Abstract
Background
The National Comprehensive Cancer Network has defined metrics for colorectal cancer; however, the association of metric adherence with patient clinical outcomes remains underexplored. The study aim was to evaluate the association of National Comprehensive Cancer Network metric adherence with recurrence and mortality in Veterans with nonmetastatic colorectal cancer.
Methods
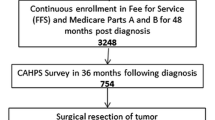
Veterans with stage I–III colorectal cancer who underwent non-emergent resection from 2001 to 2015 at a single Veterans Affairs Medical Center were included. The primary predictor was completion of eligible National Comprehensive Cancer Network metrics. The primary outcome was a composite of recurrence or all-cause death in three phases of care: surgical (up to 6 months after resection), treatment (6–18 months after resection), and surveillance (18 months–3 years after resection). Hazard ratios were estimated via Cox proportional hazards regression in a propensity score–weighted cohort.
Results
A total of 1107 electronic medical records of patients undergoing colorectal surgery were reviewed, and 379 patients were included (301 colon and 78 rectal cancer). In the surgical phase, the weighted analysis yielded a hazard ratio of 0.37 (95% confidence interval 0.12–1.13) for metric-adherent patients compared with non-adherent patients. In the treatment and surveillance phases, the hazard ratios for metric-adherent care were 0.68 (95% confidence interval 0.25–1.85) and 0.91 (95% confidence interval 0.31–2.68), respectively.
Conclusions
The National Comprehensive Cancer Network guideline metric adherence was associated with a lower rate of recurrence and death in the surgical phase of care among stage I–III patients with resected colorectal cancer.


Similar content being viewed by others
References
National Cancer Institute. SEER Cancer Statistics Review. 2019. https://seer.cancer.gov/statfacts/html/colorect.html. Accessed 11 Feb 2020.
Zullig LL, Smith VA, Jackson GL, et al. Colorectal Cancer Statistics from the Veterans Affairs Central Cancer Registry. Clinical Colorectal Cancer. 2016: 15 (4): e199–204.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Colon Cancer. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed 11 Feb 2020.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Rectal Cancer. https://www.nccn.org/professionals/physician_gls/pdf/rectal_blocks.pdf. Accessed 11 Feb 2020.
Chao HH, Schwartz AR, Hersh J, et al. Improving colorectal cancer screening and care in the Veterans Affairs Healthcare system. Clin Colorectal Cancer. 2009;8(1):22-28.
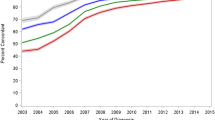
Snyder RA, Mainthia R, Patel R, Dittus RS, Roumie CL. Quality of colorectal cancer care among veterans: a 10-year retrospective cohort. Ann Surg Oncol. 2014;21(8):2476-2483.
Jackson GL, Melton LD, Abbott DH, et al. Quality of nonmetastatic colorectal cancer care in the Department of Veterans Affairs. J Clin Oncol. 2010;28(19):3176-3181.
Boland GM, Chang GJ, Haynes AB, et al. Association between adherence to National Comprehensive Cancer Network treatment guidelines and improved survival in patients with colon cancer. Cancer. 2013;119(8):1593-1601.
Malin JL, Schneider EC, Epstein AM, Adams J, Emanuel EJ, Kahn KL. Results of the National Initiative for Cancer Care Quality: how can we improve the quality of cancer care in the United States? J Clin Oncol. 2006;24(4):626-634.
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351(17):1731-1740.
André T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27(19):3109-3116.
PA Harris, R Taylor, R Thielke, J Payne, N Gonzalez, JG Conde. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr; 42(2):377-81.
Benson AB 3rd, Schrag D, Somerfield MR, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408-3419.
Johansen C, Schou G, Soll-Johanning H, Mellemgaard A, Lynge E. Influence of marital status on survival from colon and rectal cancer in Denmark. Br J Cancer. 1996; 74:985–988.
Wang L, Wilson SE, Stewart DB, Hollenbeak CS. Marital status and colon cancer outcomes in US Surveillance, Epidemiology and End Results registries: does marriage affect cancer survival by gender and stage? Cancer epidemiology. 2011; 35:417–422.
