Abstract
Background
Intrahepatic cholangiocarcinoma (ICC) is an aggressive primary tumor of the liver. While surgery remains the cornerstone of therapy, long-term survival following curative-intent resection is generally poor. The aim of the current study was to define the incidence of actual long-term survivors, as well as identify clinicopathological factors associated with long-term survival.
Methods
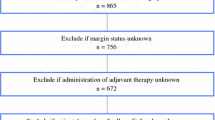
Patients who underwent a curative-intent liver resection for ICC between 1990 and 2015 were identified using a multi-institutional database. Overall, 679 patients were alive with ≥ 5 years of follow-up or had died during follow-up. Prognostic factors among patients who were long-term survivors (LT) (overall survival (OS) ≥ 5) were compared with patients who were not non-long-term survivors (non-LT) (OS < 5).
Results
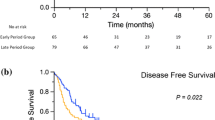
Among the 1154 patients who underwent liver resection for ICC, 5- and 10-year OS were 39.6 and 20.3% while the actual LT survival rate was 13.3%. After excluding 475 patients who survived < 5 years, as well as patients were alive yet had < 5 years of follow-up, 153 patients (22.5%) who survived ≥ 5 years were included in the LT group, while 526 patients (77.5%) who died < 5 years from the date of surgery were included in the non-LT group. Factors associated with not surviving to 5 years included perineural invasion (OR 4.78, 95% CI, 1.92–11.8; p = 0.001), intrahepatic metastasis (OR 3.75, 95% CI, 0.85–16.6, p = 0.082), satellite lesions (OR 2.12, 95% CI, 1.15–3.90, p = 0.016), N1 status (OR 4.64, 95% CI, 1.77–12.2; p = 0.002), ICC > 5 cm (OR 2.40, 95% CI, 1.54–3.74, p < 0.001), and direct invasion of an adjacent organ (OR 3.98, 95% CI, 1.18–13.4, p = 0.026). However, a subset of patients (< 10%) who had these pathological characteristics were LT.
Conclusion
While ICC is generally associated with a poor prognosis, some patients will be LT. In fact, even a subset of patients with traditional adverse prognostic factors survived long term.


Similar content being viewed by others
References
El-Serag HB, Engels EA, Landgren O, Chiao E, Henderson L, Amaratunge HC et al. Risk of hepatobiliary and pancreatic cancers after hepatitis C virus infection: a population-based study of U.S. veterans. Hepatology. 2009;49(1):116–23. https://doi.org/10.1002/hep.22606.
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Annals of Surgery. 2008; 248(1):84–96. https://doi.org/10.1097/SLA.0b013e318176c4d3.
Malhi H, Gores GJ. Cholangiocarcinoma: modern advances in understanding a deadly old disease. Journal of Hepatology. 2006; 45(6):856–67. https://doi.org/10.1016/j.jhep.2006.09.001.
Shaib YH, Davila JA, McGlynn K, El-Serag HB. Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? Journal of Hepatology. 2004; 40(3):472–7. https://doi.org/10.1016/j.jhep.2003.11.030.
Welzel TM, McGlynn KA, Hsing AW, O’Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. Journal of the National Cancer Institute. 2006; 98(12):873–5. https://doi.org/10.1093/jnci/djj234.
Khan SA, Toledano MB, Taylor-Robinson SD. Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB: the Official Journal of the International Hepato Pancreato Biliary Association. 2008; 10(2):77–82. https://doi.org/10.1080/13651820801992641.
Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surgery. 2014. https://doi.org/10.1001/jamasurg.2013.5137.
Amin MB EiC, American Joint Committee on Cancer. Springer. 2017.
Hyder O, Marques H, Pulitano C, Marsh JW, Alexandrescu S, Bauer TW et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an Eastern and Western experience. JAMA Surgery. 2014. https://doi.org/10.1001/jamasurg.2013.5168.
Amini N, Ejaz A, Spolverato G, Maithel SK, Kim Y, Pawlik TM. Management of lymph nodes during resection of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: a systematic review. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2014; 18(12):2136–48. https://doi.org/10.1007/s11605-014-2667-1.
Bagante F, Gani F, Spolverato G, Xu L, Alexandrescu S, Marques HP et al. Intrahepatic cholangiocarcinoma: prognosis of patients who did not undergo lymphadenectomy. Journal of the American College of Surgeons. 2015; 221(6):1031–40 e4. https://doi.org/10.1016/j.jamcollsurg.2015.09.012.
Kim Y, Spolverato G, Amini N, Margonis GA, Gupta R, Ejaz A et al. Surgical Management of intrahepatic cholangiocarcinoma: defining an optimal prognostic lymph node stratification schema. Annals of Surgical Oncology. 2015; 22(8):2772–8. https://doi.org/10.1245/s10434-015-4419-1.
