Abstract
Purpose
Optimal margin size when resecting colorectal liver metastases (CRLM) remains unclear, particularly in the setting of perioperative chemotherapy. We evaluated the prognostic significance of margin size in patients who received neoadjuvant FOLFOX and/or FOLFIRI prior to resection of CRLM.
Methods
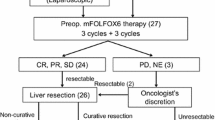
Clinicopathologic factors were collected for patients who underwent curative liver resections for CRLM between 4/2004–1/2016 and received neoadjuvant oxaliplatin and/or irinotecan and 5-FU (FOLFOX, FOLFIRI). Margins were categorized as < 1, ≥ 1–< 5, ≥ 5–< 10, or ≥ 10 mm and evaluated for association with overall survival (OS) and disease-free survival (DFS) by Cox multiple regression analysis. Margin status was classified as positive (< 1 mm) or negative (≥ 1 mm) and similarly evaluated.
Results
Of 227 patients, the median age was 58 years and most had synchronous (80%) lesions. The majority had colon cancers (75%). Margin sizes were 13% < 1 mm, 27% ≥ 1–< 5 mm, 23% ≥ 5–< 10 mm, 36% ≥ 10 mm. Most (63%) received chemotherapy post-liver resection. Five-year OS and DFS were 54% (95% CI 46–62%) and 22% (95% CI 16–28%), respectively. Positive margins significantly increased the risk of death without post-liver resection chemotherapy (HR = 3.32, p = 0.0077), but not with post-liver resection chemotherapy (HR = 1.00, p = 0.99). Negative margin sizes of ≥ 1–< 5, ≥ 5–< 10, and ≥ 10 mm were not significant predictors of OS (p > 0.05).
Conclusion
Patients undergoing liver resection for CRLM should receive post-resection chemotherapy if negative margins (≥ 1 mm) cannot be achieved. For patients receiving FOLFOX and/or FOLFIRI chemotherapy, wider margins did not improve OS.


Similar content being viewed by others
References
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA: a cancer journal for clinicians. 2014;64(1):9–29. https://doi.org/10.3322/caac.21208.
Fong Y, Kemeny N, Paty P, Blumgart LH, Cohen AM. Treatment of colorectal cancer: hepatic metastasis. Seminars in surgical oncology. 1996;12(4):219–52. https://doi.org/10.1002/(SICI)1098-2388(199607/08)12:4<219::AID-SSU3>3.0.CO;2-8.
Kemeny N. Management of liver metastases from colorectal cancer. Oncology (Williston Park). 2006;20(10):1161–76, 79; discussion 79-80, 85-6.
Adam R. Chemotherapy and surgery: new perspectives on the treatment of unresectable liver metastases. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2003;14 Suppl 2:ii13–6.
Brouquet A, Mortenson MM, Vauthey JN, Rodriguez-Bigas MA, Overman MJ, Chang GJ et al. Surgical strategies for synchronous colorectal liver metastases in 156 consecutive patients: classic, combined or reverse strategy? Journal of the American College of Surgeons. 2010;210(6):934–41. https://doi.org/10.1016/j.jamcollsurg.2010.02.039.
Brouquet A, Abdalla EK, Kopetz S, Garrett CR, Overman MJ, Eng C et al. High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(8):1083–90. https://doi.org/10.1200/JCO.2010.32.6132.
Andreou A, Aloia TA, Brouquet A, Dickson PV, Zimmitti G, Maru DM et al. Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Annals of surgery. 2013;257(6):1079–88. https://doi.org/10.1097/SLA.0b013e318283a4d1.
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Annals of surgery. 2004;239(6):818–25; discussion 25-7.
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009;27(22):3677–83. https://doi.org/10.1200/JCO.2008.20.5278.
de Haas RJ, Wicherts DA, Andreani P, Pascal G, Saliba F, Ichai P et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Annals of surgery. 2011;253(6):1069–79. https://doi.org/10.1097/SLA.0b013e318217e898.
Nordlinger B, Benoist S. [Liver metastases from colorectal cancer: a multidisciplinary approach is necessary]. Bulletin de l'Academie nationale de medecine. 2008;192(1):33–43; discussion 4.
Altendorf-Hofmann A, Scheele J. A critical review of the major indicators of prognosis after resection of hepatic metastases from colorectal carcinoma. Surgical oncology clinics of North America. 2003;12(1):165–92, xi.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Annals of surgery. 2005;241(5):715–22, discussion 22-4.
Figueras J, Burdio F, Ramos E, Torras J, Llado L, Lopez-Ben S et al. Effect of subcentimeter nonpositive resection margin on hepatic recurrence in patients undergoing hepatectomy for colorectal liver metastases. Evidences from 663 liver resections. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2007;18(7):1190–5. https://doi.org/10.1093/annonc/mdm106.
Are C, Gonen M, Zazzali K, Dematteo RP, Jarnagin WR, Fong Y et al. The impact of margins on outcome after hepatic resection for colorectal metastasis. Annals of surgery. 2007;246(2):295–300. https://doi.org/10.1097/SLA.0b013e31811ea962.
Elias D, Lasser P, Rougier P, Ducreux M, Bognel C, Roche A. Frequency, technical aspects, results, and indications of major hepatectomy after prolonged intra-arterial hepatic chemotherapy for initially unresectable hepatic tumors. Journal of the American College of Surgeons. 1995;180(2):213–9.
