Abstract
Background
The use of synthetic adhesives such as cyanoacrylates has been established previously for a wide range of clinical indications. However, more research is necessary to evaluate their use in digestive closures or anastomosis. New chemical formulations developed to achieve more flexibility of synthetic adhesives (i.e., based on n-butyl-2-cyanoacrylate) could be an alternative to achieve this purpose. The aim of this study was to investigate the feasibility of using flexible cyanoacrylate adhesives for large gastric incision closure in an animal model.
Methods
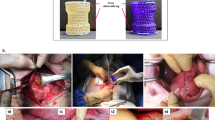
Twelve farm pigs were divided in two groups depending on the type of closure method applied. In all cases, extra-large seven centimeters gastrostomies were performed. Braided absorbable hand-sewn interrupted suture versus n-butyl-2-cyanoacrylate with softener closure were compared during a 3-week follow-up period. Histopathological aspects, hematologic and inflammatory biomarkers, and endoluminal pressure tolerated until leakage were assessed. The time spent on both closing procedures was compared.
Results
No differences between the two groups were found in any of the histopathological and inflammatory variables evaluated. The glued group tolerated a significantly higher pressure than the manual suture group. A reduction of surgery time was also observed.
Conclusions
Our results suggest that flexible cyanoacrylates could be a feasible alternative to improve the clinical outcome of the closure of hollow viscera through more efficient sutureless procedures.



Similar content being viewed by others
References
Sheridan CB, Zyromski N, Mattar S. How to always do a safe anastomosis. Contemp Surg. 2008;64:68–74.
Oh SJ, Choi WB, Song J, et al. Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg. 2009;13:239–245.
Sparreboom CL, Wu ZQ, Ji JF, et al. Integrated approach to colorectal anastomotic leakage: Communication, infection and healing disturbances. World J Gastroenterol. 2016;22:7226–7235.
Bhatia SK, Yetter AB. Correlation of visual in vitro cytotoxicity ratings of biomaterials with quantitative in vitro cell viability measurements. Cell Biol Toxicol. 2008;24:315–319.
Pascual G, Sotomayor S, Rodríguez M, et al. Cytotoxicity of Cyanoacrylate-Based Tissue Adhesives and Short-Term Preclinical In Vivo Biocompatibility in Abdominal Hernia Repair. PLoS One. 2016;11:e0157920.
Mizrahi B, Stefanescu CF, Yang C, et al. Elasticity and safety of alkoxyethyl cyanoacrylate tissue adhesives. Acta Biomater. 2011;7:3150–3157.
Montanaro L, Arciola CR, Cenni E, et al. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials. 2001;22:59–66.
Pratt GF, Rozen WM, Westwood A, et al. Technology-assisted and sutureless microvascular anastomoses: evidence for current techniques. Microsurgery. 2012;32:68–76.
Lumsden AB, Heyman ER. Closure Medical Surgical Sealant Study Group. Prospective randomized study evaluating an absorbable cyanoacrylate for use in vascular reconstructions. J Vasc Surg. 2006;44:1002–1009.
Piñeros-Fernández A, Rodeheaver PF, Rodeheaver GT. Octyl 2-cyanoacrylate for repair of peripheral nerve. Ann Plast Surg. 2005;55:188–195.
Paral J, Subrt Z, Lochman P, et al. Suture-free anastomosis of the colon. Experimental comparison of two cyanoacrylate adhesives. J Gastrointest Surg. 2011;15:451–459.
Bae KB, Kim SH, Jung SJ, et al. Cyanoacrylate for colonic anastomosis; is it safe? Int J Colorectal Dis. 2010;25:601–606.
Ozmen MM, Ozlap N, Zulfikagoru B, et al. Hystoacryl blue versus sutured left colonic anastomosis: experimental study. ANZ J Surg. 2004;74:1107–1110.
Donkerwolcke M, Burny F, Muster D. Tissues and bone adhesives--historical aspects. Biomaterials. 1998;19:1461–1466.
Cho E, Jun CH, Cho SB, et al. Endoscopic variceal ligation-induced ulcer bleeding: What are the risk factors and treatment strategies? Medicine (Baltimore) 2017;96:e7157.
