Abstract
Background
The prognostic value of sarcopenic obesity in gastric cancer surgery remains debated. We aimed to evaluate the impact on outcomes of body composition and sarcopenic obesity after gastrectomy for gastric cancer.
Methods
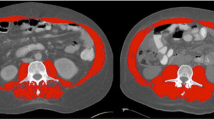
A retrospective review of prospectively maintained database of patients undergoing gastrectomy for gastric cancer from 2010 to 2017 was performed. Skeletal muscle mass and visceral adipose tissue were evaluated by preoperative computed tomography to define sarcopenia and obesity. Patients were classified in body composition groups according to the presence or absence of sarcopenia and obesity. Prognostic factors for survival were assessed by multivariate Cox analysis.
Results
Of the 198 patients undergoing gastrectomy for gastric cancer, 90 (45.4%) patients were sarcopenic, 130 (67.7%) obese, and in the subclassification for body composition categories: 33 (17%) nonsarcopenic nonobesity, 75 (38%) non sarcopenic obesity, 35 (17%) sarcopenic nonobesity, and 55 (28%) sarcopenic obesity. No category of body composition was a predictor of postoperative complications and worse overall and disease-free survival outcomes. Multivariable analysis identified ASA III classification, preoperative weight loss > 10%, postoperative surgical re-intervention, and advanced tumor stage as independent prognostic factors for overall survival, and patients aged 75 years or older, preoperative weight loss > 10%, elevated netrophil-lymphocyte ratio, and advanced tumor stage as independent prognostic factors for disease-free survival.
Conclusions
Sarcopenia, obesity, and sarcopenic obesity were not associated with worse outcomes after gastric cancer surgery.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer Journal for Clinicians 2018; 68: 394-424.
Dycken B, Bigam D, Cass C, Mackey J, Joy A, Hamilton S. Gastric Adenocarcinoma: Review and considerations for future directions. Annals of Surgery 2005; 241: 27-39.
Macdonald J. Gastric Cancer: Nagoya Is Not New York. Journal of Clinical Oncology 2011; 29: 33: 4348-50.
Russo A, Li P, Strong V. Differences in the multimodal treatment of gastric cancer: East versus west. Journal of Surgical Oncology. 2017;115:603-614.
Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric Cancer: ESMO-ESSO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2013 Oct;24Suppl6:vi57-63.
Tu RH, Lin JX, Li P, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M, Zheng CH, Huang CM. Comprehensive Complication Index Predicts Cancer-Specific Survival of Patients with Postoperative Complications after Curative Resection of Gastric Cancer. Gastroenterology research and practice. 2018; 2018:4396018.
Bartlett EK, Roses RE, Kelz RR, Drebin JA, Fraker DL, Karakousis GC. Morbidity and mortality after total gastrectomy for gastric malignancy using the American College of Surgeons National Surgical Quality Improvement Program database. Surgery. 2014;156:298-304.
Claassen YHM, Hartgrink HH, Dikken JL, de Steur WO, van Sandick JW, van Grieken NCT, Cats A, Trip AK, Jansen EPM, Meershock-Klein Kranenbearg WM, Braak JPBM, Putter H, van Berge Henegouwen MI, Verhij M, van de Velde CJH. Surgical morbidity and mortality after neoadjuvant chemotherapy in the CRITICS gastric cancer trial. European Journal of Surgical Oncology. 2018;44:613-619.
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass HO, Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. The American Journal of Medicine 1980; 69: 491-497
Mariette C, De Botton ML, Piessen G. Surgery in esophageal and gastric cancer patients: what is the role for nutrition support in your daily practice? Annals of Surgical Oncology 2012; 19: 2128-2134.
Yang Z, Zhou X, Ma B, Xing Y, Jiang X, Wang Z. Predictive value of preoperative sarcopenia in patients with gastric cancer: a meta-analysis and systematic review. Journal of Gatrointestinal Surgery 2018;22:1890-1902.
Sierzega M, Chrzan R, Wiktorowicz M, Kobdziejczyk P, Richter P. Prognostic and predictive implications of sarcopenia in Western patients undergoing gastric resections for carcinoma of the stomach. Journal of Surgical Oncology 2019;1-10.
