Abstract
Purpose
To identify perioperative factors that are significantly associated with complications requiring interventional radiology (IR) treatment after hepatectomy.
Methods
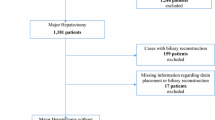
We retrospectively reviewed data from 11,243 patients in the USA who underwent hepatectomy from 2014 to 2016 using the National Surgical Quality Improvement Program database. Data on the following IR procedures were extracted: abscess drain placement, endovascular treatment for bleeding, and postoperative percutaneous biliary drain (PBD) placement up to 30 days postoperatively. Patients’ clinical and intraoperative factors were examined. Population, univariate, and multivariable analyses were performed. P < 0.05 was considered significant.
Results
A total of 704 patients (6%) required IR treatment postoperatively, and 10,539 patients (94%) did not. On multivariable analysis, biliary reconstruction was a significant predictor of postoperative abscess drain placement (hazard ratio (HR), 3.5; 95% confidence interval (CI) 1.8, 6.5; P < .001), endovascular treatment for bleeding (HR, 3.3; 95% CI 1.4, 7.8 P = .006), and postoperative PBD placement (HR, 2.9; 95% CI 1.9, 4.2; P < .001). Compared with hepatectomy without biliary reconstruction, hepatectomy with biliary reconstruction was associated with significantly higher rates of complications treated with IR procedures (26% vs. 4.9%) and death within 30 days (6.0% vs. 1.2%) (both, P < .001).
Conclusion
Biliary reconstruction is a strong predictor of the need for postoperative IR treatment after hepatectomy. One in four patients who underwent biliary reconstruction required IR treatment of a complication during the first 30 days after hepatectomy.

Similar content being viewed by others
References
Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Jr., Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J. Am. Coll. Surg. 2004;199(1):31–38.
Ishii M, Mizuguchi T, Harada K, et al. Comprehensive review of post-liver resection surgical complications and a new universal classification and grading system. World Journal of Hepatology. 2014;6(10):745–751.
Spolverato G, Ejaz A, Kim Y, et al. Patterns of care among patients undergoing hepatic resection: a query of the National Surgical Quality Improvement Program-targeted hepatectomy database. The Journal of Surgical Research. 2015;196(2):221–228.
Benzoni E, Cojutti A, Lorenzin D, et al. Liver resective surgery: a multivariate analysis of postoperative outcome and complication. Langenbeck's Archives of Surgery. 2007;392(1):45–54.
Benzoni E, Molaro R, Cedolini C, et al. Liver resection for HCC: analysis of causes and risk factors linked to postoperative complications. Hepatogastroenterology. 2007;54(73):186–189.
Jin S, Fu Q, Wuyun G, Wuyun T. Management of post-hepatectomy complications. World Journal of Gastroenterology. 2013;19(44):7983–7991.
Khuri SF. The NSQIP: a new frontier in surgery. Surgery. 2005;138(5):837–843.
Belghiti J, Kabbej M, Sauvanet A, Vilgrain V, Panis Y, Fekete F. Drainage after elective hepatic resection. A randomized trial. Ann. Surg. 1993;218(6):748–753.
Butte JM, Grendar J, Bathe O, et al. The role of peri-hepatic drain placement in liver surgery: a prospective analysis. HPB: The Official Journal of the International Hepato Pancreato Biliary Association. 2014;16(10):936–942.
Ferrero A, Lo Tesoriere R, Vigano L, Caggiano L, Sgotto E, Capussotti L. Preoperative biliary drainage increases infectious complications after hepatectomy for proximal bile duct tumor obstruction. World J. Surg. 2009;33(2):318–325.
Ramanathan R, Borrebach J, Tohme S, Tsung A. Preoperative biliary drainage is associated with increased complications after liver resection for proximal cholangiocarcinoma. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2018;22(11):1950–1957.
Zimmitti G, Roses RE, Andreou A, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2013;17(1):57–64; discussion p 64–55.
Gouma DJ, van Geenen RC, van Gulik TM, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann. Surg. 2000;232(6):786–795.
Antolovic D, Koch M, Galindo L, et al. Hepaticojejunostomy--analysis of risk factors for postoperative bile leaks and surgical complications. Journal of Gastrointestinal surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2007;11(5):555–561.
de Castro SM, Kuhlmann KF, Busch OR, et al. Incidence and management of biliary leakage after hepaticojejunostomy. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2005;9(8):1163–1171; discussion 1171-1163.
Piper GL, Peitzman AB. Current management of hepatic trauma. The Surgical Clinics of North America. 2010;90(4):775–785.
