Abstract
Purpose
To clarify imaging and clinical characteristics of ovarian carcinosarcoma (CS) compared with high-grade serous carcinoma (HGSC).
Methods
We retrospectively reviewed MR imagings of 12 patients with CS and 30 patients with HGSC and evaluated tumor size, shape, appearance, nature of cystic and solid components, hemorrhage, and necrosis. Age, premenopausal or postmenopausal, histologic subtype, presence of endometriosis, tumor markers, and stage were also evaluated. These parameters were compared using the Mann–Whitney U test and the chi-square test/Fisher’s exact test.
Results
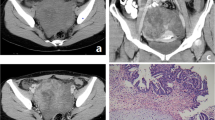
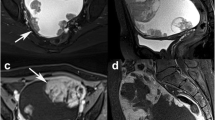
The mean size of CSs was 13.6 cm, and significantly larger than that of HGSCs (mean 9.0 cm, p = 0.022). The stained-glass appearance (67% vs. 23%, p = 0.013), hemorrhage (100% vs. 50%, p = 0.003), necrosis (75.0% vs. 13%, p = 0.000), and endometriosis (33% vs. 7%, p = 0.012) were significantly more common in CSs. The postmenopausal ratio of CSs was 100% and significantly higher than that of HGSCs (70.0%, p = 0.041). Among the tumor makers, only CA-125 was significantly lower in CSs than in HGSCs (mean 715.1 U/ml vs. 1677.1 U/ml, p = 0.009). The stage distribution was similar and was not significantly different.
Conclusion
CSs formed larger masses, and the stained-glass appearance, hemorrhage, and necrosis were more frequently observed in CSs.




Similar content being viewed by others
References
Ellenson LH, Kupryjanczyk J, Carinelli SG, Prat J, Cho KR, Singer G, Kim RK, Soslow R, Nogales FF, Cao D, Vang R, Carinelli SG, Zaloudek CJ. Tomours of the ovary; mixed epithelial and mesenchymal tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: IARC Press; 2013. p. 42–3.
Brown E, Stewart M, Rye T, Al-Nafussi A, Williams AR, Bradburn M, et al. Carcinosarcoma of the ovary: 19 years of prospective data from a single center. Cancer. 2004;100:2148–53. https://doi.org/10.1002/cncr.20256.
Kunkel J, Peng Y, Tao Y, Krigman H, Cao D. Presence of a sarcomatous component outside the ovary is an adverse prognostic factor for primary ovarian malignant mixed mesodermal/mullerian tumors: a clinicopathologic study of 47 cases. Am J Surg Pathol. 2012;36:831–7. https://doi.org/10.1097/PAS.0b013e31824ee500.
del Carmen MG, Birrer M, Schorge JO. Carcinosarcoma of the ovary: a review of the literature. Gynecol Oncol. 2012;125:271–7. https://doi.org/10.1016/j.ygyno.2011.12.418.
Kanis MJ, Kolev V, Getrajdman J, Zakashansky K, Cohen C, Rahaman J. Carcinosarcoma of the ovary: a single institution experience and review of the literature. Eur J Gynaecol Oncol. 2016;37:75–9.
Boussios S, Karathanasi A, Zakynthinakis-Kyriakou N, Tsiouris AK, Chatziantoniou AA, Kanellos FS, et al. Ovarian carcinosarcoma: current developments and future perspectives. Crit Rev Oncol Hematol. 2019;134:46–55. https://doi.org/10.1016/j.critrevonc.2018.12.006.
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, et al. Ovarian cancer statistics. CA Cancer J Clin. 2018;68:284–96. https://doi.org/10.3322/caac.21456.
Tanaka YO, Okada S, Satoh T, Matsumoto K, Saida T, Oki A, et al. Solid non-invasive ovarian masses on MR: histopathology and a diagnostic approach. Eur J Radiol. 2011;80:e91–7. https://doi.org/10.1016/j.ejrad.2010.05.032.
Li W, Chu C, Cui Y, Zhang P, Zhu M. Diffusion-weighted MRI: a useful technique to discriminate benign versus malignant ovarian surface epithelial tumors with solid and cystic components. Abdom Imaging. 2012;37:897–903. https://doi.org/10.1007/s00261-011-9814-x.
Tanaka YO, Okada S, Satoh T, Matsumoto K, Oki A, Saida T, et al. Differentiation of epithelial ovarian cancer subtypes by use of imaging and clinical data: a detailed analysis. Cancer Imaging. 2016. https://doi.org/10.1186/s40644-016-0061-9.
Erdem CZ, Bayar U, Erdem LO, Barut A, Gundogdu S, Kaya E. Polycystic ovary syndrome: dynamic contrast-enhanced ovary MR imaging. Eur J Radiol. 2004;51:48–53. https://doi.org/10.1016/j.ejrad.2003.08.005.