Zhuang CL, Huang DD, Pang WY, Zhou CJ, Wang SL, Lou N, Ma LL, Yu Z, Shen X. Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: Analysis from a large-scale cohort. Medicine (Baltimore) 2016; 95:e3164.
Bickenbach KA, Denton B, Gonen M, Brennan MF, Coit DG, Strong VE. Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer. Annals of Surgical Oncology 2013;20:780-7.
Takeuchi M, Ishii K, Seki H, Yasui N, Sakata M, Shimada A, Matsumoto H. Excessive visceral fat area as a risk factor for early postoperative complications of total gastrectomy for gastric cancer: a retrospective cohort study. BMS Surgery. 2016;16(1): 54.
Zhang y, Wang JP, Wang XL, Tian H, Gao TT, Tang LM, Tian F, Wang JW, Zheng HJ, Zhang L, Gao XJ, Li GL, Wang XY. Computed tomography-quantified body composition predicts short-term outcomes after gastrectomy in gastric cancer. Current Oncology 2018; 25(5): e411-e422.
Okumura S, Kaido N, Hamaguchi Y, Shirai H, Yao S, Yagi S, Kamo N, Hatano E, Okajima H, Takaori K, Uemoto S. Visceral adiposity and sarcopenic visceral obesity are associated with poor prognostic after resection of pancreatic cancer. Annals of Surgical Oncology 2017;24(12):3732-3740.
Kocher NJ, Jafri S, Balabhadra S, Lehman E, Gardner J, Vijay K, Sarwani N, Raman JD. Is sarcopenia and sarcopenic obesity associated with clinical and pathological outcomes in patients undergoing radical nephroureterectomy?. Urologic Oncology 2018;36(4):156.e17-156.e22.
Kobayashi A, Kaido T, Hamaguchi Y, Okumura S, Shirai H, Yao S, Kamo N, Yagi S, Taura K, Okajima H, Uemoto S. Impact of sarcopenic obesity on outcomes in patients undergoing hepatectomy for hepatocellular carcinoma. Annals of Surgery. 2019; 269(5):924-931.
Zhang W, Lin J, Chen WS, Huang YS, Wu RS, Chen XD, Lou N, Chi CH, Hu CY, Shen X. Sarcopenic obesity is associated with severe postoperative complications in gastric cancer patients undergoing gastrectomy: a prospective study. Journal of Gastrointestinal Surgery 2018; 22(11):1861-1869.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery 2004;240(2):205-13.
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D, ESMO Guidelines Committee. Gastric Cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2016;27(suppl 5): v38-v49.
Allum W, Lordick F, Alsina M, Andritsch E, Ba-Ssalamah A, Beishon M, Braga M, Caballero C, Carneiro F, Cassinello F, Dekker JW, Delgado-Bolton R, Haustermans K, Henning G, Hutter B, Lovey J, Netikova IS, Obermannová R, Obert S, Rostoft S, Saarto T, Seufferlein T, Sheth S, Wynter-Blyth V, Costa A, Naredi P. ECCO essential requirements for quality cancer care: Oesophageal and gastric cancer. Critical Reviews in Oncology/Hematology 2018; 122:179-193.
Ajani JA, Lee J, Sano T, Janjigian YY, Fan D, Song S. Gastric Adenocarcinoma. Nature Reviews Disease Primers. 2017; 3:17036.
Prado CMM, Lieff JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of repiratory and gastrointestinal tracts: a population based study. The Lancet Oncology. 2008; 9:639-635.
Doyle SL, Bennet AM, Donohoe CL, Mongan AM, Howard JM, Lithander FE, Pidgeon GP, Reynolds JV, Lysaght J. Establishing computed tomography-defined visceral fat area thresholds for use in obesity-related cancer research. Nutrition Research. 2013;33(3):171-179.
Reisinger KW, Bosmans JW, Uittenbogaart M, Alsoumali A, Poeze M, Sosef MN, Derikx JP. Loss of skeletal muscle mass during neoadjuvant chemoradiotherapy predicts postoperative mortality in esophageal cancer surgery. Annals of Surgical Oncology. 2015; 22(13): 4445-4452.
Snijder MB, van Dam RM, Visser M, Seidell JC. What aspects of body fat are particularly hazardous and how do we measure them?. International Journal of Epidemiology. 2006; 35(1): 83-92.
