Abstract
Background
Surgical resection for asymptomatic, localized, well-differentiated pancreatic neuroendocrine tumors (PNETs) is common yet controversial. Studies using overall survival as an endpoint have shown a benefit for resection; however, these results may be due to treatment selection bias. We assessed the impact of surgery on both overall (OS) and cancer-specific survival (CSS) for asymptomatic patients with stage I PNETs (AJCC 8th edition).
Methods
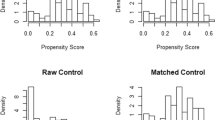
Using SEER data, we identified 709 patients from 2007 to 2015 with well- and moderately differentiated stage I PNETs. We performed Kaplan–Meier survival estimates and adjusted Cox regression for OS and CSS.
Results
Among 709 patients, 628 (88.6%) underwent surgery. There were 37 overall deaths and 11 cancer-specific deaths. All cancer-specific deaths occurred within 3 years of diagnosis. Five-year OS and CSS rates were 89% and 98%, respectively, for the population. Five-year OS rates were 56% in the non-surgical cohort versus 92% in the surgical cohort (log rank, p < 0.001). However, the 5-year CSS rates were similar; 94% in the non-surgical group and 98% in the surgical group (log rank, p = 0.207). On multivariable analysis, surgery predicted improved OS but not CSS.
Conclusion
Although OS is superior in surgically treated stage I PNETs, CSS is not improved, implying treatment selection bias towards surgery being performed in healthier patients. These data suggest that overall survival is a problematic endpoint for the study of asymptomatic, stage I PNETs. Surgery should be individualized for this cohort of patients as the primary cause of death is non-cancer related.

Similar content being viewed by others
References
Fesinmeyer MD, Austin MA, Li CI, De Roos AJ, Bowen DJ. Differences in survival by histologic type of pancreatic cancer. Cancer Epidemiol Biomark Prev 2005;14(7):1766–73. doi:https://doi.org/10.1158/1055-9965.EPI-05-0120.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol 2017;3(10):1335–42. doi:https://doi.org/10.1001/jamaoncol.2017.0589.
Zerbi A, Falconi M, Rindi G, Delle Fave G, Tomassetti P, Pasquali C et al. Clinicopathological features of pancreatic endocrine tumors: a prospective multicenter study in Italy of 297 sporadic cases. Am J Gastroenterol 2010;105(6):1421–9. doi:https://doi.org/10.1038/ajg.2009.747.
Mansour JC, Chavin K, Morris-Stiff G, Warner SG, Cardona K, Fong ZV et al. Management of asymptomatic, well-differentiated PNETs: results of the Delphi consensus process of the Americas Hepato-Pancreato-Biliary Association. HPB : the official journal of the International Hepato Pancreato Biliary Association 2018. https://doi.org/10.1016/j.hpb.2018.09.020.
Kulke MH, Anthony LB, Bushnell DL, de Herder WW, Goldsmith SJ, Klimstra DS et al. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010;39(6):735–52. doi:https://doi.org/10.1097/MPA.0b013e3181ebb168.
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R et al. Recommendations for management of patients with neuroendocrine liver metastases. The Lancet Oncology 2014;15(1):e8–21. doi:https://doi.org/10.1016/S1470-2045(13)70362-0.
Pavel M, Baudin E, Couvelard A, Krenning E, Oberg K, Steinmuller T et al. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012;95(2):157–76. doi:https://doi.org/10.1159/000335597.
Lee LC, Grant CS, Salomao DR, Fletcher JG, Takahashi N, Fidler JL et al. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery. 2012;152(6):965–74. doi:https://doi.org/10.1016/j.surg.2012.08.038.
Sadot E, Reidy-Lagunes DL, Tang LH, Do RK, Gonen M, D'Angelica MI et al. Observation versus Resection for Small Asymptomatic Pancreatic Neuroendocrine Tumors: A Matched Case-Control Study. Ann Surg Oncol 2016;23(4):1361–70. doi:https://doi.org/10.1245/s10434-015-4986-1.
