Abstract
Background and Aim
Two-stage hepatectomy (TSH) with or without portal vein ligation (PVL) or portal vein embolization (PVE) and associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) are surgical strategies in the treatment of advanced colorectal liver metastases (CRLM). The role of each strategy is yet ill defined. The aim of this analysis is to share our center experience with conventional TSH with or without PVL/PVE and ALPPS in patients with advanced bilateral CRLM.
Patients and Methods
Data were extracted from a prospectively collected institutional database. Complication rates according to the Dindo-Clavien classification, overall and recurrence-free survival data were analyzed.
Results
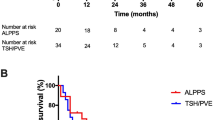
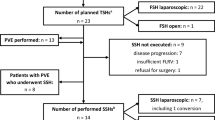
Between 2008 and 2017, 790 liver resections were performed in 611 patients with CRLM. Out of 320 patients with bilateral disease, TSH (as right or extended right hepatectomy) with or without PVL/PVE was performed in 50 patients and ALPPS in 8. Stage 2 was completed in 36 (72%) out of 50 TSH/PVL/PVE and in all ALPPS patients (100%). Median follow-up was 15.8 months (0.9 to 111.9 months). On an intention-to-treat basis, the median overall survival was 26.7 (21.8–35.1 range) months after TSH/PVL/PVE and 36.2 months (11.3–61.2 range) after ALPPS (p = 0.809). In the TSH/PVL/PVE cohort, the median overall survival was 29.9 (19.0–40.3) months in patients who completed stage 2 compared to 13.8 months in patients who did not (p < 0.001). Disease recurred in 60% in the TSH/PVL/PVE cohort and in 87.5% in the ALPPS cohort (p = 0.777). The median recurrence-free survival was 5.9 (1.7–18.6) months after TSH/PVL/PVE and 3 (1.6–14.8) months after ALPPS (p = 0.680).
Conclusion
The treatment of advanced bilateral CRLM remains a surgical and oncological challenge. A tailored approach to bilateral CRLM uses TSH/PVL/PVE as first and ALPPS as second rescue treatment in order to achieve resectability in patients with extensive tumor burden not amenable to one-stage resection. ALPPS should be reserved for patients with no other surgical options.






Similar content being viewed by others
References
Neumann, U.P., D. Seehofer, and P. Neuhaus, The surgical treatment of hepatic metastases in colorectal carcinoma. Dtsch Arztebl Int, 2010. 107(19): p. 335–42.
Adam, R., et al., Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol, 2009. 27(11): p. 1829–35.
Wicherts, D.A., R.J. de Haas, and R. Adam, Bringing unresectable liver disease to resection with curative intent. Eur J Surg Oncol, 2007. 33 Suppl 2: p. S42–51.
Clavien, P.A., et al., Strategies for safer liver surgery and partial liver transplantation. N Engl J Med, 2007. 356(15): p. 1545–59.
Lang, H., J. Baumgart, and J. Mittler, Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy in the Treatment of Colorectal Liver Metastases: Current Scenario. Dig Surg, 2018. 35(4): p. 294–302.
Folprecht, G., et al., Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol, 2005. 16(8): p. 1311–9.
Adam, R., et al., Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg, 2000. 232(6): p. 777–85.
Brouquet, A., et al., High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol, 2011. 29(8): p. 1083–90.
Cardona, K., et al., Treatment of extensive metastatic colorectal cancer to the liver with systemic and hepatic arterial infusion chemotherapy and two-stage hepatic resection: the role of salvage therapy for recurrent disease. Ann Surg Oncol, 2014. 21(3): p. 815–21.
Jaeck, D., et al., A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg, 2004. 240(6): p. 1037–49; discussion 1049-51.
Wicherts, D.A., et al., Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg, 2008. 248(6): p. 994–1005.
Heinrich, S. and H. Lang, Liver metastases from colorectal cancer: technique of liver resection. J Surg Oncol, 2013. 107(6): p. 579–84.
Ratti, F., et al., Strategies to Increase the Resectability of Patients with Colorectal Liver Metastases: A Multi-center Case-Match Analysis of ALPPS and Conventional Two-Stage Hepatectomy. Ann Surg Oncol, 2015. 22(6): p. 1933–42.
Passot, G., et al., Predictors of Safety and Efficacy of 2-Stage Hepatectomy for Bilateral Colorectal Liver Metastases. J Am Coll Surg, 2016. 223(1): p. 99–108.
Vigano, L., et al., Drop-out between the two liver resections of two-stage hepatectomy. Patient selection or loss of chance? Eur J Surg Oncol, 2016. 42(9): p. 1385–93.
