Abstract
Introduction
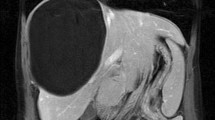
Hydatidosis is a chronic disease that is endemic and prevalent in certain regions of the world. Surgical treatment is the best option, although its main problem is that there is a high rate of recurrence. The objective of the present study was to assess its therapeutic management and the factors related to its postoperative morbidity and relapse.
Material and Methods
A descriptive and retrospective study was made of 238 patients with hepatic hydatidosis operated from January 2006 to December 2017 at our center. An analysis was made of the variables associated with postoperative morbidity and relapse, and of the temporal pattern of that relapse.
Results
Out of 238 patients, radical surgery was performed in 132 (55.5%) and partial cystectomy in 106 of them (44.3%). The postoperative morbidity was 42% (100/238) and the relapse rate was 7.2% (17/238). The factors associated with greater postoperative morbidity were partial cystectomy (OR, 2.83 (1.47–5.43); p = 0.002), ≥ 2 cysts (OR, 3.22 (1.51–6.86); p = 0.002), and biliary fistula (OR, 4.34 (2.11–8.91); p < 0.0001); and those associated with higher relapse rate were history of hydatidosis (OR, 4.98 (1.76–14.11); p = 0.003) and ≥ 2 cysts (OR, 3.23 (1.14–9.11); p = 0.027). The first relapses appeared after 14 months, with the greatest incidence between 14 and 36 months.
Conclusions
The surgical procedure applied is associated with morbidity but not with that of relapse. The observed relapse pattern demonstrates the need to maintain long-term follow-up, but with no follow-up being necessary in the first year. Broader multicenter and prospective studies are needed to establish more precise recommendations.


Similar content being viewed by others
References
Tagliacozzo S, Miccini M, Bonapasta SA, Gregori M, Tocchi A. Surgical treatment of hydatid disease of the liver: 25 years of experience. Am J Surg 2011;201:797–804. DOI: https://doi.org/10.1016/j.amjsurg.2010.02.011
Nabarro LE, Amin Z, Chiodini PL. Current management of cystic echinococcosis: a survey of specialist practice. Clin Infect Dis 2015;60:721–8. DOI: https://doi.org/10.1093/cid/ciu931
Halezeroglu S, Okur E, Tanyü MO. Surgical management for hydatid disease. Thorac Surg Clin 2012;22:375–85. DOI: https://doi.org/10.1016/j.thorsurg.2012.04.004
Georgiou GK, Lianos GD, Lazaros A, Harissis H V, Mangano A, Dionigi G, et al. Surgical management of hydatid liver disease. Int J Surg 2015;20:118–22. DOI: https://doi.org/10.1016/j.ijsu.2015.06.058
Martel G, Ismail S, Bégin A, Vandenbroucke-Menu F, Lapointe R. Surgical management of symptomatic hydatid liver disease: experience from a Western centre. Can J Surg 2014;57:320–6. DOI: https://doi.org/10.1503/cjs.024613
Pakala T, Molina M, Wu GY. Hepatic echinococcal cysts: a review. J Clin Transl Hepatol 2016;4:39–46. DOI: https://doi.org/10.14218/JCTH.2015.00036
Manterola C, Otzen T, Urrutia S, Group M. Risk factors of postoperative morbidity in patients with uncomplicated liver hydatid cyst. Int J Surg 2014;12:695–9. DOI: https://doi.org/10.1016/j.ijsu.2014.05.063
Baraket O, Moussa M, Ayed K, Kort B, Bouchoucha S. Predictive factors of morbidity after surgical treatment of hydatid cyst of the liver. Arab J Gastroenterol 2014;15:119–22. DOI: https://doi.org/10.1016/j.ajg.2014.05.004
Velasco-Tirado V, Romero-Alegría Á, Belhassen-García M, Alonso-Sardón M, Esteban-Velasco C, López-Bernús A, et al. Recurrence of cystic echinococcosis in an endemic area: a retrospective study. BMC Infect Dis 2017;17:1–8. DOI: https://doi.org/10.1186/s12879-017-2556-9
Jerraya H, Khalfallah M, Osman S Ben, Nouira R, Dziri C. Predictive factors of recurrence after surgical treatment for liver hydatid cyst. Surg Endosc 2015;29:86–93. DOI: https://doi.org/10.1007/s00464-014-3637-0
Bedioui H, Bouslama K, Maghrebi H, Farah J, Ayari H, Hsairi H, et al. Predictive factors of morbidity after surgical treatment of hepatic hydatid cyst. Pan Afr Med J. African Field Epidemiology Network; 2012; 13:29.
