Abstract
Background
Emergency laparotomy for small bowel pathologies comprises a significant number of all emergency surgeries. Application of evidence-based adapted enhanced recovery after surgery (ERAS) protocol can potentially improve the perioperative outcome in these procedures.
Aims
To determine the feasibility, safety, and efficacy of adapted ERAS pathway in emergency small bowel surgery.
Methodology
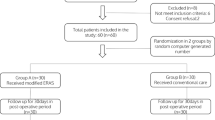
This was a single-center, prospective, open-labeled, superiority, randomized controlled trial. Patients suspected to have small bowel pathology by the emergency surgical team were randomized preoperatively into standard care and adapted ERAS group. Patients with American Society of Anesthesiologist class ≥ 3, polytrauma patients with associated other intra-abdominal organ injuries, duodenal ulcer perforations, patients presenting with refractory shock, and pregnant patients were excluded. Primary outcome parameter was the length of hospitalization (LOH). Morbidity and other functional recovery parameters were also assessed.
Results
Thirty-five patients were included in the adapted ERAS and standard care group. The laboratory and demographic variables were comparable. Patients in the ERAS group had significantly earlier recovery (days) in terms of first fluid diet (1.48 ± 0.18, p < 0.001), solid diet (2.11 ± 0.17, p < 0.001), time to first flatus (1.25 ± 0.24, p < 0.001), and first stool (1.8 ± 0.27, p < 0.001). Postoperative nausea, vomiting (RR 0.69, p = 0.19), pulmonary complications (RR 0.38, p = 0.16), superficial (RR 0.79, p = 0.33), and deep surgical site infections (RR 0.65, p = 0.39) were similar. Compared with the standard care group, ERAS group had significantly shorter LOH (8 ± 0.38 vs. 10.83 ± 0.42; Mean difference, 2.83 ± 0.56; p < 0.001).
Conclusion
Adapted ERAS pathways are feasible, safe, and significantly reduces the LOH in select patients undergoing emergency small bowel surgery.


Similar content being viewed by others
References
Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008; 248: 189–98.
Snchez-Jimnez R, Blanco A, Trebol Lpez J, Snchez A, Gutirrez F, Carmona Sez JA. ERAS (Enhanced Recovery after Surgery) in Colorectal Surgery. In: Khan J, editor. Colorectal Cancer - Surgery, Diagnostics and Treatment. First Ed. InTech; 2014; 487-503
Nelson G, Altman AD, Nick A, Meyer LA, Ramirez PT, Achtari C, et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations--Part I. Gynecol Oncol. 2016; 140:313–22.
White JJE, Houghton-Clemmey R, Marval P. Enhanced recovery after surgery (ERAS): an orthopaedic perspective. J Perioper Pract. 2013;23 :228–32.
Cerantola Y, Valerio M, Persson B, Jichlinski P, Ljungqvist O, Hubner M, et al. Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS (®)) society recommendations. Clin Nutr Edinb Scotl. 2013; 32:879–87.
Gotlib Conn L, Rotstein OD, Greco E, Tricco AC, Perrier L, Soobiah C, et al. Enhanced recovery after vascular surgery: protocol for a systematic review. Syst Rev. 2012; 1:52.
Padilla Alarcón J, Peñalver Cuesta JC. Experience with lung resection in a fast-track surgery program. Arch Bronconeumol. 2013; 49:89–93.
Batdorf NJ, Lemaine V, Lovely JK, Ballman KV, Goede WJ, Martinez-Jorge J, et al. Enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthetic Surg. 2015; 68:395–402.
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014; 38:1531–41.
Dorcaratto D, Grande L, Pera M. Enhanced recovery in gastrointestinal surgery: upper gastrointestinal surgery. Dig Surg. 2013; 30:70–8.
Varadhan KK, Neal KR, Dejong CHC, Fearon KCH, Ljungqvist O, Lobo DN. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr Edinb Scotl. 2010; 29:434–40.
Gouvas N, Tan E, Windsor A, Xynos E, Tekkis PP. Fast-track vs standard care in colorectal surgery: a meta-analysis update. Int J Colorectal Dis. 2009; 24:1119–31.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival After Emergency General Surgery: What can We Learn from Enhanced Recovery Programmes? World J Surg 2016; 40:1283–7.
