Abstract
Background
Patients undergoing colon resection for Crohn’s disease are at risk of developing postoperative complications. The aim of this study is to identify factors associated with short-term (30-day) morbidity in patients undergoing colon resection for Crohn’s disease from a national database.
Methods
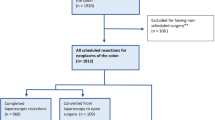
Patients who underwent colon resection for Crohn’s disease in 2015 were identified from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. The groups were classified based on presence of postoperative 30-day complications. The overall morbidity was calculated by including patients who had at least one postoperative complication. Demographics, preoperative, and operative factors were assessed and compared between the two groups. Further multivariate logistic regression analysis was conducted.
Results
A total of 1643 patients met the inclusion criteria [mean age of 41.2 (± 15.5) years, 871 (53%) female]. Sixty percent (n = 993) of the procedures were performed laparoscopically and 128 (12.8%) cases were converted to open. Ninety-five patients (5%) underwent emergent resections. Thirty percent (n = 507) of patients had at least one postoperative complication within 30 days of surgery. Ileus (16%), transfusion (7%), and organ-space surgical site infection (6%) were the most common morbidities. Independent risk factors for postoperative morbidity were male gender (p = 0.01), open surgery (p = 0.002), preoperative severe anemia (p = 0.001), and preoperative weight loss (p = 0.04).
Conclusion
Approximately one third of the patients who undergo colon resection for Crohn’s disease experience postoperative complications. Preoperative optimization of nutrition and anemia may improve outcomes. Laparoscopic technique appears to be the preferred surgical treatment option for resection when feasible.
Similar content being viewed by others
References
Frolkis AD, Dykeman J, Negron ME, Debruyn J, Jette N, Fiest KM et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145(5):996–1006. https://doi.org/10.1053/j.gastro.2013.07.041.
Yamamoto T, Watanabe T. Surgery for luminal Crohn's disease. World journal of gastroenterology. 2014;20(1):78–90. https://doi.org/10.3748/wjg.v20.i1.78.
Toh JW, Stewart P, Rickard MJ, Leong R, Wang N, Young CJ. Indications and surgical options for small bowel, large bowel and perianal Crohn's disease. World Journal of Gastroenterology. 2016;22(40):8892–904. https://doi.org/10.3748/wjg.v22.i40.8892.
Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB et al. The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Annals of surgery. 1998;228(4):491–507.
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Jr. et al. Successful implementation of the Department of Veterans Affairs' National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Annals of surgery. 2008;248(2):329–36. https://doi.org/10.1097/SLA.0b013e3181823485.
American College of Surgeons. User Guide for the 2015 ACS NSQIP Participant Use Data File (PUF). https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_user_guide_2015.ashx. Accessed November 2, 2016.
American College of Surgeons User Guide for the 2015 ACS NSQIP Procedure Targeted Participant Use Data File (PUF). 2016. https://www.facs.org/~/media/files/quality%20programs/nsqip/pt_nsqip_puf_user_guide_2015.ashx. Accessed November 2, 2016.
Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Canadian Journal of Gastroenterology = Journal Canadien de Gastroenterologie. 2005;19 Suppl A:5a-36a.
Group WS. Nutritional anaemias. World Health Organization Technical Report Series. 1968;405:1–40.
Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet (London, England). 2011;378(9800):1396–407. https://doi.org/10.1016/s0140-6736(11)61381-0.
Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. The American Journal of Medicine. 2004;116 Suppl 7A:58s–69s. https://doi.org/10.1016/j.amjmed.2003.12.013.
Kim NK, Senagore AJ, Luchtefeld MA, MacKeigan JM, Mazier WP, Belknap K et al. Long-term outcome after ileocecal resection for Crohn's disease. The American surgeon. 1997;63(7):627–33.
Goyer P, Alves A, Bretagnol F, Bouhnik Y, Valleur P, Panis Y. Impact of complex Crohn's disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Diseases of the colon and rectum. 2009;52(2):205–10. https://doi.org/10.1007/DCR.0b013e31819c9c08.
Masoomi H, Carmichael JC, Mills S, Pigazzi A, Stamos MJ. Predictive risk factors of early postoperative enteric fistula in colon and rectal surgery. The American surgeon. 2013;79(10):1058–63.
Handler M, Dotan I, Klausner JM, Yanai H, Neeman E, Tulchinsky H. Clinical recurrence and re-resection rates after extensive vs. segmental colectomy in Crohn's colitis: a retrospective cohort study. Techniques in coloproctology. 2016;20(5):287–92. https://doi.org/10.1007/s10151-016-1440-8.
Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ journal of surgery. 2006;76(7):579–85. https://doi.org/10.1111/j.1445-2197.2006.03780.x.
Tilney HS, Constantinides VA, Heriot AG, Nicolaou M, Athanasiou T, Ziprin P et al. Comparison of laparoscopic and open ileocecal resection for Crohn's disease: a metaanalysis. Surgical endoscopy. 2006;20(7):1036–44. https://doi.org/10.1007/s00464-005-0500-3.
Tan JJ, Tjandra JJ. Laparoscopic surgery for Crohn's disease: a meta-analysis. Diseases of the colon and rectum. 2007;50(5):576–85. https://doi.org/10.1007/s10350-006-0855-0.
Lee Y, Fleming FJ, Deeb AP, Gunzler D, Messing S, Monson JR. A laparoscopic approach reduces short-term complications and length of stay following ileocolic resection in Crohn's disease: an analysis of outcomes from the NSQIP database. Colorectal disease : The Official Journal of the Association of Coloproctology of Great Britain and Ireland. 2012;14(5):572–7. https://doi.org/10.1111/j.1463-1318.2011.02756.x.
Stocchi L, Milsom JW, Fazio VW. Long-term outcomes of laparoscopic versus open ileocolic resection for Crohn's disease: follow-up of a prospective randomized trial. Surgery. 2008;144(4):622–7; discussion 7-8. https://doi.org/10.1016/j.surg.2008.06.016.
Lesperance K, Martin MJ, Lehmann R, Brounts L, Steele SR. National trends and outcomes for the surgical therapy of ileocolonic Crohn's disease: a population-based analysis of laparoscopic vs. open approaches. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2009;13(7):1251–9. https://doi.org/10.1007/s11605-009-0853-3.
Strong S, Steele SR, Boutrous M, Bordineau L, Chun J, Stewart DB et al. Clinical Practice Guideline for the Surgical Management of Crohn's Disease. Diseases of the colon and rectum. 2015;58(11):1021–36. https://doi.org/10.1097/dcr.0000000000000450.
Kristo I, Stift A, Argeny S, Mittlbock M, Riss S. Minimal-invasive approach for penetrating Crohn's disease is not associated with increased complications. Surgical Endoscopy. 2016;30(12):5239–44. https://doi.org/10.1007/s00464-016-4871-4.
Eshuis EJ, Polle SW, Slors JF, Hommes DW, Sprangers MA, Gouma DJ et al. Long-term surgical recurrence, morbidity, quality of life, and body image of laparoscopic-assisted vs. open ileocolic resection for Crohn's disease: a comparative study. Diseases of the Colon and Rectum. 2008;51(6):858–67. https://doi.org/10.1007/s10350-008-9195-6.
Efron JE, Young-Fadok TM. Preoperative optimization of Crohn's disease. Clinics in colon and rectal surgery. 2007;20(4):303–8. https://doi.org/10.1055/s-2007-991029.
Patel KV, Darakhshan AA, Griffin N, Williams AB, Sanderson JD, Irving PM. Patient optimization for surgery relating to Crohn's disease. Nature reviews Gastroenterology & hepatology. 2016;13(12):707–19. https://doi.org/10.1038/nrgastro.2016.158.
White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN Journal of parenteral and enteral nutrition. 2012;36(3):275–83. https://doi.org/10.1177/0148607112440285.
Lindor KD, Fleming CR, Ilstrup DM. Preoperative nutritional status and other factors that influence surgical outcome in patients with Crohn's disease. Mayo Clinic proceedings. 1985;60(6):393–6.
Lochs H, Dejong C, Hammarqvist F, Hebuterne X, Leon-Sanz M, Schutz T et al. ESPEN Guidelines on Enteral Nutrition: Gastroenterology. Clinical Nutrition (Edinburgh, Scotland). 2006;25(2):260–74. https://doi.org/10.1016/j.clnu.2006.01.007.
Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clinical Nutrition (Edinburgh, Scotland). 2007;26(6):698–709. https://doi.org/10.1016/j.clnu.2007.06.009.
Yamada A, Komaki Y, Patel N, Komaki F, Aelvoet AS, Tran AL et al. Risk of Postoperative Complications Among Inflammatory Bowel Disease Patients Treated Preoperatively With Vedolizumab. The American journal of gastroenterology. 2017;112(9):1423–9. https://doi.org/10.1038/ajg.2017.201.
Wagner IJ, Rombeau JL. Nutritional support of surgical patients with inflammatory bowel disease. The Surgical clinics of North America. 2011;91(4):787–803, viii. https://doi.org/10.1016/j.suc.2011.04.013.