Spolverato G, Ejaz A, Kim Y, Sotiropoulos GC, Pau A, Alexandrescu S et al. Tumor size predicts vascular invasion and histologic grade among patients undergoing resection of intrahepatic cholangiocarcinoma. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2014; 18(7):1284–91. https://doi.org/10.1007/s11605-014-2533-1.
Spolverato G, Kim Y, Ejaz A, Alexandrescu S, Marques H, Aldrighetti L et al. Conditional probability of long-term survival after liver resection for intrahepatic cholangiocarcinoma: a multi-institutional analysis of 535 patients. JAMA Surgery. 2015; 150(6):538–45. https://doi.org/10.1001/jamasurg.2015.0219.
Spolverato G, Vitale A, Cucchetti A, Popescu I, Marques HP, Aldrighetti L et al. Can hepatic resection provide a long-term cure for patients with intrahepatic cholangiocarcinoma? Cancer. 2015; 121(22):3998–4006. https://doi.org/10.1002/cncr.29619.
Spolverato G, Yakoob MY, Kim Y, Alexandrescu S, Marques HP, Lamelas J et al. The impact of surgical margin status on long-term outcome after resection for intrahepatic cholangiocarcinoma. Annals of Surgical Oncology. 2015. https://doi.org/10.1245/s10434-015-4472-9.
Spolverato G, Yakoob MY, Kim Y, Alexandrescu S, Marques HP, Lamelas J et al. Impact of complications on long-term survival after resection of intrahepatic cholangiocarcinoma. Cancer. 2015; 121(16):2730–9. https://doi.org/10.1002/cncr.29419.
Spolverato G BF, Weiss, M, Alexandrescu S, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Koerkamp BG, Guglielmi A, Itaru E, Pawlik TM. Comparative performances of the 7th and the 8th editions of the American Joint Committee on Cancer Staging Systems for intrahepatic cholangiocarcinoma. Journal of Surgical Oncology.
Ronnekleiv-Kelly SM, Pawlik TM. Staging of intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr. 2017; 6(1):35–43. https://doi.org/10.21037/hbsn.2016.10.02.
Ferrone CR, Brennan MF, Gonen M, Coit DG, Fong Y, Chung S et al. Pancreatic adenocarcinoma: the actual 5-year survivors. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2008; 12(4):701–6. https://doi.org/10.1007/s11605-007-0384-8.
Zheng J, Kuk D, Gonen M, Balachandran VP, Kingham TP, Allen PJ et al. Actual 10-year survivors after resection of hepatocellular carcinoma. Annals of Surgical Oncology. 2017; 24(5):1358–66. https://doi.org/10.1245/s10434-016-5713-2.
Baheti AD, Tirumani SH, Shinagare AB, Rosenthal MH, Hornick JL, Ramaiya NH et al. Correlation of CT patterns of primary intrahepatic cholangiocarcinoma at the time of presentation with the metastatic spread and clinical outcomes: retrospective study of 92 patients. Abdominal Imaging. 2014; 39(6):1193–201. https://doi.org/10.1007/s00261-014-0167-0.
De Jong MC, Nathan H, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2011; 29(23):3140–5. https://doi.org/10.1200/jco.2011.35.6519.
Dodson RM, Weiss MJ, Cosgrove D, Herman JM, Kamel I, Anders R et al. Intrahepatic cholangiocarcinoma: management options and emerging therapies. Journal of the American College of Surgeons. 2013; 217(4):736–50e4. https://doi.org/10.1016/j.jamcollsurg.2013.05.021.
de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Annals of Surgery. 2009; 250(3):440–8. https://doi.org/10.1097/SLA.0b013e3181b4539b.
Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD et al. A proposed staging system for intrahepatic cholangiocarcinoma. Annals of Surgical Oncology. 2009; 16(1):14–22. https://doi.org/10.1245/s10434-008-0180-z.
Spolverato G, Kim Y, Alexandrescu S, Popescu I, Marques HP, Aldrighetti L et al. Is hepatic resection for large or multifocal intrahepatic cholangiocarcinoma justified? Results from a multi-institutional collaboration. Annals of Surgical Oncology. 2014. https://doi.org/10.1245/s10434-014-4223-3.
DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Annals of Surgery. 2007; 245(5):755–62. https://doi.org/10.1097/01.sla.0000251366.62632.d3.
Nakagohri T, Kinoshita T, Konishi M, Takahashi S, Gotohda N. Surgical outcome and prognostic factors in intrahepatic cholangiocarcinoma. World Journal of Surgery. 2008; 32(12):2675–80. https://doi.org/10.1007/s00268-008-9778-3.
Hatzaras I, Schmidt C, Muscarella P, Melvin WS, Ellison EC, Bloomston M. Elevated CA 19-9 portends poor prognosis in patients undergoing resection of biliary malignancies. HPB: the Official Journal of the International Hepato Pancreato Biliary Association. 2010; 12(2):134–8. https://doi.org/10.1111/j.1477-2574.2009.00149.x.
