Abstract
Introduction
In this study, we assess the effectiveness of a conservative therapeutic treatment of acute corrosive poisonings in adults, and we define therapeutic protocols based on clinical and endoscopic criteria.
Methods
We analyzed clinical records of patients with acute corrosive poisonings who were hospitalized and treated at the Toxicology Clinic at the University of Skopje, Republic of Macedonia, during a 5-year period (2006–2010). A total of 481 patients’ records with cases of acute corrosive poisonings were analyzed. There were 317 female (65.9 %) and 164 male (34.1 %) patients. The purpose of the therapy in the cases of acute corrosive poisonings is to prevent perforation as well as progressive fibrosis and stenosis of the esophagus and stomach. Therapeutic approach mainly consists of proton pump inhibitors, H2 blockers, antibiotics, and intensive hyperalimentation. There are different opinions regarding conservative treatment of acute corrosive poisonings in adults.
Conclusion
Based on our study of corrosive poisonings of adults, we propose a list of optimal treatment recommendations.
Similar content being viewed by others
Introduction
Ingestion of corrosive substances causes severe chemical burns to the upper gastrointestinal tract that are often accompanied with early or delayed complications such as gastrointestinal bleeding, perforations, esophagotracheal fistula, and esophageal or gastric stenosis. These injuries may lead to death in the acute phase of the poisoning or to nutritional issues, severe disability, and significant deterioration of life quality for the patients1,2 (Fig. 1).
Corrosive poisonings are more common in developing countries and regions where the population has lower level of health care. These poisonings can be accidental or suicidal and often cause either mild or severe post-corrosive complications. Unlike the poisonings in children that are usually accidental, corrosive ingestions in adults are in overwhelming number of cases (>90 %), results of suicide attempts. After contact with tissues, depending on the type of the corrosive agent, a coagulation or liquefaction necrosis and stenosis could appear along the entire gastrointestinal tract of the patient, from the mouth to the duodenum.3–5
Corrosive agents such as acids (hydrochloric, acetic, sulfuric), alkalis (sodium hydroxide), heavy metal salts, formalin, and various household and industry cleaning agents may cause post-corrosive injuries to the upper gastrointestinal tract. Principal factors that influence the severity of post-corrosive injuries are the pH values (of less than 2 or greater than 12), physical form, concentration and quantity of the ingested substance as well as the duration of exposure.6
The gold standard in diagnosis of corrosive poisonings is endoscopy of the esophagus and the duodenum, which is a reliable method of diagnosing acute corrosive poisonings and post-corrosive injures of the upper gastrointestinal tract. There is consensus in the scientific literature that the most optimal timing for this procedure is within the first 12–24 h post-ingestion.7,8
However, there is no consensus in the literature regarding the different treatment approaches in cases of acute corrosive poisonings. The primary purpose of the therapy is to stop the creation of esophageal stenosis, which prevents normal feeding and food absorption and usually results in additional deterioration of the patient’s conditions. Patients are usually treated with large quantities of liquids, antibiotics, H2 blockers, or proton pump (PP) inhibitors. Some authors recommend administrating large doses of corticosteroids as a possible protection from stenosis. On the other hand, other authors have reported that administration of the corticosteroid therapy in acute corrosive poisonings has not substantially contributed to the prevention of stenosis and that it might have significantly exacerbated the condition in the acute phase of poisoning.9 In cases where the standard therapeutic approach does not give initial results and patients develop stenosis, it is recommended to use retrograde intraluminal dilatation, a procedure that carries a high risk of iatrogenic injury. The other option is intraluminal esophageal stent, but its effectiveness has not yet been confirmed in a sufficient number of controlled studies or surgical intervention.10–13
The aim of this study was to present and assess the safety and effectiveness of conservative therapy in acute corrosive poisonings in adults by defining therapeutic protocol based on clinical and endoscopic criteria.
Material and Methods
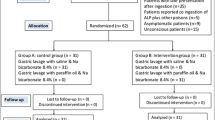
In this study, we analyzed historical clinical records of patients with acute corrosive poisonings who were hospitalized and treated at the University Clinic of Toxicology in Skopje, Republic of Macedonia, during a 5-year period (2006–2010). All data were entered in a specially designed database using a protocol, which included disease history, endoscopy information performed in the first 12–24 h after ingestion, classification of post-corrosive injuries of the upper gastrointestinal tract, as well as the control esophagogastroduodenoscopy 15 and 25 days after caustic ingestion.