Tegels JJ, van Vugt JL, Reisinger KW, Hulsewé KW, Hoofwijk AG, Derikx JP, Stoot JH. Sarcopenia is highly prevalent in patients undergoing surgery for gastric cancer but not associated with worse outcomes. Journal of Surgical Oncology. 2015;112(4):403-407.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. Journal of Clinical Oncology. 2013; 31: 1539-1547.
Wang SL, Ma LL, Chen XY, Zhou DL, Li B, Huang DD, Yu Z, Shen X, Zhuang CL. Impact of visceral fat on surgical complications and long-term survival of patients with gastric cancer after radical gastrectomy. European Journal of Clinical Nutrition. 2018;72:436-445.
Gruber ES, Jomrich G, Tamandi D, Gnant M, Schindl M, Sahora K.Sarcopenia and sarcopenic obesity are independent adverse prognostic factors in resectable ductal adenocarcinoma. PLoSONE. 2019; 14(5): e0215915.
Lodewick TM, van Nijnatten TJ, van Dam RM, van Mierlo K, Dello SA, Neumann UP, Olde Damink SW, Dejong CH. Are sarcopenia, obesity and sarcopenic obesity predictive of outcome in patients with colorectal liver metastases?. HPB (Oxford). 2015;17(5):438-446.
Nishigori T, Tsunoda S, Okobe H, Tanaka E, Hisamori S, Hosogi H, Shinohara H, Sakai Y. Impact of sarcopenic obesity on surgical site infection after laparoscopic total gastrectomy. Annals of Surgical Oncology. 2016;23 (suppl 4): 524-531.
Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, Heymsfield SB, Heshka S. Total body skeletal muscle and adipose tissue volume: estimation form a single abdominal cross-sectional image. Journal of Applied Physiology 1985. 2004; 97(6): 2333-8.
Hopkins JJ, Skubleny D, Bigam DL, Baracos VE, Eurich DT, Sawyer MB. Barriers to the interpretation of body composition in colorectal cancer: A review of the methodological inconsistency and complexity of the CT-defined body habitus. Annals of Surgical Oncology. 2018 25(5): 1381-1394.
Carneiro IP, Mazurak VC, Prado CM. Clinical implications of sarcopenic obesity in cancer. Current Oncology Reports. 2016; 18(10): 62.
Ramos MFKP, Pereira MA, Dias AR, Yagi OK, Zaidan EP, Ribeiro-Junior U, Zilberstein B, Cecconello I. Surgical outcomes of gastrectomy with D1 lymph node dissection performed for patients with unfavorable clinical conditions. European Journal of Surgical Oncology. 2019; 45(3): 460-465.
Rausei S, Ruspi L, Rosa F, Morgagni P, Marrelli D, Cossu A, Cananzi FC, Lomonaco R, Coniglio A, Biondi A, Cipollari C, Graziosi L, Fumagalli U, Casella F, Bertoli P, di Leo A, Alfieri S, Vittimberga G, Roviello F, Orsenigo E, Quagliuolo V, Montemurro S, Baiocchi G, Persiani R, Bencivenga M, Donini A, Rosati R, Sansonetti A, Ansaloni L, Zanoni A, Galli F, Dionigi G, Italian Research Group for Gastric Cancer (IRGGC). Extended lymphadenectomy in elderly and/or highly comorbid gastric cancer patients: a retrospective multicenter study. European Journal of Surgical Oncology. 2016; 42(12): 1881-1889.
Verlato G, Marrelli D, Accordini S, Bencivenga M, Di Leo A, Marchet A, Petrioli R, Zoppini G, Muggeo M, Roviello F, de Manzoni G. Short-term and long-term risk factors in gastric cancer. World Journal of Gastroenterology. 2015 7;21(21): 6434-43.
Wu XJ, Miao RL, Li ZY, Bu ZD, Zhang LH, Wu AW, Zong XL, Li SX, Shan F, Ji X, Ren H, Ji JF. Prognostic value of metastatic lymph node ratio as an additional tool to the TNM stage system in gastric cancer. European Journal of Surgical Oncology. 2015; 41(7): 927-33.
