Abstract
Background
The objective of this study was to analyze whether primary tumor resection (PTR) among patients with stage IV gastrointestinal neuroendocrine tumor (GI-NET) and unresected metastases was associated with improved outcomes.
Methods
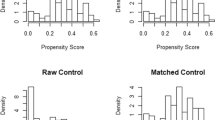
Patients diagnosed with stage IV GI-NETs were identified in the linked SEER-Medicare database from 2004 to 2015. Overall survival (OS) of patients who did versus did not undergo PTR was examined using bivariate and multivariable cox regression analysis as well as propensity score matching (PSM).
Results
Among 2219 patients with metastatic GI-NETs, 632 (28.5%) underwent PTR, whereas 1587 (71.5%) did not. The majority of individuals had a NET in the pancreas (n = 969, 43.6%); the most common site of metastatic disease was the liver (n = 1064, 47.9%). Patients with stage IV small intestinal NETs most frequently underwent PTR (62.6%) followed by individuals with colon NETs (56.5%). After adjusting for all competing factors, PTR remained independently associated with improved OS (HR = 0.65, 95% CI: 0.56–0.76). Following PSM (n = 236 per group), patients who underwent PTR had improved OS (median OS: 1.3 years vs 0.8 years, p = 0.016). While PTR of NETs originating from stomach, small intestine, colon, and pancreas was associated with improved OS, PTR of rectal NET did not yield a survival benefit.
Conclusion
Primary GI-NET resection was associated with a survival benefit among individuals presenting with metastatic GI-NET with unresected metastases. Resection of primary GI-NET among patients with stage IV disease and unresected metastases should only be performed in selected cases following multi-disciplinary evaluation.



Similar content being viewed by others
References
Moris D, Ntanasis-Stathopoulos I, Tsilimigras DI, et al. Update on Surgical Management of Small Bowel Neuroendocrine Tumors. Anticancer Res 2018; 38(3):1267-1278.
Moris D, Tsilimigras DI, Vagios S, et al. Neuroendocrine Neoplasms of the Appendix: A Review of the Literature. Anticancer Res 2018; 38(2):601-611.
Tierney JF, Chivukula SV, Wang X, et al. Resection of primary tumor may prolong survival in metastatic gastroenteropancreatic neuroendocrine tumors. Surgery 2019; 165(3):644-651.
Tsilimigras DI, Ntanasis-Stathopoulos I, Kostakis ID, et al. Is Resection of Primary Midgut Neuroendocrine Tumors in Patients with Unresectable Metastatic Liver Disease Justified? A Systematic Review and Meta-Analysis. J Gastrointest Surg 2019; 23(5):1044-1054.
Gangi A, Manguso N, Gong J, et al. Midgut Neuroendocrine Tumors with Liver-only Metastases: Benefit of Primary Tumor Resection. Ann Surg Oncol 2020; 27(11):4525-4532.
Delle Fave G, O'Toole D, Sundin A, et al. ENETS Consensus Guidelines Update for Gastroduodenal Neuroendocrine Neoplasms. Neuroendocrinology 2016; 103(2):119-24.
Niederle B, Pape UF, Costa F, et al. ENETS Consensus Guidelines Update for Neuroendocrine Neoplasms of the Jejunum and Ileum. Neuroendocrinology 2016; 103(2):125-38.
O'Toole D, Kianmanesh R, Caplin M. ENETS 2016 Consensus Guidelines for the Management of Patients with Digestive Neuroendocrine Tumors: An Update. Neuroendocrinology 2016; 103(2):117-8.
Howe JR, Cardona K, Fraker DL, et al. The Surgical Management of Small Bowel Neuroendocrine Tumors: Consensus Guidelines of the North American Neuroendocrine Tumor Society. Pancreas 2017; 46(6):715-731.
Hellman P, Lundstrom T, Ohrvall U, et al. Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastases. World J Surg 2002; 26(8):991-7.
Givi B, Pommier SJ, Thompson AK, et al. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery 2006; 140(6):891-7; discussion 897-8.
