Abstract
Background
Sarcopenia is essential in managing advanced stage (III–IV) non-small cell lung cancer (NSCLC) but is laborious to diagnose using currently available method. This study aimed to establish a simple approach to predict sarcopenia using 18F-FDG PET/CT parameters and clinical characteristics and determine their roles in prognostication in advanced stage NSCLC.
Methods
Untreated 202 NSCLC patients with stage III–IV were retrospectively reviewed. Sarcopenia was defined using the skeletal muscle index (SMI) measured at the third lumbar vertebra (L3). 18F-FDG PET/CT metabolic parameters of maximum standard uptake value, metabolic tumor volume, and total lesion glycolysis of the primary tumor (SUVmax_T, MTV_T, and TLG_T) and of whole-body lesions (MTV_WB and TLG_WB) were measured. Besides, SUVmax of the psoas major muscle (SUVmax_Muscle) was measured at the L3 level. The diagnostic endpoint was the probability of sarcopenia, and the survival endpoints included progression-free survival (PFS) and overall survival (OS).
Results
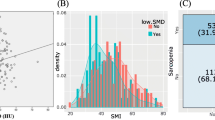
Among the enrolled 202 patients, 82 (40.6%) were diagnosed with sarcopenia. Higher age, male, lower BMI, and lower SUVmax_Muscle were correlated with a higher incidence of sarcopenia (P < 0.05), while age, sex, BMI, and SUVmax_Muscle were independently predictive of sarcopenia, and thus were utilized to construct a nomogram model. Multivariate Cox regression analysis revealed that sarcopenia score derived from the nomogram model, sarcopenia, stage, and TLG_WB were independently predictive of both PFS and OS.
Conclusion
The incidence of sarcopenia increased with declining SUVmax_Muscle in advanced stage NSCLC. Our model using age, sex, BMI, and SUVmax_Muscle might be substituted for the complicated measurement of SMI. After adjustment by stage and TLG_WB, both sarcopenia score and sarcopenia were found to be independently predictive of PFS and OS.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Bade BC, Dela Cruz CS. Lung cancer 2020: epidemiology, etiology, and prevention. Clin Chest Med. 2020;41:1–24. https://doi.org/10.1016/j.ccm.2019.10.001.
Ganti AK, Klein AB, Cotarla I, Seal B, Chou E. Update of incidence, prevalence, survival, and initial treatment in patients with non-small cell lung cancer in the US. JAMA Oncol. 2021;7:1824–32. https://doi.org/10.1001/jamaoncol.2021.4932.
Cancer Stat Facts: Lung and Bronchus Cancer. (2022) https://seer.cancer.gov/statfacts/html/lungb.html: National Cancer Institute.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20:497–530. https://doi.org/10.6004/jnccn.2022.0025.
Garinet S, Wang P, Mansuet-Lupo A, Fournel L, Wislez M, Blons H. Updated prognostic factors in localized NSCLC. Cancers (Basel). 2022;14:1400. https://doi.org/10.3390/cancers14061400.
Calvo V, Aliaga C, Carracedo C, Provencio M. Prognostic factors in potentially resectable stage III non-small cell lung cancer receiving neoadjuvant treatment-a narrative review. Transl Lung Cancer Res. 2021;10:581–9. https://doi.org/10.21037/tlcr-20-515.
Cho BC, de Pas T, Kalofonos H, Wang Q, Ramlau R, Cheng Y, et al. Prognostic factors in early-stage NSCLC: analysis of the placebo group in the MAGRIT study. Anticancer Res. 2019;39:1403–9. https://doi.org/10.21873/anticanres.13255.
Ligibel JA, Schmitz KH, Berger NA. Sarcopenia in aging, obesity, and cancer. Transl Cancer Res. 2020;9:5760–71. https://doi.org/10.21037/tcr-2019-eaoc-05.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. https://doi.org/10.1093/ageing/afy169.
