Abstract
Background
Socioeconomics, demographics, and insurance status play roles in healthcare access. Considering the limited resources available, understanding the relative impact of disparities helps prioritize programs designed to overcome them. This study evaluates gastrointestinal cancer care disparity by comparing the impact of different patient factors across oncologic care metrices.
Methods
A multi-institutional prospectively maintained cancer database was reviewed retrospectively for gastrointestinal cancers (esophagus, stomach, liver, pancreas, colorectal, and hepato-pancreato-biliary) from 2007 to 2017 to assess quality of care provided. Quality of care was defined by clinical course following national guidelines for the respective cancer. This included surgical intervention, chemotherapy, palliative care, and minimal delay to treatment/diagnosis. Logistic regression was used to adjust for confounders and identify factors associated with quality of care. Kaplan-Meier survival curves were compared using log-rank test.
Results
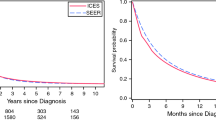
One thousand seventy-two patients were identified. Survival improved in patients with private insurance compared to government-funded options [median overall survival (mOS) 57.8 vs. 21.2 months; P < .001]. Private insurance also correlated with earlier stage at diagnosis [stages I–II = 50.9% vs. 37.5%, stages III–IV = 37.7% vs. 49.1%, P < .001], increased chemotherapy use [44.2% vs. 37.1%, P < .001], and more surgical intervention [62.4% vs. 48.8%, P < .001]. Outcomes were inferior for Black Americans, including trend towards lower rate of surgical treatment [42% vs. 54%, P = .058] and worse survival in private insurance carriers [mOS 7.8 vs. 57.8 months, P = .021] and those with early stage disease [mOS 39.2 vs. 81.5 months, P = .045] compared to White counterparts.
Conclusions
Insurance status has the strongest impact on the quality of gastrointestinal oncologic care with negative synergistic negative effect of race for Black Americans. While governmental programs aim to improve equality of care, there remains significant disparity compared to private insurance. Moreover, private insurance doesn’t correct disparity for Black Americans, suggesting the need to address racial imbalances in cancer care.



Similar content being viewed by others
References
Jackson CS, Oman M, Patel AM, Vega KJ. Health disparities in colorectal cancer among racial and ethnic minorities in the United States. J Gastrointest Oncol. 2016;7(Suppl 1):S32-43. doi:https://doi.org/10.3978/j.issn.2078-6891.2015.039.
Robbins AS, Siegel RL, Jemal A. Racial disparities in stage-specific colorectal cancer mortality rates from 1985 to 2008. J Clin Oncol. 2012;30(4):401-5. doi:https://doi.org/10.1200/jco.2011.37.5527.
Govindarajan R, Shah RV, Erkman LG, Hutchins LF. Racial differences in the outcome of patients with colorectal carcinoma. Cancer. 2003;97(2):493-8. doi:https://doi.org/10.1002/cncr.11067.
Le H, Ziogas A, Lipkin SM, Zell JA. Effects of socioeconomic status and treatment disparities in colorectal cancer survival. Cancer Epidemiol Biomarkers Prev. 2008;17(8):1950-62. doi:https://doi.org/10.1158/1055-9965.Epi-07-2774.
Lee W, Nelson R, Mailey B, Duldulao MP, Garcia-Aguilar J, Kim J. Socioeconomic factors impact colon cancer outcomes in diverse patient populations. J Gastrointest Surg. 2012;16(4):692-704. doi:https://doi.org/10.1007/s11605-011-1809-y.
Ikoma N, Cormier JN, Feig B, Du XL, Yamal JM, Hofstetter W et al. Racial disparities in preoperative chemotherapy use in gastric cancer patients in the United States: Analysis of the National Cancer Data Base, 2006-2014. Cancer. 2018;124(5):998-1007. doi:https://doi.org/10.1002/cncr.31155.
Stessin AM, Sherr DL. Demographic disparities in patterns of care and survival outcomes for patients with resected gastric adenocarcinoma. Cancer Epidemiol Biomarkers Prev. 2011;20(2):223-33. doi:https://doi.org/10.1158/1055-9965.Epi-10-0158.
Nipp R, Tramontano AC, Kong CY, Pandharipande P, Dowling EC, Schrag D et al. Disparities in cancer outcomes across age, sex, and race/ethnicity among patients with pancreatic cancer. Cancer Med. 2018;7(2):525-35. doi:https://doi.org/10.1002/cam4.1277.
Wright MJ, Overton HN, Teinor JA, Ding D, Burkhart RA, Cameron JL et al. Disparities in the use of chemotherapy in patients with resected pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2019. doi:https://doi.org/10.1007/s11605-019-04311-z.
