Abstract
Background
While the use of laparoscopy has increased among patients undergoing colorectal surgery, there is ongoing debate regarding the oncologic equivalence of laparoscopy compared to open low anterior resection (LAR) for rectal cancer.
Methods
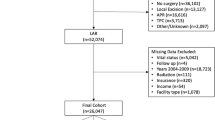
The 2010–2011 NCDB was queried for patients undergoing LAR for rectal cancer. Subjects were grouped by laparoscopic (LLAR) versus open (OLAR) technique. Baseline characteristics were compared. Subjects were propensity matched, and outcomes were compared between groups.
Results
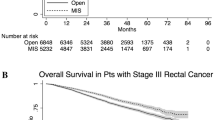
A total of 18,765 patients were identified (34.3 % LLAR, 65.7 % OLAR). After propensity matching, all baseline variables were highly similar except for carcinoembryonic antigen (CEA) level. Complete resection was more common in patients undergoing LLAR (91.6 vs. 88.9 %, p < 0.001), and statistically significant benefits were observed for gross, microscopic, and circumferential (>1 mm) margins (all p < 0.001). There was no difference in median number of lymph nodes obtained (15 vs. 15). Patients undergoing LLAR had shorter lengths of stay (5 vs. 6 days, p < 0.001) without a corresponding increase in 30-day readmission rates (6 vs. 7 %, p = 0.02).
Conclusions
Laparoscopic LAR appears to result in equivalent short-term oncologic outcomes compared to the traditional open approach as measured via surrogate endpoints in the NCDB. While these results support the increasing use of laparoscopy in rectal surgery, further data are necessary to assess long-term outcomes.
Similar content being viewed by others
References
ACS. Colorectal Cancer Facts & Figures Atlanta, Georgia2014 [April 9, 2014]. Available from: http://www.cancer.org/acs/groups/content/documents/document/acspc-042280.pdf.
Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. The New England journal of medicine. 2006 Sep 14;355(11):1114-23. PubMed PMID: 16971718.
Camma C, Giunta M, Fiorica F, Pagliaro L, Craxi A, Cottone M. Preoperative radiotherapy for resectable rectal cancer: A meta-analysis. JAMA : the journal of the American Medical Association. 2000 Aug 23-30;284(8):1008-15. PubMed PMID: 10944647.
Bosset JF, Calais G, Mineur L, Maingon P, Stojanovic-Rundic S, Bensadoun RJ, et al. Fluorouracil-based adjuvant chemotherapy after preoperative chemoradiotherapy in rectal cancer: long-term results of the EORTC 22921 randomised study. The lancet oncology. 2014 Feb;15(2):184-90. PubMed PMID: 24440473.
Baik SH, Gincherman M, Mutch MG, Birnbaum EH, Fleshman JW. Laparoscopic vs open resection for patients with rectal cancer: comparison of perioperative outcomes and long-term survival. Diseases of the colon and rectum. 2011 Jan;54(1):6-14. PubMed PMID: 21160307.
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. The lancet oncology. 2013 Mar;14(3):210-8. PubMed PMID: 23395398.
Bilimoria KY, Bentrem DJ, Nelson H, Stryker SJ, Stewart AK, Soper NJ, et al. Use and outcomes of laparoscopic-assisted colectomy for cancer in the United States. Archives of surgery. 2008 Sep;143(9):832-9; discussion 9-40. PubMed PMID: 18794419.
Speicher PJ, Englum BR, Jiang B, Pietrobon R, Mantyh CR, Migaly J. The impact of laparoscopic versus open approach on reoperation rate after segmental colectomy: a propensity analysis. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2014 Feb;18(2):378-84. PubMed PMID: 23897083.
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005 May 14-20;365(9472):1718-26. PubMed PMID: 15894098.
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. The lancet oncology. 2009 Jan;10(1):44-52. PubMed PMID: 19071061.
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr., et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Annals of surgery. 2007 Oct;246(4):655-62; discussion 62-4. PubMed PMID: 17893502.
