Abstract
Introduction
Achalasia is a rare esophageal motility disorder, incurable but amenable to palliative treatments to relieve dysphagia. Given the rarity of the disease, there is a paucity of data from population-based studies on incidence and outcome of the two treatments most commonly used in clinical practice, i.e., endoscopic pneumatic dilation (PD) and surgical myotomy (SM).
Materials and Methods
A retrospective longitudinal study was conducted on the Veneto region, in north-eastern Italy. All patients with achalasia as their primary diagnosis between 2001 and 2005 were identified and their demographics and treatment details obtained.
Results
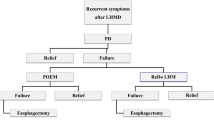
The overall incidence of achalasia was 1.59 cases/100,000/year. Achalasia patients were mainly seen at University Hospitals. Fifty-five percent of the patients received treatment, 23.3% SM and 31.8% PD. The cumulative risk of any subsequent intervention for achalasia was 20% in treated patients (29.7% in patients treated primarily with PD and 4% in patients treated with SM first).
Discussion
The epidemiology of achalasia in the Veneto Region is in line with the situation reported elsewhere and did not change between 2001 and 2005. Achalasia patients are mostly seen at University Hospitals. We observed a greater risk of subsequent intervention for patients previously treated with PD compared with SM.




Similar content being viewed by others
References
Vaezi MF, Richter JE. Diagnosis and management of achalasia. Am J Gastroenterol 1999;94:3406–3412.
Smith B. The neurological lesion in achalasia of the cardia. Gut 1970;11:388–391.
Arber N, Grossman A, Lurie B, Hoffman M, Rubinstein A, Lilos P, Rozen P, Gilat T. Epidemiology of achalasia in central Israel. Rarity of esophageal cancer. Dig Dis Sci 1993;38:1920–1925.
Mayberry JF, Atkinson M. Variations in the prevalence of achalasia in Great Britain and Ireland: an epidemiological study based on hospital admission. Q J Med 1987;62:67–74.
Mayberry JF, Atkinson M. Incidence of achalasia in New Zealand, 1980-84: an epidemiologic study based on hospital discharges. J Gastroenterol Hepatol 1988;3:247–252.
Mayberry JF, Atkinson M. Studies of incidence and prevalence of achalasia in the Nottingham area. Q J Med 1985;40:391–393.
Sonnenberg A, Massey BT, McCarty DJ, Jacobsen SJ. Epidemiology of hospitalization for achalasia in the United States. Dig Dis Sci 1993;38:233–244
Farrukh A, DeCaestecker J, Mayberry JF. An epidemiological study of achalasia among the South Asian population of Leicester, 1986–2005. Dysphagia 2008;23:161–164.
Sonnenberg A. Hospitalization for achalasia in the United States 1997–2006. Dig Dis Sci 2009;54:1680–1685.
Earlam RJ, Ellis FH Jr, Nobrega FT. Achalasia of the esophagus in a small urban community. Mayo Clin Proc 1969;44:478–483.
Mayberry JF, Rhodes J. Achalasia in the city of Cardiff from 1926 to 1977. Digestion 1980;20:248–252.
Lopushinsky SR, Urbach DR. Pneumatic dilatation and surgical myotomy for achalasia. JAMA 2006;296:2227–2233.
Karamanolis G, Sgouros S, Karatzias G, Papadopoulou E, Vasiliadis K, Stefanidis G, Mantides A. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol 2005;100:270–274.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E. Four hundred laparoscopic myotomies for esophageal achalasia: a single center experience. Ann Surg 2008;248: 986–993.
Csendes A, Braghetto I, Henriquez A, Cortés C. Late results of a prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia. Gut 1989;30:299–304.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gennaro, N., Portale, G., Gallo, C. et al. Esophageal Achalasia in the Veneto Region: Epidemiology and Treatment. J Gastrointest Surg 15, 423–428 (2011). https://doi.org/10.1007/s11605-010-1392-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1392-7