Esophagogastroduodenoscopy (EGD) was performed by an experienced team of physicians using endoscopes for upper endoscopy of the Olympus type (Japan), with a diameter of 9.2 mm. Classification of post-corrosive injuries was done according to Kikendall’s scale (Table 1). Between the 25th and 30th day after the caustic ingestion, all patients underwent x-ray imaging of the esophagus, stomach, and duodenum using gastrographin.
The therapeutic protocol for each patient was defined depending on the grade of post-corrosive injuries detected with endoscopy. Patients with grade I injury were discharged to home care if the condition was stable after 48 h of observation. Observation was made in order to discover if patients were intoxicated with some other chemical agent or medicine in addition to the corrosive poisoning. Patients with grade IIA were hospitalized for 7–10 days and treated with liquid diet, H2 blockers, antibiotics, and symptomatic therapy. Patients with grade IIB or III injury were treated with intensive hyperalimentation (parenteral or enteral), H2 blockers or PP inhibitors, antibiotics, and symptomatic therapy. Conservative therapy was considered a success if there was no perforation in the first 15 days after caustic ingestion or if there was no stenosis in the upper gastrointestinal tract in the first 30 days after ingestion.
All patients who developed gastrointestinal perforation were transferred to the Surgical Clinics for emergency surgery. In patients with esophageal stenosis, a retrograde intraluminal dilatation was performed, and if there were no contraindications, patients were surgically treated. The follow-up period for all patients lasted for 12 months.
Results
We analyzed a total of 481 records of patients with acute corrosive intoxications during a 5-year period. There were 317 (65.90 %) female and 164 (34.09 %) male patients. The average age of patients was 51.43 ± 17.82 years (±95.00 % CI 45.58–53.10), while the youngest patient was 17 and the oldest 88 years old. Corrosive agent was ingested with suicidal intent by 449 (93.43 %) patients and accidentally by 32 (6.65 %) patients. All patients were admitted and hospitalized at the clinic in the first 24 h after ingestion. In the first 24 h, all patients underwent emergency esophagogastroduodenoscopy, and the majority of them ingested hydrochloric acid (n = 250, 51.95 %), acetic acid (n = 51, 10.60 %), sulfuric acid (n = 10, 2.07 %), sodium hydroxide (n = 123, 25.57 %), bleach (n = 41, 8.52 %), and hydrogen peroxide (n = 6, 1.24 %). Of the total number of patients, post-corrosive injury of grade I was registered in 45 (9.35 %) patients, grade IIA in 144 (29.93 %), grade IIB in 168 (34.92 %), grade III in 112 (23.28 %), and grade IV in 12 (2.49 %). Emergency upper endoscopy was not performed in eight patients because of clear contraindications (acute gastrointestinal bleeding, severe shock condition) (Table 2).
According to the endoscopic and clinical criteria, patients with grade I post-corrosive injuries were observed for 24 to 48 h and were given liquid food. Those with grade IIA injuries were hospitalized for 7–10 days and were given antibiotics, H2 blockers, and liquid diet. Those with grade IIB injuries received antibiotics and PP inhibitors, and a nasojejunal probe for enteral nutrition was inserted under endoscopic control. Those with grade III injuries received antibiotics and PP inhibitors, and a nasojejunal feeding tube was inserted or the nutrition was provided through a peripheral or a central vein (parenteral nutrition) (Table 3).
Patients with grade IIB and III injuries were admitted for treatment in the Intensive Care Unit. Length of hospital stay ranged between 19 and 39 days (29.52 ± 5.91), and the length of assisted nutrition ranged between 8 and 20 days (13.33 ± 2.30).
The analysis of the ratio between the type of the corrosive agent and the grade of the post-corrosive injury with the percentage of late post-corrosive complications and mortality showed that the largest percentage of post-corrosive changes was found on the esophagus and stomach due to acid and alkali poisonings resulting in grade III injury, whereas mortality was highest in grade IV injuries and happened in the acute phase (in the first 96 h after ingestion). A total of 92 (19.12 %) patients suffered from a post-corrosive stenosis, in spite of the intensive therapy, which was in agreement with other published studies. Sixty three (13.09 %) of these patients had post-corrosive stenosis on the esophagus and 29 (6.02 %) on the stomach (Fig. 2).
Of the total number of patients who had gastric post-corrosive injures during the 1 year of clinical follow-up, 16 underwent a total gastrectomy due to fibrous changes, 10 patients underwent partial gastrectomy, while no intervention was made in 3 patients due to personal or religious reasons. One of the patients died due to systemic complications (pneumonia and sepsis) 6 months after ingestion.
