Abstract
Aim
To compare the early and late complications after left colectomy (LC) by left transverse laparotomy (LTL), midline laparotomy (ML) and laparoscopy (La).
Methods
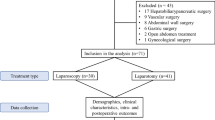
From 1998 to 2003, 328 patients underwent an LC by LTL, ML or La. After matching patients for age, ASA score and indication, 159 patients were divided into three groups of 53 patients each according to the surgical approach performed. The median follow-up was 8 years. Early and late complications were compared by univariate and multivariate analysis.
Results
Early morbidity rates after LTL, ML and La were 52 %, 45 % and 21 %, respectively (p = 0.002). Extra digestive complication rates after LTL, ML and La were 36 %, 34 % and 13.2 %, respectively (p = 0.02). Respiratory complication rates were 15 %, 21 % and 2 % (p = 0.01). The rate of wound infection was higher after LTL (15 % vs. 6 % and 6 %, p = 0.06). Length of stay was significantly shorter after La (median: LTL, 10 days; ML, 9 days; La, 6 days; p < 0.0001). At a median follow-up of 8 years, the obstruction rate was 6.3 %, regardless of the surgical approach. The rates of incisional hernia after LTL, ML and La were 8 %, 23 % and 3 % (p = 0.004), respectively, with odds ratio (OR) = 4.47 (1.2 to 16).
Conclusion
Our study shows that although La has a significant lower rate of complications, LTL, with fewer respiratory complications and hernia than ML, should be considered as the reference incision in case of conversion or contra-indication for laparoscopy.

Similar content being viewed by others
References
Laparoscopic colectomies or colectomy by laparotomy with laparoscopic preparation, S.e.v.d.a. professionnels, Editor. 2007, Service évaluation des actes professionnels, Haute autorité de santé: Paris.
Brown, S.R. and P.B. Goodfellow, Transverse versus midline incisions for abdominal surgery. Cochrane Database Syst Rev, 2005(4): CD005199.
Seiler, C.M., Deckert A, Diener MK et al. Midline versus transverse incision in major abdominal surgery: a randomized, double-blind equivalence trial (POVATI: ISRCTN60734227). Ann Surg, 2009. 249(6): p. 913–20.
Aalbers, A.G., Doeksen A, Van Berge et al. Hand-assisted laparoscopic versus open approach in colorectal surgery: a systematic review. Colorectal Dis, 2010. 12(4): 287–95.
Kuhry, E., Schwenk WF, Gaupset R et al. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev, 2008(2): CD003432.
Schwenk, W., Haase O, Neudecker J, et al. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev, 2005(3): p. CD003145.
Leung, K.L., Kwok SP, Lam SC, et al., Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet, 2004. 363(9416): p. 1187–92.
Mantion, G. Mortality and morbidity in colorectal surgery. Monographies de l'Association Francaise de Chirurgie, ed. Arnette. 2003, Rueil-Malmaison: Groupe Liaisons SA.
Gottrup, F. Oxygen in wound healing and infection. World J Surg, 2004. 28(3): 312–5.
Greif, R., Akça O, Horn EP, et al. Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. Outcomes Research Group. N Engl J Med, 2000. 342(3): p. 161–7
Tang, R., Chen HH, Wang YL et al., Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2,809 consecutive patients. Ann Surg, 2001. 234(2): p. 181–9.
Karim, H., Chafik K, Karim K, et al., Risk factors for surgical wound infection in digestive surgery. Retrospective study of 3,000 surgical wounds. Tunis Med, 2000. 78(11):634–40
Mattei, P. and Rombeau J.L., Review of the pathophysiology and management of postoperative ileus. World J Surg, 2006. 30(8): 1382–91.
Kehlet, H. and D.W. Wilmore D.W, Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg, 2008. 248(2): 189–98.
Parker, M.C., Ellis H, Moran BJ, Thompson JN, et al. Postoperative adhesions: ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Dis Colon Rectum, 2001. 44(6): 822–29; discussion 829–30.
Ellis, H. Postoperative intraabdominal adhesions: a personal view. Colorectal Dis, 2007, 9 Suppl 2: 3–8
Taylor GW, Jayne DG, Brown SR, et al. Br J Surg. Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. 2010;97(1):70–8.
Conflict of interest
There are conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borie, F., Bigourdan, JM., Pissas, MH. et al. The Best Surgical Approach for Left Colectomy: A Comparative Study Between Transverse Laparotomy, Midline Laparotomy and Laparoscopy. J Gastrointest Surg 18, 1010–1016 (2014). https://doi.org/10.1007/s11605-014-2491-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2491-7