Abstract
Importance
Wound complication following gastrointestinal surgery substantially impacts the quality and costs of surgical care. The impact of wound complication on subsequent long-term healthcare utilization has not been fully studied.
Objective
We assessed the impact of surgical wound complication on inpatient and outpatient healthcare utilization in the 2 years after gastrointestinal (GI) surgery.
Design
An observational retrospective cohort study was conducted on Veterans Affairs health system patients who underwent an inpatient GI surgical procedure, were assessed by the Veterans Affairs Surgical Quality Improvement Program (VASQIP), and were discharged alive from Veterans Affairs (VA) hospitals between October 1, 2007 and September 30, 2014.
Setting
Population-based
Participants
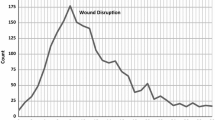
A total of 64,351 patients underwent a GI surgical procedure in the VA system between 2007 and 2014. The cohort was 93.5% male, with a median age of 63.0 years (interquartile range (IQR) 57.0–70.0). A total of 7880 patients (12.2%) had at least one reported wound complication, 5460 of which had their postoperative wound complication classified by a VASQIP nurse.
Exposure
VASQIP-assessed or ICD-9-coded wound complication in the 30 days after surgery
Main Outcome Measurements
Inpatient visits, total inpatient days, outpatient visits, and emergency department visits, and operative interventions up to 2 years after discharge from index admission
Results
Patients with a postoperative wound complication had greater inpatient healthcare utilization compared with no-wound complication for up to 2 years after surgery: inpatient admissions (mean number 3.5 vs. 2.8; P < .001), inpatient bed days (mean 41.0 vs. 25.0; P < .001). Patients with a postoperative wound complication also had greater 2-year outpatient utilization than the no-wound complication cohort: outpatient visits (mean number 92.7 vs. 75.9; P < .001) and emergency department visits (mean 3.5 vs. 2.7; P < .001). The same relationship held for wound-related parameters; inpatient admissions (2.2 vs. 0.4; P < .001); inpatient bed days (21.4 vs. 3.7; P < .001); and outpatient visits (56.2 vs. 9.7; P < .001). A greater proportion of patients in the wound complication cohort had an operative intervention for all time intervals examined (P < .001).
Conclusions
Surgical wound complications impact healthcare utilization patterns for up to 2 years after the index procedure including hospital readmissions and operative interventions; efforts to reduce postoperative wound complications will have substantial effects on patient outcomes and healthcare expenditures well beyond the 30-day postoperative period.


Similar content being viewed by others
References
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. American journal of infection control 2009; 37(5): 387–397
Scott RD. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention. 2009
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Keohane C, Denham CR, Bates DW. Health care–associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA internal medicine 2013; 173(22): 2039–2046
Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surgery 2017; 152(8): 784–791 [DOI: https://doi.org/10.1001/jamasurg.2017.0904]
Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, Tsai TC, Ko CY, Bilimoria KY. Underlying reasons associated with hospital readmission following surgery in the United States. Jama 2015; 313(5): 483–495
Tevis SE, Kohlnhofer BM, Weber SM, Kennedy GD. Postdischarge complications are an important predictor of postoperative readmissions. The American Journal of Surgery 2014; 208(4): 505–510
Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgeons 2012; 215(3): 322–330
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infection Control & Hospital Epidemiology 1999; 20(11): 725–730
Liu V, Lei X, Prescott HC, Kipnis P, Iwashyna TJ, Escobar GJ. Hospital readmission and healthcare utilization following sepsis in community settings. Journal of hospital medicine 2014; 9(8): 502–507
Mull HJ, Graham LA, Morris MS, Rosen AK, Richman JS, Whittle J, Burns E, Wagner TH, Copeland LA, Wahl T. Association of postoperative readmissions with surgical quality using a Delphi consensus process to identify relevant diagnosis codes. JAMA surgery 2018
Zhang D. A coefficient of determination for generalized linear models. The American Statistician 2017; 71(4): 310–316