Shah A, Chao KS, Ostbye T, Castleberry AW, Pietrobon R, Gloor B et al. Trends in racial disparities in pancreatic cancer surgery. J Gastrointest Surg. 2013;17(11):1897-906. doi:https://doi.org/10.1007/s11605-013-2304-4.
Singal V, Singal AK, Kuo YF. Racial disparities in treatment for pancreatic cancer and impact on survival: a population-based analysis. J Cancer Res Clin Oncol. 2012;138(4):715-22. doi:https://doi.org/10.1007/s00432-012-1156-8.
Artinyan A, Mailey B, Sanchez-Luege N, Khalili J, Sun CL, Bhatia S et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116(5):1367-77. doi:https://doi.org/10.1002/cncr.24817.
Markt SC, Tang T, Cronin AM, Katz IT, Howitt BE, Horowitz NS et al. Insurance status and cancer treatment mediate the association between race/ethnicity and cervical cancer survival. PLoS One. 2018;13(2):e0193047. doi:https://doi.org/10.1371/journal.pone.0193047.
Silber JH, Rosenbaum PR, Ross RN, Reiter JG, Niknam BA, Hill AS et al. Disparities in breast cancer survival by socioeconomic status despite medicare and medicaid insurance. Milbank Q. 2018;96(4):706-54. doi:https://doi.org/10.1111/1468-0009.12355.
Akinyemiju T, Sakhuja S, Vin-Raviv N. Racial and socio-economic disparities in breast cancer hospitalization outcomes by insurance status. Cancer Epidemiol. 2016;43:63-9. doi:https://doi.org/10.1016/j.canep.2016.06.011.
Tantraworasin A, Taioli E, Liu B, Flores RM, Kaufman AJ. The influence of insurance type on stage at presentation, treatment, and survival between Asian American and non-Hispanic White lung cancer patients. Cancer Med. 2018;7(5):1612-29. doi:https://doi.org/10.1002/cam4.1331.
Kinlock BL, Thorpe RJ, Jr., Howard DL, Bowie JV, Ross LE, Fakunle DO et al. Racial disparity in time between first diagnosis and initial treatment of prostate cancer. Cancer Control. 2016;23(1):47-51. doi:https://doi.org/10.1177/107327481602300108.
. CMS. 2019. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMS-Fast-Facts. .
Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the Patient Protection and Affordable Care Act. JAMA Oncol. 2018;4(12):1713-20. doi:https://doi.org/10.1001/jamaoncol.2018.3467.
Wright BJ, Conlin AK, Allen HL, Tsui J, Carlson MJ, Li HF. What does Medicaid expansion mean for cancer screening and prevention? Results from a randomized trial on the impacts of acquiring Medicaid coverage. Cancer. 2016;122(5):791-7. doi:https://doi.org/10.1002/cncr.29802.
Eguia E, Cobb AN, Kothari AN, Molefe A, Afshar M, Aranha GV et al. Impact of the Affordable Care Act (ACA) Medicaid expansion on cancer admissions and surgeries. Ann Surg. 2018;268(4):584-90. doi:https://doi.org/10.1097/sla.0000000000002952.
Naghavi AO, Echevarria MI, Grass GD, Strom TJ, Abuodeh YA, Ahmed KA et al. Having Medicaid insurance negatively impacts outcomes in patients with head and neck malignancies. Cancer. 2016;122(22):3529-37. doi:https://doi.org/10.1002/cncr.30212.
Smith AJB, Fader AN. Effects of the Affordable Care Act on young women with gynecologic cancers. Obstet Gynecol. 2018;131(6):966-76. doi:https://doi.org/10.1097/aog.0000000000002592.
Parikh-Patel A, Morris CR, Kizer KW. Disparities in quality of cancer care: the role of health insurance and population demographics. Medicine (Baltimore). 2017;96(50):e9125. doi:https://doi.org/10.1097/md.0000000000009125.
Pulte D, Jansen L, Brenner H. Social disparities in survival after diagnosis with colorectal cancer: contribution of race and insurance status. Cancer Epidemiol. 2017;48:41-7. doi:https://doi.org/10.1016/j.canep.2017.03.004.
Lukavsky R, Sariego J. Insurance status effects on stage of diagnosis and surgical options used in the treatment of breast cancer. South Med J. 2015;108(5):258-61. doi:https://doi.org/10.14423/smj.0000000000000281.
Moaven O, Richman JS, Reddy S, Wang T, Heslin MJ, Contreras CM. Healthcare disparities in outcomes of patients with resectable pancreatic cancer. Am J Surg. 2019;217(4):725-31. doi:https://doi.org/10.1016/j.amjsurg.2018.12.007.