Bagshaw PF, Allardyce RA, Frampton CM, Frizelle FA, Hewett PJ, McMurrick PJ, et al. Long-term outcomes of the australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: the Australasian Laparoscopic Colon Cancer Study trial. Annals of surgery. 2012 Dec;256(6):915-9. PubMed PMID: 23154392.
Braga M, Frasson M, Vignali A, Zuliani W, Capretti G, Di Carlo V. Laparoscopic resection in rectal cancer patients: outcome and cost-benefit analysis. Diseases of the colon and rectum. 2007 Apr;50(4):464-71. PubMed PMID: 17195085.
Feliciotti F, Guerrieri M, Paganini AM, De Sanctis A, Campagnacci R, Perretta S, et al. Long-term results of laparoscopic versus open resections for rectal cancer for 124 unselected patients. Surgical endoscopy. 2003 Oct;17(10):1530-5. PubMed PMID: 12874687.
Law WL, Lee YM, Choi HK, Seto CL, Ho JW. Laparoscopic and open anterior resection for upper and mid rectal cancer: an evaluation of outcomes. Diseases of the colon and rectum. 2006 Aug;49(8):1108-15. PubMed PMID: 16763756.
NCDB. American College of Surgeons: Cancer Programs: National Cancer Data Base (NCDB) 2013. Available from: http://www.facs.org/cancer/ncdb/.
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004 Apr 10;363(9416):1187-92. PubMed PMID: 15081650.
Clinicaltrials.gov. Laparoscopic-Assisted Resection or Open Resection in Treating Patients With Stage IIA, Stage IIIA, or Stage IIIB Rectal Cancer 2013 [April 9, 2014]. Available from: http://clinicaltrials.gov/show/NCT00726622.
Krane MK, Fichera A. Laparoscopic rectal cancer surgery: where do we stand? World journal of gastroenterology : WJG. 2012 Dec 14;18(46):6747-55. PubMed PMID: 23239912. Pubmed Central PMCID: 3520163.
Nandakumar G, Fleshman JW. Laparoscopy for rectal cancer. Surgical oncology clinics of North America. 2010 Oct;19(4):793-802. PubMed PMID: 20883954.
Kim CW, Yoon YS, Park IJ, Lim SB, Yu CS, Kim JC. Elevation of preoperative s-CEA concentration in stage IIA colorectal cancer can also be a high risk factor for stage II patients. Annals of surgical oncology. 2013 Sep;20(9):2914-20. PubMed PMID: 23760586.
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002 Jun 29;359(9325):2224-9. PubMed PMID: 12103285.
Milsom JW, Bohm B, Hammerhofer KA, Fazio V, Steiger E, Elson P. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. Journal of the American College of Surgeons. 1998 Jul;187(1):46-54; discussion -5. PubMed PMID: 9660024.
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. The lancet oncology. 2005 Jul;6(7):477-84. PubMed PMID: 15992696.
Clinical Outcomes of Surgical Therapy Study G. A comparison of laparoscopically assisted and open colectomy for colon cancer. The New England journal of medicine. 2004 May 13;350(20):2050-9. PubMed PMID: 15141043.
Mamidanna R, Burns EM, Bottle A, Aylin P, Stonell C, Hanna GB, et al. Reduced risk of medical morbidity and mortality in patients selected for laparoscopic colorectal resection in England: a population-based study. Archives of surgery. 2012 Mar;147(3):219-27. PubMed PMID: 22106248.
Kemp JA, Finlayson SR. Outcomes of laparoscopic and open colectomy: a national population-based comparison. Surgical innovation. 2008 Dec;15(4):277-83. PubMed PMID: 19036732.
Funding
Departmental funds
Author information
Authors and Affiliations
Corresponding author
Additional information
The NCDB is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. The data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed or the conclusions drawn from these data by the investigators.