Neumayer L, Hosokawa P, Itani K, El-Tamer M, Henderson WG, Khuri SF. Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient safety in surgery study. Journal of the American College of Surgeons 2007; 204(6): 1178–1187
Haridas M, Malangoni MA. Predictive factors for surgical site infection in general surgery. Surgery 2008; 144(4): 496–503
Hawn MT, Houston TK, Campagna EJ, Graham LA, Singh J, Bishop M, Henderson WG. The attributable risk of smoking on surgical complications. Annals of surgery 2011; 254(6): 914–920
Paulson EC, Thompson E, Mahmoud N. Surgical Site Infection and Colorectal Surgical Procedures: A Prospective Analysis of Risk Factors. Surgical Infections 2017; 18(4): 520–526
Holt P, Poloniecki J, Hofman D, Hinchliffe R, Loftus I, Thompson M. Re-interventions, readmissions and discharge destination: modern metrics for the assessment of the quality of care. European Journal of Vascular and Endovascular Surgery 2010; 39(1): 49–54
Morris AM, Baldwin L-M, Matthews B, Dominitz JA, Barlow WE, Dobie SA, Billingsley KG. Reoperation as a quality indicator in colorectal surgery: a population-based analysis. Annals of surgery 2007; 245(1): 73
Carey K, Stefos T, Zhao S, Borzecki AM, Rosen AK. Excess costs attributable to postoperative complications. Medical Care Research and Review 2011; 68(4): 490–503
Toneva GD, Deierhoi RJ, Morris M, Richman J, Cannon JA, Altom LK, Hawn MT. Oral antibiotic bowel preparation reduces length of stay and readmissions after colorectal surgery. Journal of the American College of Surgeons 2013; 216(4): 756–762
Morris MS, Graham LA, Chu DI, Cannon JA, Hawn MT. Oral antibiotic bowel preparation significantly reduces surgical site infection rates and readmission rates in elective colorectal surgery. Annals of surgery 2015; 261(6): 1034–1040
Tanner J, Padley W, Assadian O, Leaper D, Kiernan M, Edmiston C. Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8,515 patients. Surgery 2015; 158(1): 66–77
Tanner J, Khan D, Aplin C, Ball J, Thomas M, Bankart J. Post-discharge surveillance to identify colorectal surgical site infection rates and related costs. Journal of Hospital Infection 2009; 72(3): 243–250
Manniën J, Wille JC, Snoeren RL, van den Hof S. Impact of Postdischarge Surveillance on Surgical Site Infection Rates for Several Surgical Procedures Results From the Nosocomial Surveillance Network in The Netherlands. Infection Control & Hospital Epidemiology 2006; 27(8): 809–816
Gao F, Melody T, Daniels DF, Giles S, Fox S. The impact of compliance with 6-hour and 24-hour sepsis bundles on hospital mortality in patients with severe sepsis: a prospective observational study. Critical care 2005; 9(6): R764
Sanger PC, Hartzler A, Han SM, Armstrong CA, Stewart MR, Lordon RJ, Lober WB, Evans HL. Patient perspectives on post-discharge surgical site infections: towards a patient-centered mobile health solution. PLoS One 2014; 9(12): e114016
Evans HL, Lober WB. A pilot use of patient-generated wound data to improve postdischarge surgical site infection monitoring. JAMA surgery 2017; 152(6): 595–596
Anderson DJ, Podgorny K, Berrios-Torres SI, Bratzler DW, Dellinger EP, Greene L, Nyquist A-C, Saiman L, Yokoe DS, Maragakis LL. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infection Control & Hospital Epidemiology 2014; 35(S2): S66-S88
O’malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health services research 2005; 40(5p2): 1620-1639
Morris MS, Deierhoi RJ, Richman JS, Altom LK, Hawn MT. The relationship between timing of surgical complications and hospital readmission. JAMA surgery 2014; 149(4): 348–354
Davis CL, Pierce JR, Henderson W, Spencer CD, Tyler C, Langberg R, Swafford J, Felan GS, Kearns MA, Booker B. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. Journal of the American College of Surgeons 2007; 204(4): 550–560
Author information
Authors and Affiliations
Contributions
Study concept and design: TS, LG, MH. Acquisition of data: LG. Analysis and interpretation of data: TS, LG, KI, MM, SM, MH. Drafting of the manuscript: TS, LG, KI, MM, SM, MH. Critical revision and final approval of the manuscript: TS, LG, MH, KI, MM, SM, MH.
Corresponding author
Ethics declarations
The study was reviewed and approved by the VA Central Institutional Review Board with a waiver of informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sambare, T.D., Graham, L.A., Itani, K.M.F. et al. Impact of Gastrointestinal Surgical Site Wound Complications on Long-term Healthcare Utilization. J Gastrointest Surg 25, 503–511 (2021). https://doi.org/10.1007/s11605-019-04489-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04489-2