Abstract
Introduction
The pathophysiology of gastroesophageal reflux disease is multifactorial, where esophageal motility is one of the factors implicated in its genesis. However, there is still no consensus on the existence of an association between esophageal dysmotility and hiatal hernia in patients with gastroesophageal reflux disease. The objective of this study was to establish the prevalence of esophageal dysmotility in patients with hiatal hernia and to determine if herniation is a factor related to esophageal dysmotility in patients with gastroesophageal reflux disease.
Methods
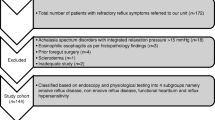
The study included 356 patients with a clinical diagnosis of gastroesophageal reflux disease submitted to upper digestive endoscopy and esophageal functional diagnostics. Hiatal hernia was defined endoscopically by a distance equal to or greater than 2 cm between the diaphragmatic constriction and the squamocolumnar junction and esophageal dysmotility when the esophageal manometry identified the amplitude of the peristaltic waves in the distal esophagus as <30 mmHg and/or less than 80% of effective contractions. For univariate statistical analysis, the patients were divided into two groups: with and without hiatal hernia. Poisson regression models were used to estimate crude and adjusted prevalence ratios (PR) of esophageal dysmotility according to hiatal hernia.
Results
Gastroesophageal reflux disease patients with hiatal hernia had a prevalence of esophageal dysmotility equal to 14.8% and those without hiatal hernia, a prevalence of 7.7% (p = 0.041). Patients with hiatal hernia also showed a higher frequency of erosive esophagitis (47.5% versus 24.2%, p < 0.001), lower low esophageal sphincter pressure (10.4 versus 13.10; p < 0.001), and higher frequency of individuals with abnormal pH-metry values (p < 0.001). The crude PR for esophageal dysmotility, according to the presence of hiatal hernia, was 1.92 (confidence interval (CI), 1.04–3.53; p = 0.037), but this association did not persist when controlled for age, esophagitis, altered pH-metry, and altered low esophageal sphincter (adjusted PR, 1.69; CI, 0.68–4.15; p = 0.257).
Conclusion
Despite the prevalence of esophageal dysmotility in the hiatal hernia group being higher than that in the group without hiatal hernia, the association between these variables in individuals with gastroesophageal reflux disease disappeared when controlling for age, esophagitis, altered pH-metry, and altered low esophageal sphincter, leading us to believe that in these patients, hiatal hernia is not an independent risk factor for dysmotility.
Similar content being viewed by others
References
Kahrilas PJ. GERD pathogenesis, pathophysiology, and clinical manifestations. Cleve Clin J Med 2003;70 Suppl 5:S4-19.
Lord RV, DeMeester SR, Peters JH, Hagen JA, Elyssnia D, Sheth CT, et al. Hiatal hernia, lower esophageal sphincter incompetence, and effectiveness of Nissen fundoplication in the spectrum of gastroesophageal reflux disease. J Gastrointest Surg 2009;13(4):602–10.
Kahrilas PJ, Shi G, Manka M, Joehl RJ. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gastroenterology 2000;118(4):688–95.
Kahrilas PJ, Lee TJ. Pathophysiology of gastroesophageal reflux disease. Thorac Surg Clin 2005;15(3):323–33.
Fornari F, Callegari-Jacques SM, Scussel PJ, Madalosso LF, Barros EF, Barros SG. Is ineffective oesophageal motility associated with reflux oesophagitis? Eur J Gastroenterol Hepatol 2007;19(9):783–7.
Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW. Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg 1996;171(1):182–6.
Fein M, Ritter MP, DeMeester TR, Oberg S, Peters JH, Hagen JA, et al. Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. J Gastrointest Surg 1999;3(4):405–10.
Ye P, Li ZS, Xu GM, Zou DW, Xu XR, Lu RH. Esophageal motility in patients with sliding hiatal hernia with reflux esophagitis. Chin Med J (Engl) 2008;121(10):898–903.
Kasapidis P, Vassilakis JS, Tzovaras G, Chrysos E, Xynos E. Effect of hiatal hernia on esophageal manometry and pH-metry in gastroesophageal reflux disease. Dig Dis Sci 1995;40(12):2724–30.
Cuomo R, Sarnelli G, Grasso R, Alfieri M, Bottiglieri ME, Paternuosto M, et al. Manometric study of hiatal hernia and its correlation with esophageal peristalsis. Dig Dis Sci 1999;44(9):1747–53.
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101(8):1900–20
Moraes-Filho J, Cecconello I, Gama-Rodrigues J, Castro L, Henry MA, Meneghelli UG, et al. Brazilian consensus on gastroesophageal reflux disease: proposals for assessment, classification, and management. Am J Gastroenterol 2002;97(2):241–8.
Cadiot G, Bruhat A, Rigaud D, Coste T, Vuagnat A, Benyedder Y, et al. Multivariate analysis of pathophysiological factors in reflux oesophagitis. Gut 1997;40(2):167–74.
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999;45(2):172–80.
Zaninotto G, DeMeester TR, Schwizer W, Johansson KE, Cheng SC. The lower esophageal sphincter in health and disease. Am J Surg 1988;155(1):104–11.
Leite LP, Johnston BT, Barrett J, Castell JA, Castell DO. Ineffective esophageal motility (IEM): the primary finding in patients with nonspecific esophageal motility disorder. Dig Dis Sci 1997;42(9):1859–65.
Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet 1951;92(4):419–31.
Crookes PF. Physiology of reflux disease: role of the lower esophageal sphincter. Surg Endosc 2006;20 Suppl 2:S462-6.
Chrysos E, Prokopakis G, Athanasakis E, Pechlivanides G, Tsiaoussis J, Mantides A, et al. Factors affecting esophageal motility in gastroesophageal reflux disease. Arch Surg 2003;138(3):241–6.
Diener U, Patti MG, Molena D, Fisichella PM, Way LW. Esophageal dysmotility and gastroesophageal reflux disease. J Gastrointest Surg 2001;5(3):260–5.
Meneghetti AT, Tedesco P, Damani T, Patti MG. Esophageal mucosal damage may promote dysmotility and worsen esophageal acid exposure. J Gastrointest Surg 2005;9(9):1313–7.
Herbella FA, Tedesco P, Nipomnick I, Fisichella PM, Patti MG. Effect of partial and total laparoscopic fundoplication on esophageal body motility. Surg Endosc 2007;21(2):285–8.
Heider TR, Behrns KE, Koruda MJ, Shaheen NJ, Lucktong TA, Bradshaw B, et al. Fundoplication improves disordered esophageal motility. J Gastrointest Surg 2003;7(2):159–63.
Oleynikov D, Eubanks TR, Oelschlager BK, Pellegrini CA. Total fundoplication is the operation of choice for patients with gastroesophageal reflux and defective peristalsis. Surg Endosc 2002;16(6):909–13.
Xu JY, Xie XP, Song GQ, Hou XH. Healing of severe reflux esophagitis with PPI does not improve esophageal dysmotility. Dis Esophagus 2007;20(4):346–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Conrado, L.M., Gurski, R.R., da Rosa, A.R.P. et al. Is There an Association Between Hiatal Hernia and Ineffective Esophageal Motility in Patients with Gastroesophageal Reflux Disease?. J Gastrointest Surg 15, 1756–1761 (2011). https://doi.org/10.1007/s11605-011-1619-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1619-2