Discussant
Dr. Alessio Pigazzi (Orange, CA): I congratulate Dr. Nussbaum and colleagues for this study on the short-term outcomes of laparoscopic low anterior resection.
This work adds to a growing body of literature showing superior postoperative results with a laparoscopic approach compared to open surgery for patients with rectal cancer.
Querying the National Cancer Data Base (NCDB) allowed the authors to identify over 6,000 patients who presumably had a laparoscopic anterior resection. However, a significant potential for bias and coding errors exists when dealing with large administrative data sets, and with that in mind, I would like the authors to address the following concerns.
1. Do the authors feel certain that the term “laparoscopic” in this series refers indeed to a laparoscopic pelvic dissection, instead of a laparoscopic mobilization of the left colon followed by an open total mesorectal excision (TME) as is often done in the USA?
2. Given the rapid growth of robotic surgery for TME, how can the authors be sure that coding errors did not result in a substantial number of the laparoscopic cases actually representing robotic rectal operations?
3. Lastly, there are now two randomized clinical trials, several meta-analyses, and many large series supporting the use of laparoscopy for rectal cancer with superior short-term outcomes compared to open surgery. Shouldn’t we be recommending the adoption of minimal access surgery as the procedure of choice in experienced centers for patient with rectal cancer?
Again, I congratulate the authors for this important work.
Closing Discussant
Dr. Nussbaum: Thank you, Dr. Pigazzi, for your thoughtful comments. With regard to your first question, the National Cancer Data Base characterizes surgical technique as open, laparoscopic/endoscopic, or robotic. Moreover, laparoscopic and robotic cases are further characterized by whether they were converted to open surgery. Overall, there was an approximate 20 % rate of conversion to open surgery, and these cases we classified in the laparoscopic group on an intention-to-treat basis. This rate is in keeping with previous reports of laparoscopic low anterior resection, and thus we feel confident that this cohort reflects patients who underwent laparoscopic pelvic dissection rather than simply takedown of the splenic flexure. Regarding your second question, 2010 was the year that the NCDB began to provide granular data on surgical technique, including laparoscopy versus robotics. This is the reason we chose 2010 to 2011 as our study interval. In both of the first two questions you raised, it is important to acknowledge that as with all large data sets, it is possible that some cases were misclassified, and coding errors may have resulted in some patients being miscategorized. Observer bias is always a possibility when analyzing large data sets, and this is something that we remain mindful of. However, we do not consider this a major limitation. To address your final point, we agree that there is a growing body of evidence supporting the use of minimally invasive techniques for resecting rectal tumors. We hope that this present study contributes meaningfully to this evidence. Nonetheless, among the studies addressing short-term oncologic outcomes for laparoscopic total mesorectal excision—even the randomized clinical trials—there exist conflicting outcomes data regarding margin status and completeness of resection. Much of this equivocality is likely the result of limitations in the design of previous studies. For example, not all previous trials have randomized patients based on planned procedure (e.g., abdominoperineal versus low anterior resection). This heterogeneity has made it challenging to interpret studies in which margin status was inferior following laparoscopic resection and certainly makes it difficult to fully endorse laparoscopic low anterior resection as the standard of care for rectal cancer. Given the retrospective nature of our study, we would not feel comfortable making this claim now based off of our findings. However, we do agree that many of the studies to date, including our present study, suggest that laparoscopic resection by experienced surgeons provides improved short-term outcomes among appropriately selected patients with rectal cancer. The ongoing ACSOG-Z6051 trail should address this question in an unbiased way, remedying many of the issues I mentioned previously. We think that only once the results of that trial are available can we truly evaluate laparoscopic low anterior resection as the standard of care for rectal cancer.
Rights and permissions
About this article
Cite this article
Nussbaum, D.P., Speicher, P.J., Ganapathi, A.M. et al. Laparoscopic Versus Open Low Anterior Resection for Rectal Cancer: Results from the National Cancer Data Base. J Gastrointest Surg 19, 124–132 (2015). https://doi.org/10.1007/s11605-014-2614-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2614-1