Strosberg J, Gardner N, Kvols L. Survival and prognostic factor analysis of 146 metastatic neuroendocrine tumors of the mid-gut. Neuroendocrinology 2009; 89(4):471-6.
Norlen O, Stalberg P, Oberg K, et al. Long-term results of surgery for small intestinal neuroendocrine tumors at a tertiary referral center. World J Surg 2012; 36(6):1419-31.
Ahmed A, Turner G, King B, et al. Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocr Relat Cancer 2009; 16(3):885-94.
Soreide O, Berstad T, Bakka A, et al. Surgical treatment as a principle in patients with advanced abdominal carcinoid tumors. Surgery 1992; 111(1):48-54.
Lewis A, Raoof M, Ituarte PHG, et al. Resection of the Primary Gastrointestinal Neuroendocrine Tumor Improves Survival With or Without Liver Treatment. Ann Surg 2019; 270(6):1131-1137.
Hyder O, Dodson RM, Nathan H, et al. Referral patterns and treatment choices for patients with hepatocellular carcinoma: a United States population-based study. J Am Coll Surg 2013; 217(5):896-906.
Ejaz A, Reames BN, Maithel S, et al. Cytoreductive debulking surgery among patients with neuroendocrine liver metastasis: a multi-institutional analysis. HPB (Oxford) 2018; 20(3):277-284.
Tsilimigras DI, Squires MH, Cloyd JM, et al. Treatment strategies for neuroendocrine liver metastases: an update. Expert Opinion on Orphan Drugs 2019; 7(7-8):327-335.
Davar J, Connolly HM, Caplin ME, et al. Diagnosing and Managing Carcinoid Heart Disease in Patients With Neuroendocrine Tumors: An Expert Statement. J Am Coll Cardiol 2017; 69(10):1288-1304.
Daskalakis K, Karakatsanis A, Stalberg P, et al. Clinical signs of fibrosis in small intestinal neuroendocrine tumours. Br J Surg 2017; 104(1):69-75.
Chambers AJ, Pasieka JL, Dixon E, et al. The palliative benefit of aggressive surgical intervention for both hepatic and mesenteric metastases from neuroendocrine tumors. Surgery 2008; 144(4):645-51; discussion 651-3.
Zhou B, Zhan C, Ding Y, et al. Role of palliative resection of the primary pancreatic neuroendocrine tumor in patients with unresectable metastatic liver disease: a systematic review and meta-analysis. Onco Targets Ther 2018; 11:975-982.
Biondi-Zoccai G, Romagnoli E, Agostoni P, et al. Are propensity scores really superior to standard multivariable analysis? Contemp Clin Trials 2011; 32(5):731-40.
Huttner FJ, Schneider L, Tarantino I, et al. Palliative resection of the primary tumor in 442 metastasized neuroendocrine tumors of the pancreas: a population-based, propensity score-matched survival analysis. Langenbecks Arch Surg 2015; 400(6):715-23.
Smith JK, Ng SC, Hill JS, et al. Complications after pancreatectomy for neuroendocrine tumors: a national study. J Surg Res 2010; 163(1):63-8.
Polcz M, Schlegel C, Edwards GC, et al. Primary Tumor Resection Offers Survival Benefit in Patients with Metastatic Midgut Neuroendocrine Tumors. Ann Surg Oncol 2020; 27(8):2795-2803.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was accepted as an Oral Presentation at the International Hepato-Pancreato-Biliary Association (IHPBA) 14th Annual Meeting, February 2021, Melbourne, Australia
Supplementary Information
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Tsilimigras, D.I., Hyer, J.M., Paredes, A.Z. et al. Resection of Primary Gastrointestinal Neuroendocrine Tumor Among Patients with Non-Resected Metastases Is Associated with Improved Survival: A SEER-Medicare Analysis. J Gastrointest Surg 25, 2368–2376 (2021). https://doi.org/10.1007/s11605-020-04898-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04898-8