Abstract
Background
Since biliary variations are commonly seen, our aims are to clarify these insidious variations and discuss their surgicopathologic implications for Bismuth-Corlette (BC) type IV hilar cholangiocarcinoma (HC) applied to hemihepatectomy.
Methods
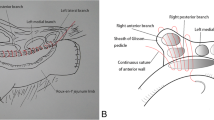
Three-dimensional images of patients with distal bile duct obstruction (n = 97) and advanced HC (n = 79) were reconstructed and analyzed retrospectively. Normal biliary confluence pattern was defined as the peripheral segment IV duct (B4) joining the common trunk of segment II (B2) and segment III (B3) ducts to form the left hepatic duct (LHD) that then joined the right hepatic duct (RHD). The lengths from left and right secondary biliary ramifications to the right side of the umbilical portion of the left portal vein (Rl-L) and the cranio-ventral side of the right portal vein (Rr-R) were measured, respectively, and compared with the resectable bile duct length in HCs. Surgicopathologic findings were compared between different BC types.
Results
The resectable bile duct length in right hemihepatectomy for eradication of type IV tumors was significantly longer than the Rl-L length in normal biliary configuration (17.4 ± 1.8 and 10.3 ± 3.4 mm, respectively, p < 0.001), and type III variation (B2 joining the common trunk of B3 and B4) was the predominant configuration (53.8%). The resectable length in left hemihepatectomy for eradication of type IV tumors was comparable with the Rr-R length in RHD absent cases (15.2 ± 2.5 and 16.4 ± 2.6 mm, respectively, p = 0.177) but significantly longer than that in normal configuration (p < 0.001). The estimated length was 8.5 ± 2.0 mm in unresectable cases. There was no significant difference between type III and IV tumors, except for the rate of nodal metastasis (29.7 and 76.0%, respectively, p < 0.001).
Conclusion
Hemihepatectomy might be selected for curative-intent resection of BC type IV tumors considering the advantageous biliary variations, whereas anatomical trisegmentectomy is recommended for the resectable bile duct length less than 10 mm. Biliary variations might result in excessive classification of BC type IV but require validation on further study.





Similar content being viewed by others
References
Nagino M. Perihilar cholangiocarcinoma: a surgeon’s viewpoint on current topics. J Gastroenterol 2012; 47:1165–1176.
Govil S, Reddy MS, Rela M. Surgical resection techniques for locally advanced hilar cholangiocarcinoma. Langenbecks Arch Surg 2014; 399:707–716.
Ito F, Cho CS, Rikkers LF, Weber SM. Hilar cholangiocarcinoma: current management. Ann Surg 2009; 250:210–218.
Xiang S, Lau WY, Chen XP. Hilar cholangiocarcinoma: controversies on the extent of surgical resection aiming at cure. Int J Colorectal Dis 2015; 30:159–171.
Poruk KE, Pawlik TM, Weiss MJ. Perioperative Management of Hilar Cholangiocarcinoma. J Gastrointest Surg 2015; 19:1889–1899.
Croome KP, Rosen CB, Heimbach JK, Nagorney DM. Is Liver Transplantation Appropriate for Patients with Potentially Resectable De Novo HilarCholangiocarcinoma? J Am Coll Surg 2015; 221:130–139.
van Gulik TM, Gouma DJ. Changing perspectives in the assessment of resectability of hilar cholangiocarcinoma. Ann Surg Oncol 2007; 14:1969–1971.
Zeng N, Tao H, Fang C, Fan Y, Xiang N, Yang J, Zhu W, Liu J, Guan T, Fang C, Xiang F. Individualized preoperative planning using three-dimensional modeling for Bismuth and Corlette type III hilarcholangiocarcinoma. World J Surg Oncol 2016; 14:44.
Chaib E, Kanas AF, Galvão FH, D’Albuquerque LA. Bile duct confluence: anatomic variations and its classification. Surg Radiol Anat 2014; 36:105–109.
Lee HY, Kim SH, Lee JM, Kim SW, Jang JY, Han JK, Choi BI. Preoperative assessment of resectability of hepatic hilar cholangiocarcinoma: combined CT andcholangiography with revised criteria. Radiology 2006; 239:113–121.
Kawarada Y, Das BC, Onishi H, Taoka H, Gadzijev EM, Ravnik D, Tabata M, Isaji S. Surgical anatomy of the bile duct branches of the medial segment (B4) of the liver in relation to hilar carcinoma. J Hepatobiliary Pancreat Surg 2000; 7:480–485.
Endo I, Matsuyama R, Mori R, Taniguchi K, Kumamoto T, Takeda K, Tanaka K, Köhn A, Schenk A. Imaging and surgical planning for perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci 2014; 21:525–532.
Hirose T, Igami T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, Mori K, Ando M, Nagino M. Surgical and Radiological Studies on the Length of the Hepatic Ducts. World J Surg 2015; 39:2983–2989.
Endo I, Shimada H, Sugita M, Fujii Y, Morioka D, Takeda K, Sugae S, Tanaka K, Togo S, Bourquain H, Peitgen HO. Role of three-dimensional imaging in operative planning for hilar cholangiocarcinoma. Surgery 2007; 142:666–675.