Esophageal dilatation was performed in 24 patients who had esophageal stenosis, two in the interval of 3 months and one after 6 months; surgical intervention was performed in 22 patients (resection with colon interposition); an esophageal stent was implanted in two patients; and 11 patients did not agree to any active treatment for different reasons; they were fed by jejunostoma. Five patients died from systemic complications (two patients due to cardiovascular complications, one due to pneumonia, and two due to acute renal failure). Eight of the patients died in the first 30 days after corrosive ingestion, five due to gastrointestinal complications (perforation) and three because of systemic complications (renal failure, hepatic failure, and DIC) (Table 4).
Discussion
In the cases of corrosive poisoning, the purpose of the therapy is to prevent perforation as well as progressive fibrosis and stenosis of the esophagus and stomach. A perforation of the esophagus or stomach can only be treated surgically.
There are different and controversial reports regarding conservative treatment of acute corrosive poisoning in adults. Therapeutic approach mainly consists of PP inhibitors, H2 blockers, antibiotics, and intensive hyperalimentation and is implemented in order to prevent late post-corrosive complications.14,15 In planning the therapeutic management, the emergency EGD plays a crucial role since it provides the necessary data regarding post-corrosive changes, which in turn dictate the protocol of the treatment. Unlike some authors who believe that endoscopic examination is not necessary in asymptomatic patients, it is our opinion that for therapy planning, all patients, without exception, must undergo an upper endoscopy.16,17 During this procedure, a classification of the post-corrosive injuries in the upper gastrointestinal tract (GIT) is done, which serves to reveal the severity of the injuries and is essential for planning the treatment protocol. Although the most used classifications are according to Zargar, Holinger, and Friedman, we used the classification suggested by Kikendall in 5 grades. The emergency EGD proved to be a very useful diagnostic–therapeutic tool in corrosive poisonings in adults.18–20
The use of corticosteroids in the treatment of acute corrosive poisonings in adults is still controversial. A study of 239 patients showed that administration of corticosteroids in the acute phase reduces the chance of late post-corrosive complications. This is in contrast to another study conducted in Europe in 572 patients, which showed that the use of corticosteroids did not significantly affect the development of post-corrosive stenosis in the upper GIT while pointing out the complications which may occur in the acute phase of poisoning.21,22 All the studies looking into justification of antibiotic therapy in acute corrosive poisonings have shown that due to the acute trauma, burns of varying degrees that damage the mucosa, submucosa, and sometimes the muscle layer of the esophagus and stomach, a positive reaction to the antibiotic in the acute phase of poisoning was detected. At the same time, controlled animal studies have shown that bacterial invasion of post-corrosively damaged mucous membrane as well as severe inflammations does induce creation of granulation tissue which results in formation of fibrosis tissue. That is why some authors justify the administration of a broad spectrum of antibiotics, in most cases of the penicillin group. In our study, all patients with grade II and III injury received antibiotics which showed very good results in favor of prevention or eradication of the infection.23,24
It is believed that antisecretory therapy in the acute phase of poisoning is extremely important in the treatment of corrosive poisoning and contributes the most to the maintenance of physiological pH level in the stomach and esophagus, thus preventing further damage from hyperacidity. A study performed in a group of 64 patients showed that more than half of the patients (>50 %) developed hyperacidity after corrosive poisoning, which in turn resulted in a gastroesophageal reflux that further damaged the esophagus. This justifies the provision of antacid therapy, mostly H2 blockers or PP inhibitors. Antisecretory therapy also proved effective in cases combined with active esophageal dilation treatment for post-corrosive stenosis. The procedure was more efficient and required less revision when it was performed on several occasions while simultaneously administering H2 blockers or PP inhibitors. A greater success rate was registered when the esophageal dilation was performed with the simultaneous use of PP inhibitors.25,26 In our study, H2 blockers were given in patients with grade IIA injury while plus 2 blockers and PP inhibitors were given to those with grade IIB and III injury. Based on our observations, we concluded that the antisecretory therapy in acute corrosive poisoning in adults is the first-choice therapy in addition to intensive hyperalimentation (Fig. 3).