Ochsner MG. Factors of failure for nonoperative management of blunt liver and splenic injuries. World Journal of Surgery. 2001;25(11):1393–1396.
Ruscelli P, Gemini A, Rimini M, et al. The role of grade of injury in non-operative management of blunt hepatic and splenic trauma: Case series from a multicenter experience. Medicine. 2019;98(35):e16746.
Brooke-Smith M, Figueras J, Ullah S, et al. Prospective evaluation of the International Study Group for Liver Surgery definition of bile leak after a liver resection and the role of routine operative drainage: an international multicentre study. HPB: the Official Journal of the International Hepato Pancreato Biliary Association. 2015;17(1):46–51.
Kim S, Maynard EC, Shah MB, et al. Risk factors for 30-day readmissions after hepatectomy: analysis of 2444 patients from the ACS-NSQIP database. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2015;19(2):266–271.
Kneuertz PJ, Pitt HA, Bilimoria KY, et al. Risk of morbidity and mortality following hepato-pancreato-biliary surgery. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2012;16(9):1727–1735.
Shwaartz C, Fields AC, Aalberg JJ, Divino CM. Role of drain placement in major hepatectomy: A NSQIP analysis of procedure-targeted hepatectomy cases. World J. Surg. 2017;41(4):1110–1118.
Poon RT, Fan ST, Lo CM, et al. Extended hepatic resection for hepatocellular carcinoma in patients with cirrhosis: is it justified? Ann. Surg. 2002;236(5):602–611.
Zaydfudim VM, Kerwin MJ, Turrentine FE, Bauer TW, Adams RB, Stukenborg GJ. The impact of chronic liver disease on the risk assessment of ACS NSQIP morbidity and mortality after hepatic resection. Surgery. 2016;159(5):1308–1315.
Lillemoe KD, Pitt HA, Cameron JL. Current management of benign bile duct strictures. Adv. Surg. 1992;25:119–174.
Pitt HA, Kaufman SL, Coleman J, White RI, Cameron JL. Benign postoperative biliary strictures. Operate or dilate? Ann. Surg. 1989;210(4):417–425; discussion 426-417.
Wu SM, Marchant LK, Haskal ZJ. Percutaneous interventions in the biliary tree. Semin. Roentgenol. 1997;32(3):228–245.
Ferrero A, Russolillo N, Vigano L, et al. Safety of conservative management of bile leakage after hepatectomy with biliary reconstruction. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2008;12(12):2204–2211.
Adham M, Chopin-Laly X, Lepilliez V, Gincul R, Valette PJ, Ponchon T. Pancreatic resection: drain or no drain? Surgery. 2013;154(5):1069–1077.
Nakayama H, Takayama T, Okubo T, et al. Subcutaneous drainage to prevent wound infection in liver resection: a randomized controlled trial. Journal of hepato-biliary-pancreatic sciences. 2014;21(7):509–517.
Aumont O, Dupre A, Abjean A, et al. Does intraoperative closed-suction drainage influence the rate of pancreatic fistula after pancreaticoduodenectomy? BMC surgery. 2017;17(1):58.
Martin AN, Narayanan S, Turrentine FE, et al. Clinical Factors and Postoperative Impact of Bile Leak After Liver Resection. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2018;22(4):661–667.
Van Buren G, 2nd, Bloomston M, Hughes SJ, et al. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Annals of surgery. 2014;259(4):605–612.
Birkmeyer JD, Shahian DM, Dimick JB, et al. Blueprint for a new American College of Surgeons: National Surgical Quality Improvement Program. J. Am. Coll. Surg. 2008;207(5):777–782.
Alluri RK, Leland H, Heckmann N. Surgical research using national databases. Annals of Translational Medicine. 2016;4(20):393.
Neuman HB, Michelassi F, Turner JW, Bass BL. Surrounded by quality metrics: what do surgeons think of ACS-NSQIP? Surgery. 2009;145(1):27–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Clifford Weiss reports an institutional grant from Merit Medical and Siemens Healthcare and material support from Surefire Medical, as well as institutional grant and payment received for consultancy from BTG and Medtronic. Dr. Kelvin Hong reports receipt of payment from Boston Scientific (as medical advisor) and BTG for consultancy and grants received from BTG and Merit Medical. Other authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kolarich, A.R., Solomon, A.J., Weiss, M.J. et al. Risk Factors for Complications Requiring Interventional Radiological Treatment After Hepatectomy. J Gastrointest Surg 25, 1184–1192 (2021). https://doi.org/10.1007/s11605-020-04609-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04609-3