Buechter M, Kahraman A, Manka P, et al. Partial spleen embolization reduces the risk of portal hypertension-induced upper gastro-intestinal bleeding in patients not eligible for TIPS implantation. PLoS One. 2017;12:e0177401.
Holster IL, Tjwa ET, Moelker A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016;63:581–589.
Kozie S, Kobryñ K, Paluszkiewicz R, et al. Endoscopic treatment of gastric varices bleeding with the use of n-butyl-2 cyanoacrylate. Prz Gastroenterol. 2015;10:239–243.
Jang WS, Shin HP, Lee JI, et al. Proton pump inhibitor administration delays rebleeding after endoscopic gastric variceal obturation. World J Gastroenterol. 2014;20:17127–17131.
Lo GH, Lin CW, Perng DS, et al. A retrospective comparative study of histoacryl injection and banding ligation in the treatment of acute type 1 gastric variceal hemorrhage. Scand J Gastroenterol. 2013;48:1198–1204.
Prachayakul V, Aswakul P, Chantarojanasiri T, et al. Factors influencing clinical out-comes of Histoacryl® glue injection-treated gastric variceal hemorrhage. World J Gastroenterol. 2013;19:2379–2387.
Liew W, Wai YY, Kosai NR, et al. Tackers versus glue mesh fixation: an objective assessment of postoperative acute and chronic pain using inflammatory markers. Hernia. 2017;21:549–554.
Silveira RK, Domingie S, Kirzin S, et al. Comparative study of safety and efficacy of synthetic surgical glue for mesh fixation in ventral rectopexy. Surg Endosc. 2017;31:4016–4024.
Dauser B, Szyszkowitz A, Seitinger G, et al. A novel glue device for fixation of mesh and peritoneal closure during laparoscopic inguinal hernia repair: short- and medium-term results. Eur Surg. 2017;49:27–31.
Shen YM, Liu YT, Chen J, et al. Efficacy and safety of NBCA (n-butyl-2-cyanoacrylate) medical adhesive for patch fixation in totally extraperitoneal prosthesis (TEP): a prospective, randomized, controlled trial. Eur Rev Med Pharmacol Sci. 2017;21:680–686.
Yontar Y, Özyazgan Ý. Correcting Concavity of Rabbit Auricular Cartilage: Comparison of Single Scoring Incisions with Butyl Cyanoacrylate-Aided Techniques. Plast Reconstr Surg. 2017;139:1152–1164.
Dundar S, Ozgur C, Yaman F, et al. Guided bone regeneration with local zoledronic acid and titanium barrier: An experimental study. Exp Ther Med. 2016;12:2015–2020.
Salata LA, Mariguela VC, Antunes AA, et al. Short-term evaluation of grafts fixed with either N-butyl-2-cyanocrylate or screws. J Oral Maxillofac Surg. 2014;72:676–682.
de Oliveira Neto PJ, Cricchio G, Hawthorne AC, et al. Tomographic, histological, and immunohistochemical evidences on the use of N-butyl-2-cyanoacrilate for onlay graft fixation in rabbits. Clin Implant Dent Relat Res. 2012;14:861–71.
Ekelund A, Nilsson OS. Tissue adhesives inhibit experimental new bone formation. Int Orthop. 1991;15:331–334.
Wells JR, Gernon WH. Bony ossicular fixation using 2-cyano-butyl-acrylate adhesive. Ach Otolaryngol Head Neck Surg. 1987;113:644–646.
Koltai PJ, Eden AR. Evaluation of three cyanoacrylate glues for ossicular reconstruction. Ann Otol Rhinol Laryngol. 1983;92:29–32.
Weiss M, Haj M. Gastrointestinal anastomosis with histoacryl glue in rats. J Invest Surg. 2001;14:9–13.
Yurtçu M, Arbag H, Cağlayan O, et al. The effect of cyanoacrylate in esophagocutaneous leakages occurring after esophageal anastomosis. Int J Pediatr Otorhinolaryngol. 2009;73:1053–1055.
