Abstract
Background
Although previous studies have suggested that drain management is highly variable, data on drain placement and timing of drain removal among patients undergoing hepatic resection remain scarce. The objective of the current study was to define the utilization of drain placement among patients undergoing major hepatic resection.
Methods
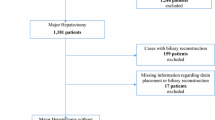
The ACS NSQIP-targeted hepatectomy database was used to identify patients who underwent major hepatectomy between 2014 and 2017. Association between day of drain removal, timing of discharge, and drain fluid bilirubin on postoperative day (POD) 3 (DFB-3) was assessed. Propensity score matching (PSM) was used to compare outcomes of patients with a drain removed before and after POD 3.
Results
Among 5330 patients, most patients had an abdominal drain placed at the time of hepatic resection (n = 3075, 57.7%). Of 2495 patients with data on timing of drain removal, only 380 patients (15.2%) had their drain removed by POD 3. Almost 1 in 6 patients (n = 441, 17.7%) were discharged home with the drain in place. DFB-3 values correlated poorly with POD of drain removal (R2 = 0.0049). After PSM, early drain removal (≤ POD 3) was associated with lower rates of grade B or C bile leakage (2.1% vs. 7.1%, p = 0.008) and prolonged length of hospital stay (6.0% vs. 12.7%, p = 0.009) compared with delayed drain removal (> POD 3).
Conclusions
Roughly 3 in 5 patients had a drain placed at the time of major hepatectomy and only 1 in 7 patients had the drain removed early. This study demonstrated the potential benefits of early drain removal in an effort to improve the quality of care following major hepatectomy.


Similar content being viewed by others
References
Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. Journal of the American College of Surgeons. 2004 2004/07/01/;199(1):31-8.
Merath K, Mehta R, Tsilimigras DI, et al. In-hospital Mortality Following Pancreatoduodenectomy: a Comprehensive Analysis. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2019 Jul 10.
Kneuertz PJ, Pitt HA, Bilimoria KY, et al. Risk of Morbidity and Mortality Following Hepato-Pancreato-Biliary Surgery. Journal of Gastrointestinal Surgery. 2012 September 01;16(9):1727-35.
Merath K, Hyer JM, Mehta R, et al. Use of perioperative epidural analgesia among Medicare patients undergoing hepatic and pancreatic surgery. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2019 Feb 2.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011 2011/05/01/;149(5):680-8.
Yamashita Y, Hamatsu T, Rikimaru T, et al. Bile leakage after hepatic resection. Annals of surgery. 2001 Jan;233(1):45-50.
Mohkam K, Farges O, Vibert E, et al. Risk score to predict biliary leakage after elective liver resection. BJS. 2018;105(1):128-39.
Squires MH, 3rd, Lad NL, Fisher SB, et al. Value of primary operative drain placement after major hepatectomy: a multi-institutional analysis of 1,041 patients. Journal of the American College of Surgeons. 2015 Apr;220(4):396-402.
Guillaud A, Pery C, Campillo B, Lourdais A, Sulpice L, Boudjema K. Incidence and predictive factors of clinically relevant bile leakage in the modern era of liver resections. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2013 Mar;15(3):224-9.
Capussotti L, Ferrero A, Vigano L, Sgotto E, Muratore A, Polastri R. Bile leakage and liver resection: Where is the risk? Archives of surgery (Chicago, Ill : 1960). 2006 Jul;141(7):690-4; discussion 5.
Zimmitti G, Roses RE, Andreou A, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2013 Jan;17(1):57-64; discussion p.-5.
Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Annals of surgery. 2012 Mar;255(3):405-14.
Petrowsky H, Demartines N, Rousson V, Clavien PA. Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Annals of surgery. 2004 Dec;240(6):1074-84; discussion 84-5.
Seykora TF, Liu JB, Maggino L, Pitt HA, Vollmer CM, Jr. Drain Management Following Distal Pancreatectomy: Characterization of Contemporary Practice and Impact of Early Removal. Annals of surgery. 2019 Jan 30.
Rondelli F, Bugiantella W, Vedovati MC, et al. To drain or not to drain extraperitoneal colorectal anastomosis? A systematic review and meta-analysis. Colorectal Disease. 2014;16(2):O35-O42.
Fuster J, Llovet JM, Garcia-Valdecasas JC, et al. Abdominal drainage after liver resection for hepatocellular carcinoma in cirrhotic patients: A randomized controlled study. Hepato-gastroenterology. 2004;51(56):536-40.
Sun H-C, Qin L-X, Lu L, et al. Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. BJS. 2006;93(4):422-6.
Kim YI, Fujita S, Hwang VJ, Nagase Y. Comparison of Abdominal Drainage and No-drainage after Elective Hepatectomy: A Randomized Study. Hepato-gastroenterology. 2014;61(131):707-11.
