Abstract
Introduction
Many patients who present for complex surgery have underlying medical comorbidities. While surgeons often refer these patients to medical appointments for preoperative “optimization” or “clearance,” the actual impact of these visits remains poorly examined. The objective of the current study was to define the potential benefit of preoperative medical appointments on outcomes and costs associated with hepatopancreatic (HP) surgery.
Methods
Patients with modifiable comorbidities undergoing HP surgery were identified in the Medicare claims data. The association of preoperative non-surgical visit and postoperative outcomes and expenditures was assessed using inverse propensity treatment weighting analysis and multivariable logistic regression.
Results
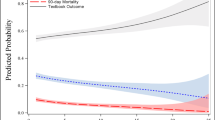
Among the 5574 Medicare beneficiaries who underwent a hepatopancreatic surgery, one in seven patients (n = 830, 14.9%) was “optimized” preoperatively. On multivariable logistic regression analysis, age (OR 1.02; 95% CI 1.01–1.03; p = 0.006) and higher comorbidity burden (OR 1.03; 95% CI 1.01–1.05; p = 0.007) were associated with modest increased odds of being referred in the preoperative period for a non-surgical evaluation; the factor most associated with preoperative non-surgical visit was male patient sex (OR 1.33; 95% CI 1.14–1.56; p < 0.001). After adjustment for competing risk factors and random site effect, patients with an “optimization” visit had 28% lower odds (OR 0.72; 95% CI 0.59–0.86; p < 0.001) of experiencing an operative complication. Additionally, patients who had a non-surgical visit had 13% higher median total expenditures compared with individuals who did not undergo an “optimization” visit (p < 0.05).
Conclusion
In conclusion, roughly one in seven Medicare beneficiaries who underwent HP surgery may have been risk stratified by a non-surgical provider prior to surgery. Preoperative evaluation was associated with modestly lower odds of complications following HP surgery and higher Medicare expenditures. Further research is needed to determine its routine utility as a means to decrease the morbidity surrounding HP surgery.

Similar content being viewed by others
References
Fecho K, Lunney AT, Boysen PG, Rock P, Norfleet EA. Postoperative mortality after inpatient surgery: Incidence and risk factors. Ther Clin Risk Manag. 2008;4(4):681-688.
Nepogodiev D, Martin J, Biccard B, Makupe A, Bhangu A, National Institute for Health Research Global Health Research Unit on Global S. Global burden of postoperative death. Lancet. 2019;393(10170):401.
Scott JW, Olufajo OA, Brat GA, et al. Use of National Burden to Define Operative Emergency General Surgery. JAMA Surg. 2016;151(6):e160480.
Merath K, Chen Q, Bagante F, et al. Synergistic Effects of Perioperative Complications on 30-Day Mortality Following Hepatopancreatic Surgery. J Gastrointest Surg. 2018;22(10):1715-1723.
Merath K, Chen Q, Bagante F, et al. Textbook Outcomes Among Medicare Patients Undergoing Hepatopancreatic Surgery. Ann Surg. 2018.
In: WHO Guidelines for Safe Surgery 2009: Safe Surgery Saves Lives. Geneva 2009.
Kim FJ, da Silva RD, Gustafson D, Nogueira L, Harlin T, Paul DL. Current issues in patient safety in surgery: a review. Patient Saf Surg. 2015;9:26.
Merath K, Hyer JM, Mehta R, et al. Use of Machine Learning for Prediction of Patient Risk of Postoperative Complications After Liver, Pancreatic, and Colorectal Surgery. J Gastrointest Surg. 2019.
Cohen ME, Liu Y, Ko CY, Hall BL. An Examination of American College of Surgeons NSQIP Surgical Risk Calculator Accuracy. J Am Coll Surg. 2017;224(5):787-795.e781.
Santa Mina D, Matthew AG, Hilton WJ, et al. Prehabilitation for men undergoing radical prostatectomy: a multi-centre, pilot randomized controlled trial. BMC Surg. 2014;14:89.
Gillis C, Buhler K, Bresee L, et al. Effects of Nutritional Prehabilitation, With and Without Exercise, on Outcomes of Patients Who Undergo Colorectal Surgery: A Systematic Review and Meta-analysis. Gastroenterology. 2018;155(2):391-410 e394.
Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937-947.
Barberan-Garcia A, Ubre M, Roca J, et al. Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann Surg. 2018;267(1):50-56.
Riggs KR, Segal JB. What is the rationale for preoperative medical evaluations? A closer look at surgical risk and common terminology. Br J Anaesth. 2016;117(6):681-684.
Chan SP, Ip KY, Irwin MG. Peri-operative optimisation of elderly and frail patients: a narrative review. Anaesthesia. 2019;74 Suppl 1:80-89.