Bianchi Cardona A, Hidalgo Grau LA, Feliu Canaleta J, et al. Postoperative cervical anastomotic fistula treated with a biologic glue. Eur J Surg Oncol. 2005;31:1222–1223.
Lukish J, Marmon L, Burns C. Nonoperative closure of persistent gastrocutaneous fistulas in children with 2-octylcyanoacrylate. J Laparoendosc Adv Surg Tech A. 2010;206:565–567.
Wu Z, Boersema GS, Vakalopoulos KA, et al. Critical analysis of cyanoacrylate in intestinal and colorectal anastomosis. J Biomed Mater Res B Appl Biomater. 2014;102:635–642.
Julián Ibáñez JF, Tarascó Palomares J, Navinés López J, et al. Introduction of Flexible Cyanoacrylates in Sutureless Gastric Closure. Surg Innov. 2016;23:490–497.
Festing S, Wilkinson R. The ethics of animal research. Talking Point on the use of animals in scientific research. EMBO Reports. 2007;8(6):526–530.
Zühlke HV, Lorenz EM, Straub EM, et al. Pathophysiology and classification of adhesions. Langenbecks Arch Chir Verh Dtsch Ges Chir. 1990:1009–1016.
Paral J, Subrt Z, Lochman P, et al. Suture-free anastomosis of the colon. Experimental comparison of two cyanoacrylate adhesives. J Gastrointest Surg. 2011;15:451–459.
Nursal TZ, Anarat R, Bircan S, et al. The effect of tissue adhesive, octyl-cyanoacrylate, on the healing of experimental high-risk and normal colonic anastomoses. Am J Surg. 2004;187:28–32.
Matsumoto MT, Hardaway RM 3rd, Pani KC, et al. Closure of gastrointestinal perforations with cyanocrylate tissue adhesive. Arch Surg. 1967;94:184–186.
Ersoy OF, Ozkan N, Celik A, et al. Effect of cyanocrylate on closure of gastric perforation: a comparative study in a rat model. Minim Invasive Ther Allied Technol. 2009;18:225–231.
Howell JM, Bresnahan KA, Stair TO, et al. Comparison of effects of suture and cyanoacrylate tissue adhesive on bacterial counts in contaminated lacerations. Antimicrob Agents Chemother. 1995;39:559–560.
Bot GM, Bot KG, Ogunranti JO, et al. The use of cyanoacrylate in surgical anastomosis: an alternative to microsurgery. J Surg Tech Case Rep. 2010;2:44–48.
Phillips RJ, Powley TL. Plasticity of vagal afferents at the site of an incision in the wall of the stomach. Auton Neurosci. 2005;123:44–53.
Vakalopoulos KA, Wu Z, Kroese LF, et al. Clinical, mechanical, and immunohistopathological effects of tissue adhesives on the colon: An in-vivo study. J Biomed Mater Res B Appl Biomater. 2016;105:846–854.
Author information
Authors and Affiliations
Contributions
JF. Julian and J. Fernández-Llamazares participated in the conception, design, surgical procedures in pigs and final critical revision.
P. Turon, AM Rodríguez, LF. del Castillo and E. Díaz participated in the conception, design, execution and final critical revision.
F. Espin and I. Vorisova contributed to analysis, interpretation of data, structure and drafting.
J. Navinés and J. Tarascó participated in the acquisition, analysis and interpretation of data.
Corresponding author
Ethics declarations
The authors declare that the Investigational Review Board and the Ethical committee of our institution approved the study and that they have no conflict of interest.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The present work has been developed under agreement between B. Braun Surgical, S.A. and The Catalonian Public Health Institute (ICS), Barcelona, Spain. The authors disclosed that Histoacryl® Flexible was employed for investigational use. Histoacryl® Flexible is not approved for internal use, only for skin closure.
Rights and permissions
About this article
Cite this article
Espin Alvarez, F., Rodríguez Rivero, A.M., Navinés López, J. et al. Clinical Feasibility of Large Gastrotomy Closure Using a Flexible Tissue Glue Based on N-Butyl-2-Cyanoacrylate: Experimental Study in Pigs. J Gastrointest Surg 23, 247–255 (2019). https://doi.org/10.1007/s11605-018-3910-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3910-y