Jacobson S. Early postoperative complications in patients with Crohn's disease given and not given preoperative total parenteral nutrition. Scandinavian Journal of Gastroenterology. 2012;47(2):170–7. https://doi.org/10.3109/00365521.2011.648954.
Dreznik Y, Horesh N, Gutman M, Gravetz A, Amiel I, Jacobi H et al. Preoperative Nutritional Optimization for Crohn's Disease Patients Can Improve Surgical Outcome. Digestive Surgery. 2017. https://doi.org/10.1159/000481408.
Filmann N, Rey J, Schneeweiss S, Ardizzone S, Bager P, Bergamaschi G et al. Prevalence of anemia in inflammatory bowel diseases in european countries: a systematic review and individual patient data meta-analysis. Inflammatory bowel diseases. 2014;20(5):936–45. https://doi.org/10.1097/01.MIB.0000442728.74340.fd.
Koutroubakis IE, Ramos-Rivers C, Regueiro M, Koutroumpakis E, Click B, Schoen RE et al. Persistent or Recurrent Anemia Is Associated With Severe and Disabling Inflammatory Bowel Disease. Clinical Gastroenterology and Hepatology : The Official Clinical Practice Journal of the American Gastroenterological Association. 2015;13(10):1760–6. https://doi.org/10.1016/j.cgh.2015.03.029.
Guo K, Ren J, Li G, Hu Q, Wu X, Wang Z et al. Risk factors of surgical site infections in patients with Crohn's disease complicated with gastrointestinal fistula. International journal of colorectal disease. 2017;32(5):635–43. https://doi.org/10.1007/s00384-017-2751-6.
Yang SS, Yu CS, Yoon YS, Yoon SN, Lim SB, Kim JC. Risk factors for complications after bowel surgery in Korean patients with Crohn's disease. Journal of the Korean Surgical Society. 2012;83(3):141–8. https://doi.org/10.4174/jkss.2012.83.3.141.
Morar PS, Hodgkinson JD, Thalayasingam S, Koysombat K, Purcell M, Hart AL et al. Determining Predictors for Intra-abdominal Septic Complications Following Ileocolonic Resection for Crohn's Disease-Considerations in Pre-operative and Peri-operative Optimisation Techniques to Improve Outcome. Journal of Crohn's & Colitis. 2015;9(6):483–91. https://doi.org/10.1093/ecco-jcc/jjv051.
Kulaylat AN, Hollenbeak CS, Sangster W, Stewart DB, Sr. Impact of smoking on the surgical outcome of Crohn's disease: a propensity-score matched National Surgical Quality Improvement Program analysis. Colorectal Disease: The Official Journal of the Association of Coloproctology of Great Britain and Ireland. 2015;17(10):891–902. https://doi.org/10.1111/codi.12958.
Sharma A, Deeb AP, Iannuzzi JC, Rickles AS, Monson JR, Fleming FJ. Tobacco smoking and postoperative outcomes after colorectal surgery. Annals of Surgery. 2013;258(2):296–300. https://doi.org/10.1097/SLA.0b013e3182708cc5.
Barker K, Graham NG, Mason MC, De Dombal FT, Goligher JC. The relative significance of preoperative oral antibiotics, mechanical bowel preparation, and preoperative peritoneal contamination in the avoidance of sepsis after radical surgery for ulcerative colitis and Crohn's disease of the large bowel. The British Journal Of Surgery. 1971;58(4):270–3.
Alavi K, Sturrock PR, Sweeney WB, Maykel JA, Cervera-Servin JA, Tseng J et al. A simple risk score for predicting surgical site infections in inflammatory bowel disease. Diseases of the Colon and Rectum. 2010;53(11):1480–6. https://doi.org/10.1007/DCR.0b013e3181f1f0fd.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conception or design of the project; assisted with the acquisition, analysis, or interpretation of data; drafted and/or revised the manuscript; and had final approval of the version to be published. All the authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity may be resolved.
Corresponding author
Ethics declarations
Conflicts of Interest and Source of Funding
The authors have no conflicts of interest including relevant financial interests, activities, relationships, and affiliations.
State
The preliminary results of the study were presented as poster at the American Society of Colon and Rectal Surgery Annual Scientific Meeting, June 10–14, 2017, Seattle, WA.
Rights and permissions
About this article
Cite this article
Aydinli, H.H., Aytac, E., Remzi, F.H. et al. Factors Associated with Short-Term Morbidity in Patients Undergoing Colon Resection for Crohn’s Disease. J Gastrointest Surg 22, 1434–1441 (2018). https://doi.org/10.1007/s11605-018-3763-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3763-4