Gaujoux S, Partelli S, Maire F, D'Onofrio M, Larroque B, Tamburrino D et al. Observational study of natural history of small sporadic nonfunctioning pancreatic neuroendocrine tumors. J Clin Endocrinol Metab 2013;98(12):4784–9. doi:https://doi.org/10.1210/jc.2013-2604.
Jung JG, Lee KT, Woo YS, Lee JK, Lee KH, Jang KT et al. Behavior of Small, Asymptomatic, Nonfunctioning Pancreatic Neuroendocrine Tumors (NF-PNETs). Medicine (Baltimore) 2015;94(26):e983. doi:https://doi.org/10.1097/MD.0000000000000983.
Rosenberg AM, Friedmann P, Del Rivero J, Libutti SK, Laird AM. Resection versus expectant management of small incidentally discovered nonfunctional pancreatic neuroendocrine tumors. Surgery. 2016;159(1):302–9. doi:https://doi.org/10.1016/j.surg.2015.10.013.
Sharpe SM, In H, Winchester DJ, Talamonti MS, Baker MS. Surgical resection provides an overall survival benefit for patients with small pancreatic neuroendocrine tumors. J Gastrointest Surg 2015;19(1):117–23; discussion 23. doi:https://doi.org/10.1007/s11605-014-2615-0.
Finkelstein P, Sharma R, Picado O, Gadde R, Stuart H, Ripat C et al. Pancreatic Neuroendocrine Tumors (panNETs): Analysis of Overall Survival of Nonsurgical Management Versus Surgical Resection. J Gastrointest Surg 2017;21(5):855–66. doi:https://doi.org/10.1007/s11605-017-3365-6.
Gratian L, Pura J, Dinan M, Roman S, Reed S, Sosa JA. Impact of extent of surgery on survival in patients with small nonfunctional pancreatic neuroendocrine tumors in the United States. Ann Surg Oncol 2014;21(11):3515–21. doi:https://doi.org/10.1245/s10434-014-3769-4.
Amin MB, Edge SB, American Joint Committee on Cancer. AJCC cancer staging manual. Eighth edition. ed. Switzerland: Springer; 2017.
Surveillance, Epidemiology, and End Results Program Overview. https://seer.cancer.gov/about/factsheets/SEER_Overview.pdf. Accessed 28 Feb 2019.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 2007;165(6):710–8. doi:https://doi.org/10.1093/aje/kwk052.
National Comprehensive Cancer Network. Neuroendocrine and Adrenal Tumors (Version 3.2018). https://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf. Accessed January 20, 2018.
Scott AT, Howe JR. Evaluation and Management of Neuroendocrine Tumors of the Pancreas. Surg Clin North Am 2019;99(4):793–814. doi:https://doi.org/10.1016/j.suc.2019.04.014.
Swanson RS, Pezzi CM, Mallin K, Loomis AM, Winchester DP. The 90-day mortality after pancreatectomy for cancer is double the 30-day mortality: more than 20,000 resections from the national cancer data base. Ann Surg Oncol 2014;21(13):4059–67. doi:https://doi.org/10.1245/s10434-014-4036-4.
Giordano SH, Kuo YF, Duan Z, Hortobagyi GN, Freeman J, Goodwin JS. Limits of observational data in determining outcomes from cancer therapy. Cancer. 2008;112(11):2456–66. doi:https://doi.org/10.1002/cncr.23452.
Acknowledgments
The authors thank Diana Castillo for her assistance with figure preparation.
Author information
Authors and Affiliations
Contributions
Each author participated in the work to take public responsibility for appropriate portions of the content as per the guidelines of the International Committee of Medical Journal Editors (ICMJE). All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published; AND agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Powers, B.D., Rothermel, L.D., Fleming, J.B. et al. A Survival Analysis of Patients with Localized, Asymptomatic Pancreatic Neuroendocrine Tumors: No Surgical Survival Benefit when Examining Appropriately Selected Outcomes. J Gastrointest Surg 24, 2773–2779 (2020). https://doi.org/10.1007/s11605-019-04433-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04433-4