Nathan H, Pawlik TM. Staging of intrahepatic cholangiocarcinoma. Current Opinion in Gastroenterology. 2010; 26(3):269–73. https://doi.org/10.1097/MOG.0b013e328337c899.
Hyder O, Hatzaras I, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H et al. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery. 2013; 153(6):811–8. https://doi.org/10.1016/j.surg.2012.12.005.
Bollschweiler E. Benefits and limitations of Kaplan-Meier calculations of survival chance in cancer surgery. Langenbeck’s Archives of Surgery/Deutsche Gesellschaft fur Chirurgie. 2003; 388(4):239–44. https://doi.org/10.1007/s00423-003-0410-6.
Bagante F, Spolverato G, Merath K, Postlewait LM, Poultsides GA, Mullen MG et al. Neuroendocrine liver metastasis: the chance to be cured after liver surgery. J Surg Oncol. 2017. https://doi.org/10.1002/jso.24563.
Spolverato G, Bagante F, Ethun CG, Poultsides G, Tran T, Idrees K et al. Defining the chance of statistical cure among patients with extrahepatic biliary tract cancer. World J Surg. 2017; 41(1):224–31. https://doi.org/10.1007/s00268-016-3691-y.
Bagante F, Spolverato G, Weiss M, Alexandrescu S, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Koerkamp BG, Guglielmi A, Itaru E, Pawlik TM. Impact of morphological status on long-term outcome among patients undergoing liver surgery for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2017; 24:2491–2501.
Adachi T, Eguchi S. Lymph node dissection for intrahepatic cholangiocarcinoma: a critical review of the literature to date. Journal of Hepato-Biliary-Pancreatic Sciences. 2014; 21(3):162–8. https://doi.org/10.1002/jhbp.30.
Ribero D, Pinna AD, Guglielmi A, Ponti A, Nuzzo G, Giulini SM et al. Surgical approach for long-term survival of patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis of 434 patients. Archives of Surgery. 2012; 147(12):1107–13.
Ercolani G, Vetrone G, Grazi GL, Aramaki O, Cescon M, Ravaioli M et al. Intrahepatic cholangiocarcinoma: primary liver resection and aggressive multimodal treatment of recurrence significantly prolong survival. Annals of Surgery. 2010; 252(1):107–14. https://doi.org/10.1097/SLA.0b013e3181e462e6.
Saxena A, Chua T, Sarkar A, Chu F, Morris D. Clinicopathologic and treatment-related factors influencing recurrence and survival after hepatic resection of intrahepatic cholangiocarcinoma: a 19-year experience from an established Australian Hepatobiliary Unit. Journal of Gastrointestinal Surgery. 2010; 14(7):1128–38. https://doi.org/10.1007/s11605-010-1203-1.
Guglielmi A, Ruzzenente A, Campagnaro T, Pachera S, Valdegamberi A, Nicoli P et al. Intrahepatic cholangiocarcinoma: prognostic factors after surgical resection. World Journal of Surgery. 2009; 33(6):1247–54. https://doi.org/10.1007/s00268-009-9970-0.
Yedibela S, Demir R, Zhang W, Meyer T, Hohenberger W, Schonleben F. Surgical treatment of mass-forming intrahepatic cholangiocarcinoma: an 11-year western single-center experience in 107 patients. Annals of Surgical Oncology. 2009; 16(2):404–12.
Uenishi T, Kubo S, Yamazaki O, Yamada T, Sasaki Y, Nagano H et al. Indications for surgical treatment of intrahepatic cholangiocarcinoma with lymph node metastases. Journal of Hepato-Biliary-Pancreatic Surgery. 2008; 15(4):417–22. https://doi.org/10.1007/s00534-007-1315-5.
Yamashita Y, Taketomi A, Morita K, Fukuhara T, Ueda S, Sanefuji K et al. The impact of surgical treatment and poor prognostic factors for patients with intrahepatic cholangiocarcinoma: retrospective analysis of 60 patients. Anticancer Research. 2008; 28(4C):2353–9.
Rama R, Swaminathan R, Venkatesan P. Cure models for estimating hospital-based breast cancer survival. Asian Pac J Cancer Prev. 2010; 11(2):387–91.
Rasouli M, Ghadimi MR, Mahmoodi M, Mohammad K, Zeraati H, Hosseini M. Survival analysis of patients with esophageal cancer using parametric cure model. Asian Pac J Cancer Prev. 2011; 12(9):2359–63.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as an Oral Presentation at the Annual Americas Hepato-Pancreato-Biliary Association Meeting, Miami, FL 2017.
Rights and permissions
About this article
Cite this article
Bagante, F., Spolverato, G., Weiss, M. et al. Defining Long-Term Survivors Following Resection of Intrahepatic Cholangiocarcinoma. J Gastrointest Surg 21, 1888–1897 (2017). https://doi.org/10.1007/s11605-017-3550-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3550-7