Lyon A, Payne CJ, Mackay GJ. Enhanced recovery programme in colorectal surgery: does one size fit all? World J Gastroenterol. 2012 28; 18:5661–3.
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, et al. Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg. 2014; 207:807–14.
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V. Adapted ERAS Pathway vs. Standard Care in Patients with Perforated Duodenal Ulcer-a Randomized Controlled Trial. J Gastrointest Surg. 2018; 22:107–16.
Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M. Enhanced recovery pathway for urgent colectomy. World J Surg. 2014; 38:2153–9.
Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol. 2014; 20:13950–5.
Low J, Johnson N, Morris C. Epidural analgesia: first do no harm. Anaesthesia.2008;63:1-3.
Pragatheeswarane M, Muthukumaraswamy R, Kadambari D, Kate V. Early oral feeding vs. traditional feeding in patients undergoing elective open bowel surgery-a randomized controlled trial. J Gastrointest Surg. 2014; 18:1017-23
Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932; 22:55.
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al. The Clavien-Dindo classification of surgical complications: five-year experience. Am J Surg. 2009; 250:187-9.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017 Aug 1;152(8):784–91.
Yamada T, Hayashi T, Cho H, Yoshikawa T, Taniguchi H, Fukushima R, et al. Usefulness of enhanced recovery after surgery protocol as compared with conventional postoperative care in gastric surgery. Gastr Can. 2012; 15:34-41.
Chen Hu J, Xin Jiang L, Cai L, Tao Zheng H, Yuan Hu S, Bing Chen H, et al. Preliminary experience of fast-track surgery combined with laparoscopy-assisted radical distal gastrectomy for gastric cancer. J Gastrointest Surg. 2012; 16:1830-9.
Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007.CD004929.
Spanjersberg WR, Readings J, Keus F, van Laarhoven CJ. Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst. Rev. 2011; CD007635.
Stoot JH, van Dam RM, Busch OR, van Hillegersberg R, De Boer M, Olde Damink SWM, et al. The effect of a multimodal fast-track programme on outcomes in laparoscopic liver surgery: a multicentre pilot study. HPB. 2009; 11:140–4.
Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg . 2013; 17:962–72.
Nygren J, Thacker J, Carli F, Fearon KCH, Norderval S, Lobo DN, et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr Edinb Scotl. 2012; 31:801–16
Wisely JC, Barclay KL. Effects of an enhanced recovery after surgery programme on emergency surgical patients. ANZ J Surg. 2016. DOI:https://doi.org/10.1111/ans.13465.
Zaouter C, Kaneva P, Carli F. Less urinary tract infection by earlier removal of bladder catheter in surgical patients receiving thoracic epidural analgesia. Reg Anesth Pain Med. 2009; 34:542–8.
Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, Morgenstein-Wagner TB, et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg. 1992; 216:172–83.
Egbert LD, Battit GE, Welch CE, Bartlett MK. Reduction of postoperative pain by encouragement and instruction of patients. a study of doctor-patient rapport. N Engl J Med. 1964; 270:825–7.
Hughes MJ, Ventham NT, McNally S, Harrison E, Wigmore S. Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis. JAMA Surg. 2014; 149:1224–30.
Author information
Authors and Affiliations
Contributions
Kumar Saurabh: Data collection; Formal analysis; Investigation; Writing-original draft
Sathasivam Sureshkumar: Conceptualization; Supervision; Writing- review and editing
Subair Mohsina: Methodology; Validation; Writing-review and editing
Thulasingam Mahalakshmy: Formal analysis; Supervision; Writing- review and editing
Pankaj Kundra: Formal analysis; Supervision; Writing- review and editing
Vikram Kate: Conceptualization; Formal analysis; Supervision; Validation; Writing- review and editing
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Financial Disclosure
None to Declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saurabh, K., Sureshkumar, S., Mohsina, S. et al. Adapted ERAS Pathway Versus Standard Care in Patients Undergoing Emergency Small Bowel Surgery: a Randomized Controlled Trial. J Gastrointest Surg 24, 2077–2087 (2020). https://doi.org/10.1007/s11605-020-04684-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04684-6