Abstract
Background
There is a paucity of data demonstrating the effect race and insurance status have on postoperative outcomes for patients with rectal cancer. We evaluated factors impacting short-term outcomes following rectal cancer surgery.
Design
Patients who underwent surgery for rectal cancer using the University Health System Consortium database from 2011 to 2012 were studied. Univariate and multivariable analyses were used to identify patient related risk factors for 30-day outcomes after proctectomy: complication rate, 30-day readmission, ICU stay, and length of hospital stay (LOS).
Results
A total of 9272 proctectomies were identified in this cohort. After adjustment for potential confounders, black patients were more likely to have 30-day readmissions (OR 1.51, 95 % CI 1.26–1.81), ICU stays (OR 1.25, 95 % CI 1.03–1.51), and longer LOS (+1.67 days, 95 % CI 1.21–2.13) when compared to whites. Compared to those with private insurance, patients with public or military insurance or who were self-pay had a higher likelihood of having postoperative complications.
Conclusions
In patients who undergo elective proctectomy for rectal cancer, non-white and non-privately insured status are associated with significantly worse short-term outcomes. Further studies are needed to determine the implications with respect to receipt of adjuvant therapy and survival.
Similar content being viewed by others
References
Robbins AS, Siegel RL, Jemal A. Racial disparities in stage-specific colorectal cancer mortality rates from 1985 to 2008. J Clin Oncol. 2012;30(4):401–5.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29.
Polite BN, Dignam JJ, Olopade OI. Colorectal cancer model of health disparities: understanding mortality differences in minority populations. J Clin Oncol. 2006;24(14):2179–87.
Demissie K, Oluwole OO, Balasubramanian BA, Osinubi OO, August D, Rhoads GG. Racial differences in the treatment of colorectal cancer: a comparison of surgical and radiation therapy between Whites and Blacks. Ann Epidemiol. 2004;14(3):215–21.
Baldwin LM, Dobie SA, Billingsley K, Cai Y, Wright GE, Dominitz JA, et al. Explaining black-white differences in receipt of recommended colon cancer treatment. J Natl Cancer Inst. 2005;97(16):1211–20.
Breslin TM, Morris AM, Gu N, Wong SL, Finlayson EV, Banerjee M, et al. Hospital factors and racial disparities in mortality after surgery for breast and colon cancer. J Clin Oncol. 2009;27(24):3945–50.
Mukamel DB, Murthy AS, Weimer DL. Racial differences in access to high-quality cardiac surgeons. Am J Public Health. 2000;90(11):1774–7.
Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683–91.
Smith JaMC. Health Insurance Coverage in the United States: 2014. In: Bureau UC, ed. Current Population Reports; 2015.
Damle RN, Macomber CW, Flahive JM, Davids JS, Sweeney WB, Sturrock PR, et al. Surgeon volume and elective resection for colon cancer: an analysis of outcomes and use of laparoscopy. J Am Coll Surg. 2014;218(6):1223–30.
Harmon JW, Tang DG, Gordon TA, Bowman HM, Choti MA, Kaufman HS, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg. 1999;230(3):404–11; discussion 11–3.
Schrag D, Panageas KS, Riedel E, Hsieh L, Bach PB, Guillem JG, et al. Surgeon volume compared to hospital volume as a predictor of outcome following primary colon cancer resection. J Surg Oncol. 2003;83(2):68–78; discussion −9.
Tevis SE, Kohlnhofer BM, Stringfield S, Foley EF, Harms BA, Heise CP, et al. Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon Rectum. 2013;56(12):1339–48.
Hendren S, Birkmeyer JD, Yin H, Banerjee M, Sonnenday C, Morris AM. Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer. Dis Colon Rectum. 2010;53(12):1587–93.
Damle RN, Cherng NB, Flahive JM, Davids JS, Maykel JA, Sturrock PR, et al. Clostridium difficile infection after colorectal surgery: a rare but costly complication. J Gastrointest Surg. 2014;18(10):1804–11.
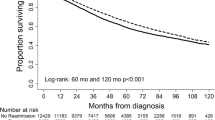
Morris AM, Wei Y, Birkmeyer NJ, Birkmeyer JD. Racial disparities in late survival after rectal cancer surgery. J Am Coll Surg. 2006;203(6):787–94.
Ravi P, Sood A, Schmid M, Abdollah F, Sammon JD, Sun M, et al. Racial/Ethnic Disparities in Perioperative Outcomes of Major Procedures: Results From the National Surgical Quality Improvement Program. Ann Surg. 2015;262(6):955–64.
Parsons HM, Tuttle TM, Kuntz KM, Begun JW, McGovern PM, Virnig BA. Quality of care along the cancer continuum: does receiving adequate lymph node evaluation for colon cancer lead to comprehensive postsurgical care? J Am Coll Surg. 2012;215(3):400–11.
Dagogo-Jack S, Funnell MM, Davidson J. Barriers to achieving optimal glycemic control in a multi-ethnic society: a US focus. Curr Diabetes Rev. 2006;2(3):285–93.
Delgado J, Jacobs EA, Lackland DT, Evans DA, de Leon CF. Differences in blood pressure control in a large population-based sample of older African Americans and non-Hispanic whites. J Gerontol A Biol Sci Med Sci. 2012;67(11):1253–8.
Johnston G, Goss JR, Malmgren JA, Spertus JA. Health status and social risk correlates of extended length of stay following coronary artery bypass surgery. Ann Thorac Surg. 2004;77(2):557–62.
Schatzkin A. Variation in inpatient racial composition among acute-care hospitals in New York State. Soc Sci Med. 1985;20(4):371–9.
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
LaPar DJ, Bhamidipati CM, Mery CM, Stukenborg GJ, Jones DR, Schirmer BD, et al. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010;252(3):544–50; discussion 50–1.
Kelz RR, Gimotty PA, Polsky D, Norman S, Fraker D, DeMichele A. Morbidity and mortality of colorectal carcinoma surgery differs by insurance status. Cancer. 2004;101(10):2187–94.
Roetzheim RG, Pal N, Tennant C, Voti L, Ayanian JZ, Schwabe A, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91(16):1409–15.
Bradley CJ, Given CW, Roberts C. Late stage cancers in a Medicaid-insured population. Med Care. 2003;41(6):722–8.
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9(3):222–31.
Cohen JW. Medicaid policy and the substitution of hospital outpatient care for physician care. Health Serv Res. 1989;24(1):33–66.
Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279(21):1703–8.
Author contributions
Study conception and design: Chan, Damle, Davids, Suwanabol, Sturrock, Sweeney, Maykel, Alavi
Acquisition of data: Damle, Suwanabol, Alavi
Analysis and Interpretation of data: Chan, Damle, Suwanabol, Alavi
Drafting of manuscript: Chan, Suwanabol, Alavi
Critical revisions: Damle, Davids, Sturrock, Sweeney, Maykel
Final Approval: Chan, Damle, Davids, Suwanabol, Sturrock, Sweeney, Maykel, Alavi
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts or disclosures to report.
Funding
The authors have no funding sources to disclose.
Additional information
Sook Y. Chan M.D. and Pasithorn A. Suwanabol M.D. contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chan, S.Y., Suwanabol, P.A., Damle, R.N. et al. Characterizing Short-Term Outcomes Following Surgery for Rectal Cancer: the Role of Race and Insurance Status. J Gastrointest Surg 20, 1891–1898 (2016). https://doi.org/10.1007/s11605-016-3241-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3241-9