Kanyilmaz G, Benli Yavuz B, Aktan M, Sahin O. Prognostic importance of (18)F-fluorodeoxyglucose uptake by positron emission tomography for stage III non-small cell lung cancer treated with definitive chemoradiotherapy. Rev Esp Med Nucl Imagen Mol (Engl Ed). 2020;39:20–6. https://doi.org/10.1016/j.remn.2019.04.006.
Chen HH, Chiu NT, Su WC, Guo HR, Lee BF. Prognostic value of whole-body total lesion glycolysis at pretreatment FDG PET/CT in non-small cell lung cancer. Radiology. 2012;264:559–66. https://doi.org/10.1148/radiol.12111148.
Ettinger DS, Wood DE, Akerley W, Bazhenova LA, Borghaei H, Camidge DR, et al. NCCN guidelines insights: non-small cell lung cancer, version 4.2016. J Natl Compr Canc Netw. 2016;14:255–64. https://doi.org/10.6004/jnccn.2016.0031.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman J, Chirieac LR, et al. Non-small cell lung cancer, version 5.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:504–35. https://doi.org/10.6004/jnccn.2017.0050.
Gomez-Perez S, McKeever L, Sheean P. Tutorial: a step-by-step guide (version 2.0) for measuring abdominal circumference and skeletal muscle from a single cross-sectional computed-tomography image using the national institutes of health imageJ. JPEN J Parenter Enteral Nutr. 2020;44:419–24. https://doi.org/10.1002/jpen.1721.
Zeng X, Shi ZW, Yu JJ, Wang LF, Luo YY, Jin SM, et al. Sarcopenia as a prognostic predictor of liver cirrhosis: a multicentre study in China. J Cachexia Sarcopenia Muscle. 2021;12:1948–58. https://doi.org/10.1002/jcsm.12797.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16:e173–80. https://doi.org/10.1016/S1470-2045(14)71116-7.
Albano D, Camoni L, Rinaldi R, Tucci A, Zilioli VR, Muzi C, et al. Comparison between skeletal muscle and adipose tissue measurements with high-dose CT and low-dose attenuation correction CT of (18)F-FDG PET/CT in elderly Hodgkin lymphoma patients: a two-centre validation. Br J Radiol. 2021;94:20200672. https://doi.org/10.1259/bjr.20200672.
Meza-Valderrama D, Marco E, Dávalos-Yerovi V, Muns MD, Tejero-Sánchez M, Duarte E, et al. Sarcopenia, malnutrition, and cachexia: adapting definitions and terminology of nutritional disorders in older people with cancer. Nutrients. 2021;13:761. https://doi.org/10.3390/nu13030761.
Yang M, Shen Y, Tan L, Li W. Prognostic value of sarcopenia in lung cancer: a systematic review and meta-analysis. Chest. 2019;156:101–11. https://doi.org/10.1016/j.chest.2019.04.115.
Kim EY, Lee HY, Kim KW, Lee JI, Kim YS, Choi WJ, et al. Preoperative computed tomography-determined sarcopenia and postoperative outcome after surgery for non-small cell lung cancer. Scand J Surg. 2018;107:244–51. https://doi.org/10.1177/1457496917748221.
Stene GB, Helbostad JL, Amundsen T, Sorhaug S, Hjelde H, Kaasa S, et al. Changes in skeletal muscle mass during palliative chemotherapy in patients with advanced lung cancer. Acta Oncol. 2015;54:340–8. https://doi.org/10.3109/0284186X.2014.953259.
Kimura M, Naito T, Kenmotsu H, Taira T, Wakuda K, Oyakawa T, et al. Prognostic impact of cancer cachexia in patients with advanced non-small cell lung cancer. Support Care Cancer. 2015;23:1699–708. https://doi.org/10.1007/s00520-014-2534-3.
Rossi S, Di Noia V, Tonetti L, Strippoli A, Basso M, Schinzari G, et al. Does sarcopenia affect outcome in patients with non-small-cell lung cancer harboring EGFR mutations? Future Oncol. 2018;14:919–26. https://doi.org/10.2217/fon-2017-0499.
