Abstract
Introduction
The centralisation of pancreatic cancer (PC) services still varies worldwide. This study aimed to assess the impact that a centralisation has had on patients in South Wales, UK.
Methods
A retrospective cohort analysis of patients in South Wales, UK, with PC prior to (2004–2009), and after (2010–2014) the formation of a specialist centre. Patients were identified using record linkage of electronic health records.
Results
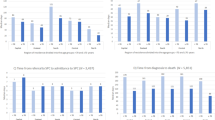
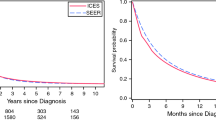
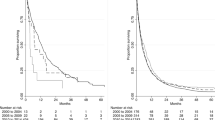
The overall survival (OS) of all 3413 patients with PC increased from a median (IQR) 10 weeks (3–31) to 11 weeks (4–35), p = 0.038, after centralisation. The OS of patients undergoing surgical resection or chemotherapy alone did not improve (93 weeks (39–203) vs. 90 weeks (50–95), p = 0.764 and 33 weeks (20–57) vs. 33 weeks (19–58), p = 0.793). Surgical resection and chemotherapy rates increased (6.1% vs. 9.2%, p < 0.001 and 19.7% vs. 27.0%, p < 0.001). The 30-day mortality rate trended downwards (7.2% vs. 3.6%, p = 0.186). The percentage of patients who received no treatment reduced (75.2% vs. 69.6%, p < 0.001).
Conclusion
The centralisation of PC services in South Wales is associated with a small increase in OS and a larger increase in PC treatment utilisation. It is concerning that many patients still fail to receive any treatments.



Similar content being viewed by others
References
Sun H, Ma H, Hong G, Sun H, Wang J. Survival improvement in patients with pancreatic cancer by decade: a period analysis of the SEER database, 1981-2010. Sci Rep. 2014;4:6747.
Cancer Research UK. Bowel Cancer survival statistics 2014 [Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/survival#heading-Two.
Pancreatic Cancer UK. Cancer Research UK triple research funding into Pancreatic Cancer 2016 [Available from: https://pancreaticcanceraction.org/news/cancer-research-uk-boosts-efforts-overcome-deadliest-cancer-rates-climb/.
Kotteas E, Saif MW, Syrigos K. Immunotherapy for pancreatic cancer. J Cancer Res Clin Oncol. 2016;142(8):1795-805.
Bachmann MO, Alderson D, Peters TJ, Bedford C, Edwards D, Wotton S, Harvey IM. Influence of specialization on the management and outcome of patients with pancreatic cancer. Br J Surg. 2003;90(2):171-7.
Calman H HD. A policy framework for commissioning cancer services. Department of Health. 1995.
NHS. Guidance on commissioning cancer services: improving outcomes in upper gastro-intestinal cancers the manual. 2001.
Lemmens VE, Bosscha K, van der Schelling G, Brenninkmeijer S, Coebergh JW, de Hingh IH. Improving outcome for patients with pancreatic cancer through centralization. Br J Surg. 2011;98(10):1455-62.
Ford DV, Jones KH, Verplancke JP, Lyons RA, John G, Brown G, Brooks CJ, Thompson S, Bodger O, Couch T, Leake K. The SAIL Databank: building a national architecture for e-health research and evaluation. BMC Health Serv Res. 2009;9:157.
Lyons RA, Jones KH, John G, Brooks CJ, Verplancke JP, Ford DV, Brown G, Leake K. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak. 2009;9:3.
Welsh Government. Welsh Index of Multiple deprivation 2015 [Available from: https://gov.wales/statistics-and-research/welsh-index-multiple-deprivation/?lang=en.
Bauer H, Honselmann KC. Minimum Volume Standards in Surgery - Are We There Yet? Visc Med. 2017;33(2):106-16.
Mathur A, Luberice K, Ross S, Choung E, Rosemurgy A. Pancreaticoduodenectomy at High-volume Centers: Surgeon Volume Goes Beyond the Leapfrog Criteria. Ann Surg. 2015;262(2):e37-9.
Pal N, Axisa B, Yusof S, Newcombe RG, Wemyss-Holden S, Rhodes M, Lewis MP. Volume and outcome for major upper GI surgery in England. J Gastrointest Surg. 2008;12(2):353-7.