Liu X, Qiu H, Liu J, Chen S, Xu D, Li W, Zhan Y, Li Y, Chen Y, Zhou Z, Sun X. A novel prognostic score, based on preoperative nutritional status, predicts outcomes of patients after curative resection for gastric cancer. Journal of Cancer. 2016; 7(14): 2148-2156.
Zheng HL, Lu J, Li P, Xie JW, Wang JB, Lin JX, Chen QY, Cao LL, Lin M, Tu R, Huang CM, Zheng CH. Effects of preoperative malnutrition on short and long-term outcomes of patients with gastric cancer: can we do better?. Annals of Surgical Oncology. 2017; 24:3376.
Liu X, Qiu H, Kong P, Zhou Z, Sun X. Gastric cancer, nutritional status and outcome. OncoTargets and therapy. 2017; 10:2107-2114.
Djaladat H, Bruns HM, Miranda G, Cai J, Skinner EC, Daneshmand S. The association of preoperative serum albumin level and American Society of Anesthesiologists (ASA) score on early complications and survival of patients undergoing radical cystectomy for urothelial bladder cancer. BJU International. 2014; 113(6): 887-93.
Wang S, Xu L, Wang Q, Li J, Bai B, Li Z, Wu X, Yu P, Li X, Yin J. Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World Journal of Surgical Oncology. 2019; 17(1): 52.
Jin LX, Sanford DE, Squires MH 3rd, Moses LE, Yan Y, Poultsides GA, Votanopoulos KI, Weber SM, Bloomston M, Pawlik TM, Hawkins WG, Linehan DC, Schmidt C, Worhunsky DJ, Acher AW, Cardona K, Cho CS, Kooby DA, Levine EA, Winslow E, Saunders N, Spolverato G, Colditz GA, Maithel SK, Fields RC. Interaction of postoperative morbidity and receipt of adjuvant therapy on long-term survival after resection for gastric adenocarcinoma: results from the U.S. Gastric Cancer Collaborative. Annals of Surgical Oncology. 2016;23: 2398-408.
Qu JL, Qu XJ, Li X, Zhang JD, Teng YE, Jin B, Zhao MF, Yu P, Liu DY, Liu YP. Early initiation of fluorouracil-based adjuvant chemotherapy improves survival in patients with resectable gastric cancer. Journal of BUON. 2015; 20:800-7.
O`Leary DP, Wang JH, Cotter TG, Redmond HP. Less stress, more success? Oncological implications of surgery-induced oxidative stress. Gut. 2013; 62:461-70.
Miyamoto R, Inagawa S, Sano N, Tadano S, Adachi S, Yamamoto M. The neutrophil-to-lymphocyte ratio (NLR) predicts short-term and long-term outcomes in gastric cancer patients. European Journal of Surgical Oncology. 2018; 44(5): 607-612.
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007; 73:215-20.
Shimada H, Takiguchi N, Kainuma O, Soda H, Ikeda A, Cho A, Mayazaki A, Gunji H, Yamamoto H, Nagata M. High preoperative neutrophil-lymphocyte ratio predicts por survival in patients with gastric cáncer. Gastric Cancer. 2010; 13:170-6.
Jung MR, Park YK, Jeong O, Seon JW, Ryu SY, Kim DY, Kim YJ. Elevated preoperative neutrophil to lymphocyte ratio predicts poor survival following resection in late stage gastric cancer. Journal of Surgical Oncology. 2011; 104:504-10.
Author information
Authors and Affiliations
Contributions
V. Rodrigues made substantial contributions to the conception or design of the work, the acquisition, analysis and interpretation of data for the work.
F. Landi made substantial contributions to the acquisition of data and made drafting the work and revising it critically for important intellectual content.
R. Mast made substancial contributions to the acquisition of data for the work.
S. Castro and N. Rodríguez made agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
J. Pradell, A. Gantxegi, and M. López-Cano made drafting the work and revising it critically for important intellectual content.
M. Armengol made the final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodrigues, V., Landi, F., Castro, S. et al. Is Sarcopenic Obesity an Indicator of Poor Prognosis in Gastric Cancer Surgery? A Cohort Study in a Western Population. J Gastrointest Surg 25, 1388–1403 (2021). https://doi.org/10.1007/s11605-020-04716-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04716-1