Nutrition is of crucial importance in the treatment of acute corrosive poisonings because of patient’s inability to consume food due to the extensive damage of the wall of the esophagus and stomach. As a result of this hypercatabolic state and negative nitrogen balance, the patient’s condition quickly deteriorates. It is believed that food particles penetrate into granulocytes in the esophageal wall and exacerbate the inflammation. Such processes in the wall of the esophagus and stomach continue over the course of several days when a bacterial invasion resulting in inflammatory response and development of granulation tissue occurs. All these suggest that special care must be devoted to nutrition, and patients should not receive food by mouth for 10–15 days (NPO—“nil per os”). This allows the mucosa in the esophagus and stomach to regenerate faster without additional trauma.27,28 The nutrition can be parenteral or enteral thereby avoiding oral intake of food and providing the upper post-corrosive damaged GIT a chance to regenerate faster. Intensive hyperalimentation is recommended in the first 7 days, and oral intake of food is to be avoided in order to prevent further deterioration. No food intake by mouth or the so-called “esophageal rest” can last at least 10 days from the verified endoscopic grade of post-corrosive injury. Some authors suggest esophageal rest in a duration of 15–10 days, that is, until the first endoscopic checkup. During the “rest,” the patient is fed parenterally by peripheral or central vein and enterally by nasogastric or nasoenteric tube or by enterostoma (gastrostoma or jejunostoma). Most of the patients in our study were fed enterally by endoscopically inserted enteral tubes or by enterostomy. In fewer cases, they were also fed parenterally. Our analysis showed that the percentage of post-corrosive stenosis was reduced by 10–15 %. However, we do not have a sufficient number of patients to conduct a statistically relevant study that will show that enteral feeding with nasoenteric tube reduces the number of patients who develop post-corrosive stenosis of the esophagus or stomach.29,30
Most of the published studies so far on corrosive poisoning are on children of ages between 1 and 14. There are very few studies that report on corrosive poisoning of adults, and they mostly point to the importance of the drug therapy as a conservative approach. However, corrosive poisonings in children and adults are considerably different both in grades and severity of the post-corrosive complications, as well as in the preferred treatment of the patients, and the prognosis and outcome of the poisoning. This study is significant because it provides a large number of very relevant and unique data for corrosive poisonings of adults and the treatment recommendations, outcomes, and prognosis based on a 5-year-long period of observation.
In this study, we paid great attention to the hyperalimentation and the use of antisecretory therapy as treatment options for patients. Our analysis pointed to the reasons why we initiated the treatment with application of nasogastric or nasojejunal tube for artificial feeding. We found that during the first, acute phase of poisoning, the patients’ upper gastrointestinal tract was inflamed, with persistent vascular thrombosis and granulation. At the same time, presence of the tube in the lumen was of great importance. The patient did not receive any food by mouth (nil per os), so the esophagus and the stomach had an opportunity to recover maximally, without additional trauma. Based on our results, we concluded that the proposed approach of treatment gives the best results, which was supported by a relatively low percentage of early and late post-corrosive complications in the observed patient population.
The new perspective provided by this study shows an optimal approach to treatment of acute corrosive poisonings, and it emphasizes the importance of proper nutrition in patients. We suggest that for the best recovery results, the patient should not receive any food by mouth during the period of 10 to 15 days, which ideally gives the upper GIT the ability to regenerate maximally via natural processes. With that approach, we were able to achieve the main purpose in the therapy of acute corrosive poisonings, which was a prevention of late post-corrosive complications, stenosis, and strictures. Additionally, the proposed therapeutic methodology is more efficient, more economical, and preserves the lumen of the gastrointestinal tract, keeping it physiologically active.
Conclusion
The main conclusions of our analysis of corrosive poisonings of adults can be summarized in the following approach and treatment recommendations:
-
1.
It is highly beneficial to perform an emergency EGD before deciding and initiating the therapy.
-
2.
Patients with acute corrosive poisonings should be hospitalized in the intensive care unit.
-
3.
The therapy should include predominantly antibiotics, antacids (H2 blockers or PP inhibitors), and intensive hyperalimentation (enteral if possible).
-
4.
Notably fewer cases of post-corrosive stenosis of the esophagus have been noticed in patients who have been fed entirely through nasoenteric feeding tubes.
-
5.
Corticotherapy is controversial even though there are statistically relevant studies conducted in a larger number of patients showing that its administration does not prevent creation of stenosis.
References
Gen Tohda, Choichi Sugawa, Christopher Gayer, et al. Clinical evaluation and management of caustic injury in the upper gastrointestinal tract in 95 adult patients in an urban medical center. Surg Endosc 2008; 22:1119–1125
Carmen Cabral, Mirce´a Chirica, Ce´cile de Chaisemartin, et al. Caustic injuries of the upper digestive tract: a population observational study. Surg Endosc 2012; 26:214–221
N. Ananthakrishnan, G. Parthasarathy, Vikram Kate. Chronic Corrosive Injuries of the Stomach—A Single Unit Experience of 109 Patients Over Thirty Years. World J Surg 2010; 34:758–764
Andon Chibishev, Zanina Pereska, Vesna Chibisheva et al. Corrosive Poisonings in Adults . Mat Soc Med 2012; 24 : 125–130
Sarfati E, Gossot D, Assens P, et al. Management of caustic ingestion in adults. Br J Surg 1987; 74:146–148
Hao-Tsai Cheng, Chi-Liang Cheng, Cheng-Hui Lin et al. Caustic ingestion in adults: The role of endoscopic classification in predicting outcome. BMC Gastroenterology 2008; 8:31
Munoz-Bonerand N, Gornet JM. Diagnostic and therapeutic management of digestive caustic burns. J Chirug (Paris) 2002;139 : 72–6
Zargar SA, Kuchhar R, Mehta S, et al. The role of fibroptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991; 37:165–169.