Xiao D, Zheng C, Jindal M, Johnson LB, DeLeire T, Shara N et al. Medicaid expansion and disparity reduction in surgical cancer care at high-quality hospitals. J Am Coll Surg. 2018;226(1):22-9. doi:https://doi.org/10.1016/j.jamcollsurg.2017.09.012.
Loehrer AP, Song Z, Haynes AB, Chang DC, Hutter MM, Mullen JT. Impact of health insurance expansion on the treatment of colorectal cancer. J Clin Oncol. 2016;34(34):4110-5. doi:https://doi.org/10.1200/jco.2016.68.5701.
Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on racial and ethnic disparities in health insurance coverage. Am J Public Health. 2016;106(8):1416-21. doi:https://doi.org/10.2105/ajph.2016.303155.
Moskowitz GB, Stone J, Childs A. Implicit stereotyping and medical decisions: unconscious stereotype activation in practitioners' thoughts about African Americans. Am J Public Health. 2012;102(5):996-1001. doi:https://doi.org/10.2105/ajph.2011.300591.
Hausmann LR, Mor M, Hanusa BH, Zickmund S, Cohen PZ, Grant R et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982-8. doi:https://doi.org/10.1007/s11606-010-1399-5.
Powell IJ, Bock CH, Ruterbusch JJ, Sakr W. Evidence supports a faster growth rate and/or earlier transformation to clinically significant prostate cancer in black than in white American men, and influences racial progression and mortality disparity. J Urol. 2010;183(5):1792-6. doi:https://doi.org/10.1016/j.juro.2010.01.015.
Gild P, Wankowicz SA, Sood A, von Landenberg N, Friedlander DF, Alanee S et al. Racial disparity in quality of care and overall survival among black vs. white patients with muscle-invasive bladder cancer treated with radical cystectomy: a national cancer database analysis. Urol Oncol. 2018;36(10):469.e1-469.e11. doi:https://doi.org/10.1016/j.urolonc.2018.07.012.
Dimick J, Ruhter J, Sarrazin MV, Birkmeyer JD. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Millwood). 2013;32(6):1046-53. doi:https://doi.org/10.1377/hlthaff.2011.1365.
Wudel LJ, Jr., Chapman WC, Shyr Y, Davidson M, Jeyakumar A, Rogers SO, Jr. et al. Disparate outcomes in patients with colorectal cancer: effect of race on long-term survival. Arch Surg. 2002;137(5):550-4; discussion 4-6. doi:https://doi.org/10.1001/archsurg.137.5.550.
Shi L, Chen CC, Nie X, Zhu J, Hu R. Racial and socioeconomic disparities in access to primary care among people with chronic conditions. J Am Board Fam Med. 2014;27(2):189-98. doi:https://doi.org/10.3122/jabfm.2014.02.130246.
Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575-84. doi:https://doi.org/10.1056/NEJMsa040609.
Lansdorp-Vogelaar I, Kuntz KM, Knudsen AB, van Ballegooijen M, Zauber AG, Jemal A. Contribution of screening and survival differences to racial disparities in colorectal cancer rates. Cancer Epidemiol Biomarkers Prev. 2012;21(5):728-36. doi:https://doi.org/10.1158/1055-9965.Epi-12-0023.
U.S. Census Bureau QuickFacts: Massachusetts. 2020. https://www.census.gov/quickfacts/MA.
Acknowledgements
No funding was received for this research; no further acknowledgements.
Funding
This research did not receive any specific funding from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Omid Salehi, MD: conception/design of the work, data collection/acquisition, data analysis/interpretation, drafting article, revision of article, final approval
Eduardo A. Vega, MD: conception/design of the work, data collection, data analysis/interpretation, revision of article, final approval
Christopher Lathan, MD: conception/design of the work, revision of article, final approval
Daria James, CTR: data acquisition, revision of article, final approval
Olga Kozyreva, MD: conception/design of the work, data acquisition, revision of article, final approval
Sylvia V. Alarcon, MD: conception/design of the work, revision of article, final approval
Onur C. Kutlu, MD: data analysis/interpretation, revision of article, final approval
Beth Herrick, MD: conception/design of the work, revision of article, final approval
Claudius Conrad, MD, PhD: conception/design of the work, supervision/leadership, data analysis/interpretation, revision of article, final approval
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous Presentation Acceptance: SSAT DDW (Society for Surgery of the Alimentary Tract: Digestive Disease Week) 2021, SSAT Quick Shot Session: Hepatobiliary & Pancreas I; May 21-23, 2021.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Salehi, O., Vega, E.A., Lathan, C. et al. Race, Age, Gender, and Insurance Status: A Comparative Analysis of Access to and Quality of Gastrointestinal Cancer Care. J Gastrointest Surg 25, 2152–2162 (2021). https://doi.org/10.1007/s11605-021-05038-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05038-6