portion of the Cirrhotic Liver. Annals of Surgical Oncology. 2019;26:2980.
Liu W, Zou R, Wang C, Qiu J, Shen J, Liao Y, Yang Z, Zhang Y, Wang Y, Yuan Y, Li K, Zuo D, He W, Zheng Y, Li B, Yuan Y. Microwave ablation versus resection for hepatocellular carcinoma within the Milan criteria: a propensity-score analysis. Ther Adv Med Oncol. 2019;11:1758835919874652.
Cucchetti A, Piscaglia F, Cescon M, Colecchia A, Ercolani G, Bolondi L, Pinna AD. Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. J Hepatol. 2013;59:300-307.
Lee BC, Liu KL, Wu CH, Huang KW, Ho CM, Hu RH, Ho MC, Wu YM, Lee PH, Liang PC. Comparison of Radiofrequency Ablation and Transarterial Chemoembolization for Hepatocellular Carcinoma in the Caudate Lobe. Cardiovasc Intervent Radiol. 2018;41:1699-1707.
He W, Li B, Zheng Y, Zou R, Shen J, Cheng D, Tao Q, Liu W, Li Q, Chen G, Yuan Y. Resection vs. ablation for alpha-fetoprotein positive hepatocellular carcinoma within the Milan criteria: a propensity score analysis. Liver Int. 2016;36:1677-1687.
Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, Imamura H, Sugawara Y, Kokudo N, Makuuchi M. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology. 2008;134:1908-16.
Funding
The article is supported by the National Science Fund for Distinguished Young Scholars (No. 81825013), the National Natural Science Foundation of China (No. 82003105), the National Natural Science Foundation of China (No. 81801703), and the Natural Science Foundation of Guangdong, China (No. 2018A030310326).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, W., Tan, J., Li, B. et al. Comparison of Hepatic Resection with Percutaneous Ablation for Hepatocellular Carcinoma in the Caudate Lobe Within Milan Criteria. J Gastrointest Surg 26, 323–332 (2022). https://doi.org/10.1007/s11605-021-05111-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05111-0