Abstract
Background
Presently, the role of liver resection (LR) for multifocal hepatocellular carcinoma (HCC) remains controversial. However, in many regions worldwide, LR remains the only treatment modality available to such patients which offers the possibility of long-term cure. The aim of this study is to determine the outcomes and prognostic factors of patients with multifocal HCC after LR.
Methods
This is a retrospective analysis of 110 patients who underwent potentially curative LR for pathologically proven multifocal HCC between 2000 and 2011.
Results
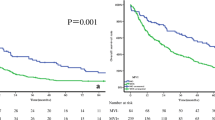
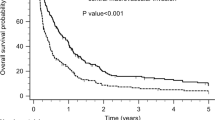
The median age was 64 (range, 18–84) years, and there were 88 males (80.0 %). Sixty-one patients underwent a major hepatectomy, and the overall postoperative mortality was 1.8 %. Sixty-eight patients had liver cirrhosis, of which, 58 were child’s A and 10 were child’s B. The 1- and 5-year overall survival (OS) was 82 and 44 %, respectively. The corresponding 1- and 5-year recurrence-free survival (RFS) was 57 and 19 %, respectively. Multivariate analysis demonstrated that the number of nodules (>3) and presence of microvascular invasion were associated with RFS. Number of nodules (>3), margin positivity, Child-Pugh status, and presence of microvascular invasion were independent prognostic factors of OS.
Conclusions
LR followed by treatment of recurrences may result in reasonable long-term survival and should be considered in a selected group of patients with multifocal HCC. Number of nodules (>3), margin positivity, Child-Pugh status, and presence of microvascular invasion, but not tumor size, were independent negative predictors of OS. These findings have potential implications on the AJCC staging for multifocal HCC.



Similar content being viewed by others
References
Ho CM, Huang GT, Tsang YM, et al. Liver resection improves the survival of patients with multiple hepatocellular carcinomas. Ann Surg Oncol 2009;16:848–55.
Cheng CH, Lee CF, Wu TH, et al. Evaluation of the new AJCC staging system for resectable hepatocellular carcinoma. World J Surg Oncol 2011;9:114
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology 2005;42:1208–36.
Kim PT, Jang JH, Atenafu EG, et al. Outcomes after hepatic resection and subsequent multimodal treatment of recurrence for multifocal hepatocellular carcinoma. Br J Surg 2013;100:1516–22.
Pons F, Varela M, Llovet M. Staging systems in hepatocellular carcinoma. HPB (Oxford) 2005;7:35–41.
Makuuchi M, Kokudo N, Arii S, et al. Development of evidence-based clinical guidelines for the diagnosis and treatment of hepatocellular carcinoma in Japan, Hepatol Res 2008;39:37–51.
Forner A, Llover JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245–1255.
Torzilli G, Donadon M, Marconi M, et al. Hepatectomy for stage B and stage C hepatocellular carcinoma in the Barcelona clinic liver cancer classification: results of a prospective analysis. Arch Surg 2008;143:1082–90.
Ishizawa T, Hasegawa K, Aoki T, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 2008;134:1908–16.
Minagawa M, Ikai I, Matsuyama Y, et al. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,7722 patients in Japan. Ann Surg 2007;245:909–922.
Ng KK, Vauthney JN, Pawlik TM, et al. Is hepatic resection for large or multinodular hepatocellular carcinoma justified? Results from a multi-institutional database. Ann Surg Oncol 2005;12:1–10.
Fan ST, Mau Lo C, Poon RT, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma. Ann Surg 2011;253:745–58.
American Joint Committee on Cancer. American Joint Committee on Cancer Staging Manual, 7th, Edge SB, Byrd DR, Compton CC, et al. (Eds), Springer, New York 2010:175.
Choi SH, Choi GH, Kim SU, et al. Role of surgical resection for multiple hepatocellular carcinomas. World J Gastroenterol 2013;19(3):366–74.
Fan ST, Poon RT, Yeung C, et al. Outcomes after partial hepatectomy for hepatocellular carcinoma within the Milan criteria. Br J Surg 2011;98:1292–300.
Lim KC, Chow PK, Allen JC, et al. Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to Milan criteria. Ann Surg 2011;254:108–13.
Wang JH, Changchien CS, Hu TH, et al. The efficacy of treatment schedules according to Barcelona Clinic Liver Cancer staging for hepatocellular carcinoma-survival analysis of 3892 patients. Eur J Cancer 2008;44:1000–6.
Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–90.
Zhong JH, Ke Y, Gong WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg 2013 in press
Cheung TT, Ng KK, Chok KS, et al. Combined resection and radiofrequency ablation for multifocal hepatocellular carcinoma: prognosis and outcomes. World J Gastroenterol 2010;16:3056–62.
Vauthey JN, Lauwers GY, Esnaola NF, et al. Simplified staging for hepatocellular carcinoma. J Clin Oncol 2002;20:1527–36.
Vauthey JN, Klimstra D, Blumgart LH. A simplified staging system for hepatocellular carcinomas. Gastroenterology 1995;108:617–8.
Huang J, Zhang Y, Peng Z, et al. A modified TNM-7 staging system to better predict the survival in patients with hepatocellular carcinoma after hepatectomy. J Cancer Res Clin Oncol 2013;139:1709–19.
Tsai TJ, Chau GY, Lui WY, et al. Clinical significance of microscopic tumor venous invasion in patients with resectable hepatocellular carcinoma. Surgery 2000;127:603–8.
Fong Y, Sun RL, Jarnagin W, et al. An analysis of 412 cases of hepatocellular carcinoma at a western center. Ann Surg 1998;229:790–800.
Funding
There are no sources of funding associated with this manuscript
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goh, B.K.P., Chow, P.K.H., Teo, JY. et al. Number of Nodules, Child-Pugh Status, Margin Positivity, and Microvascular Invasion, but not Tumor Size, are Prognostic Factors of Survival after Liver Resection for Multifocal Hepatocellular Carcinoma. J Gastrointest Surg 18, 1477–1485 (2014). https://doi.org/10.1007/s11605-014-2542-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2542-0