Pisarska M, Torbicz G, Gajewska N, et al. Compliance with the ERAS Protocol and 3-Year Survival After Laparoscopic Surgery for Non-metastatic Colorectal Cancer. World J Surg. 2019;43(10):2552-2560
Li L, Greene T. A weighting analogue to pair matching in propensity score analysis. The International Journal of Biostatistics, 2013; 9(2), 215–234.
R Core Team (2019). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
Jackson GL, Zullig LL, Zafar SY, et al. Using NCCN clinical practice guidelines in oncology to measure the quality of colorectal cancer care in the Veterans health administration. J Natl Compr Canc Netw. 2013;11(4):431-441.
Romanus D, Weiser MR, Skibber JM, et al. Concordance with NCCN Colorectal Cancer Guidelines and ASCO/NCCN Quality Measures: an NCCN institutional analysis. J Natl Compr Canc Netw. 2009;7(8):895-904.
Mason MC, Chang GJ, Petersen LA, et al. National Quality Forum Colon Cancer Quality Metric Performance: How Are Hospitals Measuring Up? Ann Surg. 2017;266(6):1013-1020.
National Quality Forum. Endorsement Summary: Cancer Measures. http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Additional_Cancer_Measures.aspx. Accessed 11 Feb 2020.
Hines RB, Barrett A, Twumasi-Ankrah P, et al. Predictors of guideline treatment nonadherence and the impact on survival in patients with colorectal cancer. J Natl Compr Canc Netw. 2015;13(1):51-60.
Le Voyer TE, Sigurdson ER, Hanlon AL, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003;21(15):2912-2919.
Wells KO, Hawkins AT, Krishnamurthy DM, et al. Omission of Adjuvant Chemotherapy Is Associated With Increased Mortality in Patients With T3N0 Colon Cancer With Inadequate Lymph Node Harvest. Dis Colon rectum. 2017;60(1):15-21.
Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009;373(9666):821-828.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26(2):303-312.
Kitz J, Fokas E, Beissbarth T, et al. Association of Plane of Total Mesorectal Excision With Prognosis of Rectal Cancer: Secondary Analysis of the CAO/ARO/AIO-04 Phase 3 Randomized Clinical Trial. JAMA Surg. 2018;153(8):e181607.
Hill SS, Chung SK, Meyer DC, et al. Impact of Preoperative Care for Rectal Adenocarcinoma on Pathologic Specimen Quality and Postoperative Morbidity: A NSQIP Analysis. J Am Coll Surg. October 2019. doi:https://doi.org/10.1016/j.jamcollsurg.2019.09.004
Primrose JN, Perera R, Gray A, et al. Effect of 3 to 5 years of scheduled CEA and CT follow-up to detect recurrence of colorectal cancer: the FACS randomized clinical trial. JAMA. 2014;311(3):263-270.
Rosati G, Ambrosini G, Barni S, et al. A randomized trial of intensive versus minimal surveillance of patients with resected Dukes B2-C colorectal carcinoma. Ann Oncol. 2016;27(2):274-280.
Snyder RA, Hu C-Y, Cuddy A, et al. Association Between Intensity of Posttreatment Surveillance Testing and Detection of Recurrence in Patients With Colorectal Cancer. JAMA. 2018;319(20):2104-2115.
Acknowledgments
The authors would like to thank Jennifer Wharton, BS, for her contributions to IRB preparation. This work was supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars Program, and with the use of facilities at VA Tennessee Valley Healthcare System, Nashville, TN.
Funding
Dr. Edwards is supported by the Office of Academic Affiliations, Department of Veterans Affairs (VA) National Quality Scholars Program.
Author information
Authors and Affiliations
Contributions
Study conception and design: Edwards, Martin, Wyman, Snyder, Bailey, Roumie
Acquisition of data: Edwards, Martin, Snyder
Analysis and interpretation of data: Edwards, Samuels, Roumie
Drafting of the manuscript: Edwards, Samuels, Roumie
Critical revision of the manuscript: Edwards, Martin, Samuels, Wyman, Bailey, Kiernan, Snyder, Dittus, Roumie
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 442 kb)
Rights and permissions
About this article
Cite this article
Edwards, G.C., Martin, R.L., Samuels, L.R. et al. Association of Adherence to Quality Metrics with Recurrence or Mortality among Veterans with Colorectal Cancer. J Gastrointest Surg 25, 2055–2064 (2021). https://doi.org/10.1007/s11605-020-04804-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04804-2