Furusawa N, Kobayashi A, Yokoyama T, Shimizu A, Motoyama H, Kanai K, Arakura N, Yamada A, Kitou Y, Miyagawa S. Biliary tract variations of the left liver with special reference to the left medial sectional bile duct in 500 patients. Am J Surg 2015; 210:351–356.
Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, Nishio H, Nimura Y. Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg 2004; 239:82–86.
Takeishi K, Shirabe K, Yoshida Y, Tsutsui Y, Kurihara T, Kimura K, Itoh S, Harimoto N, Yamashita YI, Ikegami T, Yoshizumi T, Nishie A, Maehara Y. Correlation between portal vein anatomy and bile duct variation in 407 living liver donors. Am J Transplant 2015; 15:155–160.
Matsumoto N, Ebata T, Yokoyama Y, Igami T, Sugawara G, Shimoyama Y, Nagino M. Role of anatomical right hepatic trisectionectomy for perihilar cholangiocarcinoma. Br J Surg 2014; 101:261–268.
Hosokawa I, Shimizu H, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Miyazaki M. Surgical strategy for hilar cholangiocarcinoma of the left-side predominance: current role of lefttrisectionectomy. Ann Surg 2014; 259:1178–1185.
Ebata T, Watanabe H, Ajioka Y, Oda K, Nimura Y. Pathological appraisal of lines of resection for bile duct carcinoma. Br J Surg 2002; 89:1260–1267.
Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, Seehofer D. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol 2012; 19:1602–1608.
Hu HJ, Mao H, Shrestha A, Tan YQ, Ma WJ, Yang Q, Wang JK, Cheng NS, Li FY. Prognostic factors and long-term outcomes of hilar cholangiocarcinoma: A single-institution experience in China. World J Gastroenterol 2016; 22:2601–2610.
Ebata T, Kosuge T, Hirano S, Unno M, Yamamoto M, Miyazaki M, Kokudo N, Miyagawa S, Takada T, Nagino M. Proposal to modify the International Union Against Cancer staging system for perihilar cholangiocarcinomas. Br J Surg 2014; 101:79–88.
Popescu I, Dumitrascu T. Curative-intent surgery for hilar cholangiocarcinoma: prognostic factors for clinical decision making. Langenbecks Arch Surg 2014; 399:693–705.
Higuchi R, Yamamoto M. Indications for portal vein embolization in perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci 2014; 21:542–549.
Hwang S, Ko GY, Kim MH, Lee SK, Gwon DI, Ha TY, Song GW, Jung DH, Park DH, Lee SS. Preoperative Left Portal Vein Embolization for Left Liver Resection in High-Risk Hepatobiliary Malignancy Patients. World J Surg 2016; 40:2758–2765.
Mansour JC, Aloia TA, Crane CH, Heimbach JK, Nagino M, Vauthey JN. Hilar cholangiocarcinoma: expert consensus statement. HPB (Oxford) 2015; 17:691–699.
Izbicki JR, Tsui TY, Bohn BA, Bockhorn M. Surgical strategies in patients with advanced hilar cholangiocarcinoma (Klatskin tumor). J Gastrointest Surg 2013; 17:581–585.
Sotiropoulos GC, Lang H, Molmenti EP, Kaiser GM, Paul A, Broelsch CE. Partial or complete mesohepatectomy combined with resection of the hilar bifurcation in cases of Klatskin tumors: a reasonable strategy? Am J Surg 2009; 198:297–298.
La Greca G, Racalbuto A, Puleo S, Licata A. Favourable anatomical variation for the resection of a Klatskin tumour. Eur J Surg Oncol 1996; 22:97–101.
Ni Q, Wang H, Liang X, Zhang Y, Chen W, Wang J. Successful Parenchyma-Sparing Anatomical Surgery by 3-Dimensional Reconstruction of HilarCholangiocarcinoma Combined with Anatomic Variation. J Coll Physicians Surg Pak 2016; 26:S13-15.
Giuliante F, Ardito F, Guglielmi A, Aldrighetti L, Ferrero A, Calise F, Giulini SM, Jovine E, Breccia C, De Rose AM, Pinna AD, Nuzzo G. Association of Lymph Node Status With Survival in Patients After Liver Resection for HilarCholangiocarcinoma in an Italian Multicenter Analysis. JAMA Surg 2016; 151:916–922.
Acknowledgments
This study is supported by the China Postdoctoral Science Foundation (2015M581837).
Authors’ Contribution
Gu-wei Ji drafted the paper and Fei-peng Zhu was responsible for radiological evaluation. Ke Wang, Chen-yu Jiao, and Zi-cheng Shao conducted the data analysis. The corresponding author, Xiang-cheng Li, designed the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Gu-wei Ji and Fei-peng Zhu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ji, Gw., Zhu, Fp., Wang, K. et al. Clinical Implications of Biliary Confluence Pattern for Bismuth-Corlette Type IV Hilar Cholangiocarcinoma Applied to Hemihepatectomy. J Gastrointest Surg 21, 666–675 (2017). https://doi.org/10.1007/s11605-017-3377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3377-2