Gavriilidis P, Hidalgo E, de’Angelis N, Lodge P, Azoulay D. Re-appraisal of prophylactic drainage in uncomplicated liver resections: a systematic review and meta-analysis. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2017 Jan;19(1):16-20.
Butte JM, Grendar J, Bathe O, et al. The role of peri-hepatic drain placement in liver surgery: a prospective analysis. HPB. 2014;16(10):936-42.
Beane JD, House MG, Ceppa EP, Dolejs SC, Pitt HA. Variation in Drain Management After Pancreatoduodenectomy: Early Versus Delayed Removal. Annals of surgery. 2019 Apr;269(4):718-24.
McMillan MT, Malleo G, Bassi C, et al. Multicenter, Prospective Trial of Selective Drain Management for Pancreatoduodenectomy Using Risk Stratification. Annals of surgery. 2017;265(6):1209-18.
Hokuto D, Nomi T, Yasuda S, et al. The safety of the early removal of prophylactic drainage after liver resection based solely on predetermined criteria: a propensity score analysis. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2017 Apr;19(4):359-64.
Raval MV, Pawlik TM. Practical Guide to Surgical Data Sets: National Surgical Quality Improvement Program (NSQIP) and Pediatric NSQIP. JAMA surgery. 2018 Aug 1;153(8):764-5.
Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013 Mar;216(3):420-7.
Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251-67.
Yamazaki S, Takayama T, Moriguchi M, et al. Criteria for drain removal following liver resection. BJS. 2012;99(11):1584-90.
Ishizawa T, Zuker NB, Conrad C, et al. Using a ‘no drain’ policy in 342 laparoscopic hepatectomies: which factors predict failure? HPB. 2014;16(5):494-9.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011 2011/05/01/;149(5):713-24.
Sahara K, Merath K, Hyer JM, et al. Impact of Surgeon Volume on Outcomes and Expenditure Among Medicare Beneficiaries Undergoing Liver Resection: the Effect of Minimally Invasive Surgery. Journal of Gastrointestinal Surgery. 2019 July 19.
Dougherty SH, Simmons RL. The biology and practice of surgical drains. Part 1. Current problems in surgery. 1992 Aug;29(8):559-623.
Kyoden Y, Imamura H, Sano K, et al. Value of prophylactic abdominal drainage in 1269 consecutive cases of elective liver resection. Journal of hepato-biliary-pancreatic sciences. 2010 Mar;17(2):186-92.
Melloul E, Hübner M, Scott M, et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World journal of surgery. 2016 October 01;40(10):2425-40.
Rahbari NN, Elbers H, Koch M, et al. Bilirubin level in the drainage fluid is an early and independent predictor of clinically relevant bile leakage after hepatic resection. Surgery. 2012 Nov;152(5):821-31.
Tanaka K, Kumamoto T, Nojiri K, Takeda K, Endo I. The effectiveness and appropriate management of abdominal drains in patients undergoing elective liver resection: a retrospective analysis and prospective case series. Surgery today. 2013 April 01;43(4):372-80.
Zimmitti G, Vauthey JN, Shindoh J, et al. Systematic use of an intraoperative air leak test at the time of major liver resection reduces the rate of postoperative biliary complications. Journal of the American College of Surgeons. 2013 Dec;217(6):1028-37.
Wang H-Q, Yang J, Yang J-Y, Yan L-N. Bile leakage test in liver resection: a systematic review and meta-analysis. World journal of gastroenterology. 2013;19(45):8420-6.
Xourafas D, Ejaz A, Tsung A, Dillhoff M, Pawlik TM, Cloyd JM. Validation of early drain removal after pancreatoduodenectomy based on modified fistula risk score stratification: a population-based assessment. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2019 Mar 18.
Mitsuka Y, Yamazaki S, Yoshida N, Masamichi M, Higaki T, Takayama T. Prospective Validation of Optimal Drain Management “The 3 x 3 Rule” after Liver Resection. World journal of surgery. 2016 Sep;40(9):2213-20.
Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review Enhanced Recovery After Surgery Enhanced Recovery After Surgery. JAMA surgery. 2017;152(3):292-8.
Bassi C, Molinari E, Malleo G, et al. Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Annals of surgery. 2010 Aug;252(2):207-14.
Costa G, Donadon M, Torzilli G. Post-hepatectomy biliary fistula: from risk factors to the role of drain placement and management—still a lot to be answered. Hepatobiliary surgery and nutrition. 2019;8(4):417-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Precis: The current study showed that considerable variation existed in the use of drain placement and timing of surgical drain removal after major hepatectomy. This study also demonstrated the potential benefits of early drain removal following major hepatectomy.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Sahara, K., Tsilimigras, D.I., Moro, A. et al. Variation in Drain Management Among Patients Undergoing Major Hepatectomy. J Gastrointest Surg 25, 962–970 (2021). https://doi.org/10.1007/s11605-020-04610-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04610-w