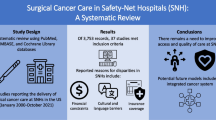
Abstract
Background
Due to disparities in access to care, patients with Medicaid or no health insurance are at risk of not receiving appropriate adjuvant treatment following resection of pancreatic cancer. We have previously shown inferior short-term outcomes following surgery at safety-net hospitals. Subsequently, we hypothesized that safety-net hospitals caring for these vulnerable populations utilize less adjuvant chemoradiation, resulting in inferior long-term outcomes.
Methods
The American College of Surgeons National Cancer Data Base was queried for patients diagnosed with pancreatic adenocarcinoma (n = 32,296) from 1998 to 2010. Hospitals were grouped according to safety-net burden, defined as the proportion of patients with Medicaid or no insurance. The highest quartile, representing safety-net hospitals, was compared to lower-burden hospitals with regard to patient demographics, disease characteristics, surgical management, delivery of multimodal systemic therapy, and survival.
Results
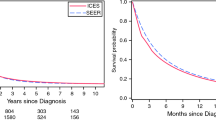
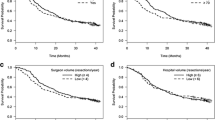
Patients at safety-net hospitals were less often white, had lower income, and were less educated. Safety-net hospital patients were just as likely to undergo surgical resection (OR 1.03, p = 0.73), achieving similar rates of negative surgical margins when compared to patients at medium and low burden hospitals (70% vs. 73% vs. 66%). Thirty-day mortality rates were 5.6% for high burden hospitals, 5.2% for medium burden hospitals, and 4.3% for low burden hospitals. No clinically significant differences were noted in the proportion of surgical patients receiving either chemotherapy (48% vs. 52% vs. 52%) or radiation therapy (26% vs. 30% vs. 29%) or the time between diagnosis and start of systemic therapy (58 days vs. 61 days vs. 53 days). Across safety-net burden groups, no difference was noted in stage-specific median survival (all p > 0.05) or receipt of adjuvant as opposed to neoadjuvant systemic therapy (82% vs. 85% vs. 85%). Multivariate analysis adjusting for cancer stage revealed no difference in survival for safety-net hospital patients who had surgery and survived > 30 days (HR 1.02, p = 0.63).
Conclusion
For patients surviving the perioperative setting following pancreatic cancer surgery, safety-net hospitals achieve equivalent long-term survival outcomes potentially due to equivalent delivery of multimodal therapy at non-safety-net hospitals. Safety-net hospitals are a crucial resource that provides quality long-term cancer treatment for vulnerable populations.
Similar content being viewed by others
References
American Cancer Society. Cancer Facts & Figures 2016. Atlanta: American Cancer Society; 2016:1–9.
Ghaneh P, Costello E, Neoptolemos JP. Biology and management of pancreatic cancer. Postgraduate medical journal. 2008;84:478–97.
Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. Pancreatic cancer. The Lancet. 2011;378:607–20.
Katz MHG, Shi Q, Ahmad SA, Herman JM, Marsh RDW, Collisson E, et al. Preoperative Modified FOLFIRINOX Treatment Followed by Capecitabine-Based Chemoradiation for Borderline Resectable Pancreatic Cancer: Alliance for Clinical Trials in Oncology Trial A021101. JAMA surgery. 2016;151:e161137.
Regine WF, Winter KA, Abrams RA, Safran H, Hoffman JP, Konski A, et al. Fluorouracil vs Gemcitabine Chemotherapy Before and After Fluorouracil-Based Chemoradiation Following Resection of Pancreatic Adenocarcinoma A Randomized Controlled Trial. Jama. 2008;299:1019–27.
Khorana AA, Mangu PB, Berlin J, Engebretson A, Hong TS, Maitra A, et al. Potentially curable pancreatic cancer: American society of clinical oncology clinical practice guideline. Journal of Clinical Oncology. 2016;34:2541–56.
In: Ein Lewin M, Altman S, editors. Americas’s Health Care Safety Net: Intact but Endangered. Washington (DC) 2000.
Go DE, Abbott DE, Wima K, Hanseman DJ, Ertel AE, Chang AL, et al. Addressing the High Costs of Pancreaticoduodenectomy at Safety-Net Hospitals. JAMA Surg. 2016;151(10):908–14.
Hoehn RS, Wima K, Vestal MA, Weilage DJ, Hanseman DJ, Abbott DE, et al. Effect of Hospital Safety-Net Burden on Cost and Outcomes After Surgery. JAMA Surgery. 2015;0558:1.
Gagliardi AR, Soong D, Gallinger S. Identifying Factors Influencing Pancreatic Cancer Management to Inform Quality Improvement Efforts and Future Research: A Scoping Systematic Review. Pancreas. 2016;45(2):161–6.