Go SI, Park MJ, Song HN, Kang MH, Park HJ, Jeon KN, et al. Sarcopenia and inflammation are independent predictors of survival in male patients newly diagnosed with small cell lung cancer. Support Care Cancer. 2016;24:2075–84. https://doi.org/10.1007/s00520-015-2997-x.
Hyun SH, Ahn HK, Kim H, Ahn MJ, Park K, Ahn YC, et al. Volume-based assessment by (18)F-FDG PET/CT predicts survival in patients with stage III non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2014;41:50–8. https://doi.org/10.1007/s00259-013-2530-8.
Lee JW, Lee SM, Yun M, Cho A. Prognostic value of volumetric parameters on staging and posttreatment FDG PET/CT in patients with stage IV non-small cell lung cancer. Clin Nucl Med. 2016;41:347–53. https://doi.org/10.1097/RLU.0000000000001126.
Liao S, Penney BC, Wroblewski K, Zhang H, Simon CA, Kampalath R, et al. Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39:27–38. https://doi.org/10.1007/s00259-011-1934-6.
Okami J, Shintani Y, Okumura M, Ito H, Ohtsuka T, Toyooka S, et al. Demographics, safety and quality, and prognostic information in both the seventh and eighth editions of the TNM classification in 18,973 surgical cases of the Japanese joint committee of lung cancer registry database in 2010. J Thorac Oncol. 2019;14:212–22. https://doi.org/10.1016/j.jtho.2018.10.002.
Araghi M, Fidler-Benaoudia M, Arnold M, Rutherford M, Bardot A, Ferlay J, et al. International differences in lung cancer survival by sex, histological type and stage at diagnosis: an ICBP SURVMARK-2 Study. Thorax. 2022;77:378–90. https://doi.org/10.1136/thoraxjnl-2020-216555.
Ferguson MK, Skosey C, Hoffman PC, Golomb HM. Sex-associated differences in presentation and survival in patients with lung cancer. J Clin Oncol. 1990;8:1402–7. https://doi.org/10.1200/JCO.1990.8.8.1402.
Ferguson MK, Wang J, Hoffman PC, Haraf DJ, Olak J, Masters GA, et al. Sex-associated differences in survival of patients undergoing resection for lung cancer. Ann Thorac Surg. 2000;69:245–9. https://doi.org/10.1016/s0003-4975(99)01078-4 (discussion 9-50).
Jeon DS, Kim JW, Kim SG, Kim HR, Song SY, Lee JC, et al. Sex differences in the characteristics and survival of patients with non-small-cell lung cancer: a retrospective analytical study based on real-world clinical data of the Korean population. Thorac Cancer. 2022. https://doi.org/10.1111/1759-7714.14594.
Heymsfield SB, Stanley A, Pietrobelli A, Heo M. Simple skeletal muscle mass estimation formulas: what we can learn from them. Front Endocrinol (Lausanne). 2020;11:31. https://doi.org/10.3389/fendo.2020.00031.
Acknowledgements
This work was supported by the fund from the National Natural Science Foundation of China (81971645), Guangdong Provincial People's Hospital (KY0120211130), and Guangdong Provincial Key Laboratory of Artificial Intelligence in Medical Image Analysis and Application (No. 2022B1212010011).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11604_2022_1369_MOESM1_ESM.tif
Supplementary file1 Figure S1. The receiver operating characteristic (ROC) curve plotting the diagnostic performance of sarcopenia score to predict sarcopenia, and the area under the curve (AUC) was 0.851 (TIF 4028 KB)
About this article
Cite this article
Yuan, H., Tan, X., Sun, X. et al. Role of 18F-FDG PET/CT and sarcopenia in untreated non-small cell lung cancer with advanced stage. Jpn J Radiol 41, 521–530 (2023). https://doi.org/10.1007/s11604-022-01369-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-022-01369-9