Touma D, Sersté T, Ntounda R, Mulkay J, Buset M, Van Laethem Y. The liver involvement of the hydatid disease: a systematic review designed for the hepato-gastroenterologist. Acta Gastroenterol Belg 2013;76:210–8.
Brunetti E, Tamarozzi F, Macpherson C, Filice C, Schindler-piontek M, Kabaalioglu A, et al. Ultrasound and cystic echinococcosis. Ultrasound Int Open 2018; 4: 70–78. DOI: https://doi.org/10.1055/a-0650-3807
Escolà-vergé L, Salvador F, Sánchez-montalvá A, Escudero-fernández JM, Sulleiro E, Rando A, et al. Retrospective study of cystic echinococcosis in a recent cohort of a referral center for liver surgery. Journal of Gastrointestinal Surgery; 2018; In press. https://doi.org/10.1007/s11605-018-3971-y
Prousalidis J, Kosmidis C, Anthimidis G, Kapoutzis K, Karamanlis E, Fachantidis E. Postoperative recurrence of cystic hydatidosis. Can J Surg 2012;55:15–20. DOI: https://doi.org/10.1503/cjs.013010
Secchi MA, Pettinari R, Mercapide C, Bracco R, Castilla C, Cassone E, et al. Surgical management of liver hydatidosis: a multicentre series of 1412 patients. Liver Int 2010;30:85–93. DOI: https://doi.org/10.1111/j.1478-3231.2009.02116.x
Haddad MC, Al Awar GN, Jalbout RN, Kanj V, Elkattah R, Faraj W, et al. New trends in the management of hepatic Echinococcus granulosus. J Med Liban. Lebanon; 2011;59:154–9.
Ramia JM, Serrablo A, Serradilla M, Lopez-Marcano A, de la Plaza R, Palomares A. Major hepatectomies in liver cystic echinococcosis: a bi-centric experience. Retrospective cohort study. Int J Surg 2018;54:182–6. DOI: https://doi.org/10.1016/j.ijsu.2018.04.049
i Gavara CG, López-Andújar R, Ibáñez TB, Ángel JMR, Herraiz ÁM, Castellanos FO, et al. Review of the treatment of liver hydatid cysts. World J Gastroenterol WJG 2015;21:124–31. DOI: https://doi.org/10.3748/wjg.v21.i1.124
Ramia JM, Figueras J, De la Plaza R, García-Parreño J. Cysto-biliary communication in liver hydatidosis. Langenbeck’s Arch Surg 2012;397:881–7. DOI: https://doi.org/10.1007/s00423-012-0926-8
Daradkeh S, Husam E-M, Farah G, Sroujieh AS, Abu-Khalaf M. Predictors of morbidity and mortality in the surgical management of hydatid cyst of the liver. Langenbeck’s Arch Surg 2007;392:35–9. DOI: https://doi.org/10.1007/s00423-006-0064-2
Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, Madeddu G, Malaguarnera G, et al. Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol 2012;18:1448–58. DOI: https://doi.org/10.3748/wjg.v18.i13.1448
Author information
Authors and Affiliations
Contributions
Isabel Jaén-Torrejimeno contributed to the acquisition, analysis, and interpretation of data for the work, and drafting of the work. She gives her final approval of the version to be published and agrees to be accountable for all aspects of the work.
Diego López-Guerra contributed to the acquisition and analysis of data for the work and revised it critically. He gives his final approval of the version to be published and agrees to be accountable for all aspects of the work.
Aranzazu Prada-Villaverde contributed to the acquisition of data for the work and revised it critically. She gives her final approval of the version to be published and agrees to be accountable for all aspects of the work.
Gerardo Blanco-Fernández contributed to the conception and design of the work; acquisition, analysis, and interpretation of data for the work; and drafting of the work. He gives his final approval of the version to be published and agrees to be accountable for all aspects of the work.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jaén-Torrejimeno, I., López-Guerra, D., Prada-Villaverde, A. et al. Pattern of Relapse in Hepatic Hydatidosis: Analysis of 238 Cases in a Single Hospital. J Gastrointest Surg 24, 361–367 (2020). https://doi.org/10.1007/s11605-019-04163-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04163-7