Chow WB, Rosenthal RA, Merkow RP, et al. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg. 2012;215(4):453-466.
Alkhatib H, Tastaldi L, Krpata DM, et al. Impact of modifiable comorbidities on 30-day wound morbidity after open incisional hernia repair. Surgery. 2019;166(1):94-101.
Leeds IL, Canner JK, Gani F, et al. Increased Healthcare Utilization for Medical Comorbidities Prior to Surgery Improves Postoperative Outcomes. Ann Surg. 2018.
Rossi M, Iemma D. Patients with comorbidities: what shall we do to improve the outcome. Minerva Anestesiol. 2009;75(5):325-327.
Grocott MPW, Plumb JOM, Edwards M, Fecher-Jones I, Levett DZH. Re-designing the pathway to surgery: better care and added value. Perioper Med (Lond). 2017;6:9.
Sheetz KH, Ibrahim AM, Nathan H, Dimick JB. Variation in Surgical Outcomes Across Networks of the Highest-Rated US Hospitals. JAMA Surg. 2019;154(6):510-515.
Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203(6):865-877.
DuGoff EH, Canudas-Romo V, Buttorff C, Leff B, Anderson GF. Multiple chronic conditions and life expectancy: a life table analysis. Med Care. 2014;52(8):688-694.
Paredes AZ, Beal EW, Bagante F, Dillhoff ME, Cloyd JM, Pawlik TM. Patterns of readmission among the elderly after hepatopancreatobiliary surgery. Am J Surg. 2018.
Vitale A, Spolverato G, Bagante F, et al. A multi-institutional analysis of elderly patients undergoing a liver resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2016;113(4):420-426.
Hoyt DB, Schneidman DS. The American College of Surgeons: an enduring commitment to quality and patient care. Am J Surg. 2015;209(3):436-441.
Weisz D, Gusmano MK, Rodwin VG. Gender and the treatment of heart disease in older persons in the United States, France, and England: a comparative, population-based view of a clinical phenomenon. Gend Med. 2004;1(1):29-40.
Henoch I, Strang S, Lofdahl CG, Ekberg-Jansson A. Management of COPD, equal treatment across age, gender, and social situation? A register study. Int J Chron Obstruct Pulmon Dis. 2016;11:2681-2690.
Mustard CA, Kaufert P, Kozyrskyj A, Mayer T. Sex differences in the use of health care services. N Engl J Med. 1998;338(23):1678-1683.
Bhuyan SS, Shiyanbola O, Deka P, et al. The Role of Gender in Cost-Related Medication Nonadherence Among Patients with Diabetes. J Am Board Fam Med. 2018;31(5):743-751.
Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National Differences in Trends for Heart Failure Hospitalizations by Sex and Race/Ethnicity. Circ Cardiovasc Qual Outcomes. 2017;10(7).
Bhave PD, Lu X, Girotra S, Kamel H, Vaughan Sarrazin MS. Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm. 2015;12(7):1406-1412.
Fabbri E, Zoli M, Gonzalez-Freire M, Salive ME, Studenski SA, Ferrucci L. Aging and Multimorbidity: New Tasks, Priorities, and Frontiers for Integrated Gerontological and Clinical Research. J Am Med Dir Assoc. 2015;16(8):640-647.
Sebastian A, Huddleston P, 3rd, Kakar S, Habermann E, Wagie A, Nassr A. Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5,441 patients from the ACS NSQIP 2005-2012. Spine J. 2016;16(4):504-509.
Ejaz A, Schmidt C, Johnston FM, Frank SM, Pawlik TM. Risk factors and prediction model for inpatient surgical site infection after major abdominal surgery. J Surg Res. 2017;217:153-159.
VanLare JM, Conway PH. Value-based purchasing--national programs to move from volume to value. N Engl J Med. 2012;367(4):292-295.
Howard R, Yin YS, McCandless L, Wang S, Englesbe M, Machado-Aranda D. Taking Control of Your Surgery: Impact of a Prehabilitation Program on Major Abdominal Surgery. J Am Coll Surg. 2019;228(1):72-80.
Sanchez-Lorente D, Navarro-Ripoll R, Guzman R, et al. Prehabilitation in thoracic surgery. J Thorac Dis. 2018;10(Suppl 22):S2593-S2600.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 18 kb).
Rights and permissions
About this article
Cite this article
Paredes, A.Z., Hyer, J.M., Tsilimigras, D.I. et al. Preoperative Medical Referral Prior to Hepatopancreatic Surgery—Is It Worth it?. J Gastrointest Surg 25, 954–961 (2021). https://doi.org/10.1007/s11605-020-04590-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04590-x