Schnitzbauer, A.A., et al., Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg, 2012. 255(3): p. 405–14.
Lang, H., ALPPS for Colorectal Liver Metastases. J Gastrointest Surg, 2017. 21(1): p. 190–192.
Oldhafer, K.J., et al., ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg, 2014. 38(6): p. 1504–9.
Hernandez-Alejandro, R., et al., Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases? Surgery, 2015. 157(2): p. 194–201.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205–13.
Mullen, J.T., et al., Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg, 2007. 204(5): p. 854–62; discussion 862-4.
Brudvik, K.W., et al., RAS Mutation Clinical Risk Score to Predict Survival After Resection of Colorectal Liver Metastases. Ann Surg, 2017.
Adam, R., et al., Outcome after associating liver partition and portal vein ligation for staged hepatectomy and conventional two-stage hepatectomy for colorectal liver metastases. Br J Surg, 2016. 103(11): p. 1521–9.
Simoneau, E., et al., Portal vein embolization and its effect on tumour progression for colorectal cancer liver metastases. Br J Surg, 2015. 102(10): p. 1240–9.
Giuliante, F., et al., Tumor progression during preoperative chemotherapy predicts failure to complete 2-stage hepatectomy for colorectal liver metastases: results of an Italian multicenter analysis of 130 patients. J Am Coll Surg, 2014. 219(2): p. 285–94.
Abdalla, E.K., et al., Resection of hepatic colorectal metastases involving the caudate lobe: perioperative outcome and survival. J Gastrointest Surg, 2007. 11(1): p. 66–72.
Narita, M., et al., Two-stage hepatectomy for multiple bilobar colorectal liver metastases. Br J Surg, 2011. 98(10): p. 1463–75.
Imai, K., et al., Failure to Achieve a 2-Stage Hepatectomy for Colorectal Liver Metastases: How to Prevent It? Ann Surg, 2015. 262(5): p. 772–8; discussion 778-9.
Moris, D., et al., Operative Results and Oncologic Outcomes of Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Versus Two-Stage Hepatectomy (TSH) in Patients with Unresectable Colorectal Liver Metastases: A Systematic Review and Meta-Analysis. World J Surg, 2018. 42(3): p. 806–815.
Vigano, L., et al., Is Tumor Detachment from Vascular Structures Equivalent to R0 Resection in Surgery for Colorectal Liver Metastases? An Observational Cohort. Ann Surg Oncol, 2016. 23(4): p. 1352–60.
Vigano, L., et al., R1 Resection for Colorectal Liver Metastases: a Survey Questioning Surgeons about Its Incidence, Clinical Impact, and Management. J Gastrointest Surg, 2018.
Hosokawa, I., et al., Long-Term Survival Benefit and Potential for Cure after R1 Resection for Colorectal Liver Metastases. Ann Surg Oncol, 2016. 23(6): p. 1897–905.
Torzilli, G., et al., Is Enhanced One-Stage Hepatectomy a Safe and Feasible Alternative to the Two-Stage Hepatectomy in the Setting of Multiple Bilobar Colorectal Liver Metastases? A Comparative Analysis between Two Pioneering Centers. Dig Surg, 2018. 35(4): p. 323–332.
Karoui, M., et al., Combined first-stage hepatectomy and colorectal resection in a two-stage hepatectomy strategy for bilobar synchronous liver metastases. Br J Surg, 2010. 97(9): p. 1354–62.
Pamecha, V., et al., Prospective evaluation of two-stage hepatectomy combined with selective portal vein embolisation and systemic chemotherapy for patients with unresectable bilobar colorectal liver metastases. Dig Surg, 2008. 25(5): p. 387–93.
Vigano, L., et al., Early recurrence after liver resection for colorectal metastases: risk factors, prognosis, and treatment. A LiverMetSurvey-based study of 6,025 patients. Ann Surg Oncol, 2014. 21(4): p. 1276–86.
Sandstrom, P., et al., ALPPS Improves Resectability Compared With Conventional Two-stage Hepatectomy in Patients With Advanced Colorectal Liver Metastasis: Results From a Scandinavian Multicenter Randomized Controlled Trial (LIGRO Trial). Ann Surg, 2018. 267(5): p. 833–840.
Schnitzbauer, A.A., et al., Indicating ALPPS for Colorectal Liver Metastases: A Critical Analysis of Patients in the International ALPPS Registry. Surgery, 2018.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baumgart, J., Jungmann, F., Bartsch, F. et al. Two-Stage Hepatectomy and ALPPS for Advanced Bilateral Liver Metastases: a Tailored Approach Balancing Risk and Outcome. J Gastrointest Surg 23, 2391–2400 (2019). https://doi.org/10.1007/s11605-019-04145-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04145-9