Harlan LC, Ph D. Original Article Racial/Ethnic Patterns of Care for Pancreatic Cancer 1 1. Journal of Palliative Medicine. 2009;12.
Blanco BA, Kothari AN, Blackwell RH, Brownlee SA, Yau RM, Attisha JP, et al. “Take the Volume Pledge” may result in disparity in access to care. Surgery. 2016:1–9.
Schwartz DM, Fong ZV, Warshaw AL, Zinner MJ, Chang DC. The Hidden Consequences of the Volume Pledge. Annals of Surgery. 2016;XX:1.
Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–3.
Rajaram R, Chung JW, Kinnier CV, Barnard C, Mohanty S, Pavey ES, et al. Hospital Characteristics Associated With Penalties in the Centers for Medicare & Medicaid Services Hospital-Acquired Condition Reduction Program. Jama. 2015;314:375–83.
Amarasingham R, Moore BJ, Tabak YP, Drazner MH, Clark CA, Zhang S, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–8.
Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48(4):495–504.
Macht R, McAneny D, Doherty G. Challenges in Surgical Quality at Safety-Net Hospitals. JAMA Surg. 2016;151(9):795–6.
McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL. Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transplant. 2012;12(12):3283–8.
Mouch CA, Regenbogen SE, Revels SL, Wong SL, Lemak CH, Morris AM. The quality of surgical care in safety net hospitals: a systematic review. Surgery. 2014;155(5):826–38.
Quillin RC, 3rd, Wilson GC, Wima K, Hohmann SF, Sutton JM, Shaw JJ, et al. Neighborhood level effects of socioeconomic status on liver transplant selection and recipient survival. Clin Gastroenterol Hepatol. 2014;12(11):1934–41.
Wakeam E, Hevelone ND, Maine R, Swain J, Lipsitz SA, Finlayson SR, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA Surg. 2014;149(3):229–35.
Wilson GC, Cutler Quillin R, 3rd, Sutton JM, Wima K, Shaw JJ, Hoehn RS, et al. Factors related to readmission after major elective surgery. Dig Dis Sci. 2015;60(1):47–53.
Bazzoli GJ, Chen HF, Zhao M, Lindrooth RC. Hospital financial condition and the quality of patient care. Health Econ. 2008;17(8):977–95.
Encinosa WE, Bernard DM. Hospital finances and patient safety outcomes. Inquiry. 2005;42(1):60–72.
Lindrooth RC, Konetzka RT, Navathe AS, Zhu J, Chen W, Volpp K. The impact of profitability of hospital admissions on mortality. Health Serv Res. 2013;48(2 Pt 2):792–809.
McHugh M, Martin TC, Orwat J, Dyke KV. Medicare's policy to limit payment for hospital-acquired conditions: the impact on safety net providers. J Health Care Poor Underserved. 2011;22(2):638–47.
Author information
Authors and Affiliations
Contributions
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication before its appearance in the Journal of Gastrointestinal Surgery.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Category 1
Conception and design of study:
Vikrom K Dhar, Richard S Hoehn, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Acquisition of data:
Vikrom K Dhar, Richard S Hoehn, Young Kim, Brent T Xia, Andrew D Jung, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Analysis and/or interpretation of data:
Vikrom K Dhar, Richard S Hoehn, Young Kim, Brent T Xia, Andrew D Jung, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Category 2
Drafting the manuscript:
Vikrom K Dhar, Richard S Hoehn, Syed A Ahmad, Shimul A Shah.
Revising the manuscript critically for important intellectual content:
Vikrom K Dhar, Richard S Hoehn, Young Kim, Brent T Xia, Andrew D Jung, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Category 3
Final approval of the version of the manuscript to be published:
Vikrom K Dhar, Richard S Hoehn, Young Kim, Brent T Xia, Andrew D Jung, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Category 4
Agreement to be accountable for all aspects of the work:
Vikrom K Dhar, Richard S Hoehn, Young Kim, Brent T Xia, Andrew D Jung, Dennis J Hanseman, Syed A Ahmad, Shimul A Shah.
Additional information
Presentation
This manuscript was accepted for presidential plenary presentation at the 2017 Society for Surgery of the Alimentary Tract Annual Meeting in Chicago, IL, held May 6–9, 2017.
Rights and permissions
About this article
Cite this article
Dhar, V.K., Hoehn, R.S., Kim, Y. et al. Equivalent Treatment and Survival after Resection of Pancreatic Cancer at Safety-Net Hospitals. J Gastrointest Surg 22, 98–106 (2018). https://doi.org/10.1007/s11605-017-3549-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3549-0