Fulton JA, Hoffman RS. Steroids in second degree caustic burns of the esophagus: a systematic pooled analysis of fifty years of human data: 1956–2006. Clin Toxicol (Phila). 2007; 45:402–8.
Katzka A David MD. Caustic Injury to the Esophagus . Current Treatment Options in Gastroenterology 2001; 4:59–6
Christesen HB. Diagnostic and treatment of caustic ingestion. Ugeskr Laeger 1994;158 : 4125–4126.
Mihalache C, Mihalache S. Clinical aspects of the post-caustic esophageal stenosis on 116 cases . Rev Med Chir Soc Med Nat Iasi 2006; 110 :377–80
Zerbib P, Voisin B, Truant S, et al. The conservative management of severe caustic gastric injuries. Ann Surg. 2011; 253:684–8.
Zhou J-H, Jiang Y-G, Wang R-W et al. Management of corrosive esophageal burns in 149 cases. J Thorac Cardiovasc Surg 2005; 130: 449–55.
Ramasamy K, Gumaste V V. Corrosive ingestion in adults. J Clin Gastroenterol 2003; 37: 119–24.
Cox A J III, Eisenbeis J F. Ingestion of caustic hair relaxer: is endoscopy necessary? Laryngoscope 1997; 107: 897–902.
Celik B, Nadir A, Sahin E, Kaptanoglu M. Is esophagoscopy necessary for corrosive ingestion in adults? Dis Esophagus. 2009; 22 : 638–41
Kikendal JW. Caustic ingestion injuries. Gastroenterol Clin North Am 1991; 20 : 847–857
Zagar SA, Kochhar R, Nagar B, et al. Ingestion of corrosive acid. Gastroenterology. 1989; 97:702–707.
Triadafilopulos George. Caustic esophageal injury in adults, up to date, June 2006, Available from: http://www.uptodate.com/contents/caustic-esophageal-injury-in-adults
Mamede RC, De Mello Filho FV . Treatment of caustic ingestion: an analysis of 239 cases. Dis Esophagus 2002; 15 :210–3.
Peclova D. Navratil. Do corticosteroids prevent oesophageal stricture after corrosive ingestion. Toxicol Rev.2005; 24 : 125–9
Kardon E. Caustic ingestion, com [homepage on the Internet]. Emergency Medicine Toxicology. [updated 2010 may; cited June 2010]. Available from: emedicine.medscape.com
Carlos Arevalo-Silva, Ron Eliashar, Jay Wohlgelernter et al. Ingestion of Caustic Substances:A 15-Year Experience. Laryngoscope 2006; 116:1422–1426
Abakumov M M, Pinchuk TP, ll’iashenko LG.Is antisecretory therapy of patients with chemical burn of the esophagus mandatory. Khirurgiia (Mosk) 2007; 1:20–4.
Antisecretory therapy for prevention of stenoses of bougienage after-burn of esophageal strictures. Allakhverdian AS, Mazurin VS, Morozov SV et al. Gastroenterol. 2003; 4:36–9, 114
Chibishev A. Post-corrosive late complications in esophagus and stomach--role of the esophageal rest. Med Arh2010 .;64:320–3.
Chibishev A, Simonovska-Veljanovska N, Pereska Z. Artificial Nutrition in Therapeutic Approach of Acute Caustic Poisonings . Macedonian Journal of Medical Sciences 2010; 3:180–187.
DI Constanco. New therapeutic approaches to corrosive burns. Gut 1982; 21:370–375
Zwischenberger, Joseph B. Clare Savage, and Akhil Bidan. Surgical Aspects of Esophageal Disease Perforation and Caustic Injury. Am. J. Respir. Crit. Care Med2002; 165:1037–40
Conflict of Interest
The authors state that they had no conflict of interest during this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chibishev, A., Pereska, Z., Simonovska, N. et al. Conservative Therapeutic Approach to Corrosive Poisonings in Adults. J Gastrointest Surg 17, 1044–1049 (2013). https://doi.org/10.1007/s11605-013-2190-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2190-9