Mukherjee S, Kocher HM, Hutchins RR, Bhattacharya S, Abraham AT. Impact of hospital volume on outcomes for pancreaticoduodenectomy: a single UK HPB centre experience. Eur J Surg Oncol. 2009;35(7):734-8.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S, Unno M. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Ann Surg. 2016;263(4):664-72.
Walters DM, Lapar DJ, de Lange EE, Sarti M, Stokes JB, Adams RB, Bauer TW. Pancreas-protocol imaging at a high-volume center leads to improved preoperative staging of pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2011;18(10):2764-71.
Mamidanna R, Ni Z, Anderson O, Spiegelhalter SD, Bottle A, Aylin P, Faiz O, Hanna GB. Surgeon Volume and Cancer Esophagectomy, Gastrectomy, and Pancreatectomy: A Population-based Study in England. Ann Surg. 2016;263(4):727-32.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49(12):1076-81.
Wong MCS, Jiang JY, Liang M, Fang Y, Yeung MS, Sung JJY. Global temporal patterns of pancreatic cancer and association with socioeconomic development. Sci Rep. 2017;7(1):3165.
Abel GA, Barclay ME, Payne RA. Adjusted indices of multiple deprivation to enable comparisons within and between constituent countries of the UK including an illustration using mortality rates. BMJ Open. 2016;6(11):e012750.
Gooiker GA, Lemmens VE, Besselink MG, Busch OR, Bonsing BA, Molenaar IQ, Tollenaar RA, de Hingh IH, Wouters MW. Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg. 2014;101(8):1000-5.
Huang L, Jansen L, Balavarca Y, Molina-Montes E, Babaei M, van der Geest L, Lemmens V, Van Eycken L, De Schutter H, Johannesen TB, Fristrup CW, Mortensen MB, Primic-Zakelj M, Zadnik V, Becker N, Hackert T, Magi M, Cassetti T, Sassatelli R, Grutzmann R, Merkel S, Goncalves AF, Bento MJ, Hegyi P, Lakatos G, Szentesi A, Moreau M, van de Velde T, Broeks A, Sant M, Minicozzi P, Mazzaferro V, Real FX, Carrato A, Molero X, Besselink MG, Malats N, Buchler MW, Schrotz-King P, Brennert H. Resection of pancreatic cancer in Europe and USA: an international large-scale study highlighting large variations. Gut. 2019;68(1):130-9.
National Cancer Registration & Analysis Service and Cancer Research UK. Chemotherapy, Radiotherapy and Tumour Resections in England: 2013-2014. 2017.
Public Health Wales. Cancer Incidence in Wales. 2017.
Zijlstra M, van der Geest LGM, van Laarhoven HWM, Lemmens V, van de Poll-Franse LV, Raijmakers NJH. Patient characteristics and treatment considerations in pancreatic cancer: a population based study in the Netherlands. Acta Oncol. 2018;57(9):1185-91.
West Midland Reserach Collaboratives. Receipt of Curative resection Or palliative Care for Hepatopancreaticobiliary Tumours 2018 [Available from: https://ricochetstudy.wixsite.com/ricochet.
Acknowledgements
This study used anonymised data provided by patients, collected by the NHS as part of their care and support, and held in the Secure Anonymised Information Linkage (SAIL) Databank. We would like to acknowledge all data providers that make anonymised data available for research.
Funding
The primary author was supported by an Amser Justin Time grant through Tenovus Cancer care (Grant number AJT2015-01) towards a higher learning degree. This work was supported by Health Data Research UK (NIWA1) which receives its funding from HDR UK Ltd. funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation (BHF) and the Welcome Trust.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of this manuscript. The project was conceived by NGM, HH, GJ and BAS. Data collection and analysis were performed by NGM, RG and AA. Interpretation, drafting and revision of the manuscript were performed by all authors.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Preliminary results of this study were presented to the 13th IHPBA World Congress, Geneva, 2018, as an oral presentation.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Mowbray, N.G., Griffiths, R., Akbari, A. et al. The Impact of a Centralised Pancreatic Cancer Service: a Case Study of Wales, UK. J Gastrointest Surg 26, 367–375 (2022). https://doi.org/10.1007/s11605-020-04612-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04612-8