Liu W, Sun Y, Zhang L, Xing BC. Negative surgical margin improved long-term survival of colorectal cancer liver metastases after hepatic resection: a systematic review and meta-analysis. International journal of colorectal disease. 2015;30(10):1365–73. https://doi.org/10.1007/s00384-015-2323-6.
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371(9617):1007–16. https://doi.org/10.1016/S0140-6736(08)60455-9.
Nordlinger B, Van Cutsem E, Rougier P, Kohne CH, Ychou M, Sobrero A et al. Does chemotherapy prior to liver resection increase the potential for cure in patients with metastatic colorectal cancer? A report from the European Colorectal Metastases Treatment Group. European journal of cancer. 2007;43(14):2037–45. https://doi.org/10.1016/j.ejca.2007.07.017.
Van Cutsem E, Nordlinger B, Adam R, Kohne CH, Pozzo C, Poston G et al. Towards a pan-European consensus on the treatment of patients with colorectal liver metastases. European journal of cancer. 2006;42(14):2212–21. https://doi.org/10.1016/j.ejca.2006.04.012.
Engstrom PF, Arnoletti JP, Benson AB, 3rd, Chen YJ, Choti MA, Cooper HS et al. NCCN Clinical Practice Guidelines in Oncology: colon cancer. Journal of the National Comprehensive Cancer Network : JNCCN. 2009;7(8):778–831.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Annals of surgery. 1999;230(3):309–18; discussion 18-21.
Holm S. A Simple Sequentially Rejective Multiple Test Procedure. Scand J Statist. 1979;6:65–70.
Therneau T. A Package for Survival Analysis in S. version 2.38. 2015. https://CRAN.R-project.org/package=survival.
R Core Team: R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2017. https://www.R-project.org/.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of surgery. 2004;240(2):205–13.
Ekberg H, Tranberg KG, Andersson R, Lundstedt C, Hagerstrand I, Ranstam J et al. Determinants of survival in liver resection for colorectal secondaries. The British journal of surgery. 1986;73(9):727–31.
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77(7):1254–62.
Cady B, Jenkins RL, Steele GD, Jr., Lewis WD, Stone MD, McDermott WV et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Annals of surgery. 1998;227(4):566–71.
Elias D, Cavalcanti A, Sabourin JC, Lassau N, Pignon JP, Ducreux M et al. Resection of liver metastases from colorectal cancer: the real impact of the surgical margin. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 1998;24(3):174–9.
Sadot E, Groot Koerkamp B, Leal JN, Shia J, Gonen M, Allen PJ et al. Resection margin and survival in 2368 patients undergoing hepatic resection for metastatic colorectal cancer: surgical technique or biologic surrogate? Annals of surgery. 2015;262(3):476–85; discussion 83-5. https://doi.org/10.1097/SLA.0000000000001427.
Tanaka K, Nojiri K, Kumamoto T, Takeda K, Endo I. R1 resection for aggressive or advanced colorectal liver metastases is justified in combination with effective prehepatectomy chemotherapy. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2011;37(4):336–43. https://doi.org/10.1016/j.ejso.2011.01.007.
Ayez N, Lalmahomed ZS, Eggermont AM, Ijzermans JN, de Jonge J, van Montfort K et al. Outcome of microscopic incomplete resection (R1) of colorectal liver metastases in the era of neoadjuvant chemotherapy. Annals of surgical oncology. 2012;19(5):1618–27. https://doi.org/10.1245/s10434-011-2114-4.
Laurent C, Adam JP, Denost Q, Smith D, Saric J, Chiche L. Significance of R1 Resection for Advanced Colorectal Liver Metastases in the Era of Modern Effective Chemotherapy. World journal of surgery. 2016;40(5):1191–9. https://doi.org/10.1007/s00268-016-3404-6.
Hamady ZZ, Cameron IC, Wyatt J, Prasad RK, Toogood GJ, Lodge JP. Resection margin in patients undergoing hepatectomy for colorectal liver metastasis: a critical appraisal of the 1cm rule. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2006;32(5):557–63. https://doi.org/10.1016/j.ejso.2006.02.001.
Wakai T, Shirai Y, Sakata J, Valera VA, Korita PV, Akazawa K et al. Appraisal of 1 cm hepatectomy margins for intrahepatic micrometastases in patients with colorectal carcinoma liver metastasis. Annals of surgical oncology. 2008;15(9):2472–81. https://doi.org/10.1245/s10434-008-0023-y.
Bodingbauer M, Tamandl D, Schmid K, Plank C, Schima W, Gruenberger T. Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. The British journal of surgery. 2007;94(9):1133–8. https://doi.org/10.1002/bjs.5762.
Muratore A, Ribero D, Zimmitti G, Mellano A, Langella S, Capussotti L. Resection margin and recurrence-free survival after liver resection of colorectal metastases. Annals of surgical oncology. 2010;17(5):1324–9. https://doi.org/10.1245/s10434-009-0770-4.
Konopke R, Kersting S, Makowiec F, Gassmann P, Kuhlisch E, Senninger N et al. Resection of colorectal liver metastases: is a resection margin of 3 mm enough? : a multicenter analysis of the GAST Study Group. World journal of surgery. 2008;32(9):2047–56. https://doi.org/10.1007/s00268-008-9629-2.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND participated in drafting the work or revising it critically for important intellectual content; AND provided final approval of the version to be published; AND agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Miller, C.L., Taylor, M.S., Qadan, M. et al. Prognostic Significance of Surgical Margin Size After Neoadjuvant FOLFOX and/or FOLFIRI for Colorectal Liver Metastases. J Gastrointest Surg 21, 1831–1840 (2017). https://doi.org/10.1007/s11605-017-3557-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3557-0