Abstract
Background
Postoperative pancreatic fistula is a main cause of fatal complications post-pancreatoduodenectomy. However, no universally accepted drainage management exists for clinically relevant postoperative pancreatic fistulas. We retrospectively evaluated cases in which drain contrast imaging was used to determine its utility in identifying clinically relevant postoperative pancreatic fistulas post-pancreatoduodenectomy.
Methods
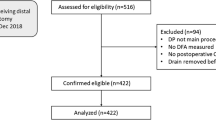
Between January 2014 and December 2018, 209 consecutive patients who underwent pancreatoduodenectomy in our institute were retrospectively analyzed. Drain monitoring with contrast imaging was performed in 47 of the cases. We classified drain contrast type into three categories and evaluated postoperative outcome in each group: (1) fistulous tract group—only the fistula was contrasted; (2) fluid collection group – fluid collection connected to the drain fistula; and (3) pancreatico-anastomotic fistula group—fistula connected to the digestive tract.
Results
The durations of postoperative hospital stay and drainage were significantly shorter in the fistulous tract group than in the fluid collection group (31 vs. 46 days, p = 0.0026; and 12 vs. 38 days, p < 0.0001, respectively). The cost and number of drain exchanges were significantly lower in the fistulous tract group than in the fluid collection group ($163.6 vs. 467.5, p < 0.0001; and 1 vs. 5.5, p < 0.0001, respectively). Notably, no patient had grade C postoperative pancreatic fistula.
Conclusion
Classification of prophylactic drain contrast type can aid in predicting outcomes of clinically relevant postoperative pancreatic fistulas and optimizing drainage management.



Similar content being viewed by others
References
Bassi C, Buchler MW, Fingerhut A, Sarr M. Predictive factors for postoperative pancreatic fistula. Ann Surg 2015;261:e99.
Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, Gumbs A, Pederzoli P. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg 2004;21:54-59.
Zhang H, Zhu F, Shen M, Tian R, Shi CJ, Wang X, Jiang JX, Hu J, Wang M, Qin RY. Systematic review and meta- analysis comparing three techniques for pancreatic remnant closure following distal pancreatectomy. Br J Surg 2015;102:4-15.
Allen PJ, Gonen M, Brennan MF, Bucknor AA, Robinson LM, Pappas MM, Carlucci KE, D'Angelica MI, DeMatteo RP, Kingham TP, Fong Y, Jarnagin WR. Pasireotide for post-operative pancreatic fistula. N Engl J Med 2014;370:2014-2022.
Malleo G, Pulvirenti A, Marchegiani G, Butturini G, Salvia R, Bassi C. Diagnosis and management of postoperative pancreatic fistula. Langenbeck’s Arch Surg 2014;399:801-810.
Vollmer CM Jr, Sanchez N, Gondek S, McAuliffe J, Kent TS, Christein JD, Callery MP; Pancreatic Surgery Mortality Study Group. A root-cause analysis of mortality following major pancreatectomy. J Gastrointest Surg 2012;16:89-102; discussion 102-3.
Kawai M, Tani M, Terasawa H. Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection. Ann Surg 2006;244:1.
McMillan MT, Malleo G, Bassi C, Allegrini V, Casetti L, Drebin JA, Esposito A, Landoni L, Lee MK, Pulvirenti A, Roses RE, Salvia R, Vollmer CM Jr. Multicenter, prospective trial of selective drain management for pancreatoduodenectomy using risk stratification. Ann Surg 2017;265:1209-1218.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Hila MA, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma D, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M; International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 2017;161:584-591.
Faccioli N, Foti G, Molinari E, Hermans JJ, Comai A, Talamini G, Bassi C, Pozzi-Mucelli R. Role of fistulography in evaluating pancreatic fistula after pancreaticoduodenectomy. Br J Radiol 2012;85:219-224.
Hayashibe A, Kameyama M, Shinbo M, Makimoto S. The surgical procedure and clinical results of subtotal stomach preserving pancreaticoduodenectomy (SSPPD) in comparison with pylorus preserving pancreaticoduodenectomy (PPPD). J Surg Oncol 2007;95:106-109.
Fujii T, Sugimoto H, Yamada S, Kanda M, Kanda M, Suenaga M, Takami H, Hattori M, Inokawa Y, Nomoto S, Fujiwara M, Kodera Y. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg 2014;18:1108–1115.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 182 kb)
Rights and permissions
About this article
Cite this article
Kushiya, H., Nakamura, T., Asano, T. et al. Predicting the Outcomes of Postoperative Pancreatic Fistula After Pancreatoduodenectomy Using Prophylactic Drain Contrast Imaging. J Gastrointest Surg 25, 1445–1450 (2021). https://doi.org/10.1007/s11605-020-04646-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04646-y