Costa MJ, Walls J. Epidermal growth factor receptor and c-erbB-2 oncoprotein expression in female genital tract carcinosarcomas (malignant mixed müllerian tumors). Clinicopathologic study of 82 cases. Cancer. 1996;77:533–42. https://doi.org/10.1002/(SICI)1097-0142(19960201)77:3<533::AID-CNCR16>3.0.CO;2-5.
Tanaka YO, Tsunoda H, Minami R, Yoshikawa H, Minami M. Carcinosarcoma of the uterus: MR findings. J Magn Reson Imaging. 2008;28:434–9. https://doi.org/10.1002/jmri.21469.
Kamishima Y, Takeuchi M, Kawai T, Kawaguchi T, Yamaguchi K, Takahashi N, et al. A predictive diagnostic model using multiparametric MRI for differentiating uterine carcinosarcoma from carcinoma of the uterine corpus. Jpn J Radiol. 2017;35:472–83. https://doi.org/10.1007/s11604-017-0655-6.
Ohguri T, Aoki T, Watanabe H, Nakamura K, Nakata H, Matsuura Y, et al. MRI findings including gadolinium-enhanced dynamic studies of malignant, mixed mesodermal tumors of the uterus: differentiation from endometrial carcinomas. Eur Radiol. 2002;12:2737–42. https://doi.org/10.1007/s00330-002-1405-3.
Kim S, Kim YT, Kim S, Kim SW, Lee JY, Kang WJ. Diagnostic value of (18) F-FDG PET/CT and MRI in the preoperative evaluation of uterine carcinosarcoma. Nucl Med Mol Imaging. 2018;52:445–52. https://doi.org/10.1007/s13139-018-0549-2.
Ling Y, Feng CY, Xia SM, Shen LH, Luo LQ, Zhang HY. Magnetic resonance imaging of ovarian carcinosarcoma: correlation to the clinicopathological findings. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30:1648–50.
Pankaj S, Nazneen S, Kumari A, Kumari S, Choudhary V, Roy VK. A rare tumor of the ovary: carcinosarcoma report and review of literature. J Obstet Gynaecol India. 2016;66:648–50. https://doi.org/10.1007/s13224-015-0788-4.
Sood AK, Sorosky JI, Gelder MS, Buller RE, Anderson B, Wilkinson EJ, et al. Primary ovarian sarcoma: analysis of prognostic variables and the role of surgical cytoreduction. Cancer. 1998;1(82):1731–7.
Ariyoshi K, Kawauchi S, Kaku T, Nakano H, Tsuneyoshi M. Prognostic factors in ovarian carcinosarcoma: a clinicopathological and immunohistochemical analysis of 23 cases. Histopathology. 2000;37:427–36. https://doi.org/10.1046/j.1365-2559.2000.01015.x.
Gourley C, Al-Nafussi A, Abdulkader M, Smyth J, Gabra H. Malignant mixed mesodermal tumours: biology and clinical aspects. Eur J Cancer. 2002;38:1437–46. https://doi.org/10.1016/s0959-8049(02)00114-4.
Sonoda Y, Saigo PE, Gederici MG, Boyd J. Carcinosarcoma of the ovary in a patient with germline BRCA2 mutation: evidence for monoclonal origin. Gynecol Oncol. 2000;76:226–9. https://doi.org/10.1006/gyno.1999.5681.
Carnevali I, Cimetti L, Sahnane N, Libera L, Cavallero A, Formenti G, et al. Two cases of carcinosarcomas of the ovary involved in hereditary cancer syndromes. Int J Gynecol Pathol. 2017;36:64–70. https://doi.org/10.1097/PGP.0000000000000290.
Matias-Guiu X, Stewart CJ. Endometriosis-associated ovarian neoplasia. Pathology. 2018;50:190–204. https://doi.org/10.1016/j.pathol.2017.10.006.
Amin K, Brumley B, Erickson BK, Khalifa MA. Müllerian carcinosarcoma arising from atypical pelvic endometriosis. Gynecol Oncol Rep. 2018;25:87–9. https://doi.org/10.1016/j.gore.2018.06.009.
Menon S, Deodhar K, Rekhi B, Dhake R, Gupta S, Ghosh J, et al. Clinico-pathological spectrum of primary ovarian malignant mixed mullerian tumors (OMMMT) from a tertiary cancer institute: a series of 27 cases. Indian J Pathol Microbiol. 2013;56:365–71. https://doi.org/10.4103/0377-4929.125293.
Marko J, Marko KI, Pachigolla SL, Crothers BA, Mattu R, Wolfman DJ. Mucinous neoplasms of the ovary: radiologic-pathologic correlation. Radiographics. 2019;39:982–97. https://doi.org/10.1148/rg.2019180221.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Tsukuba (R01-347).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Saida, T., Mori, K., Tanaka, Y.O. et al. Carcinosarcoma of the ovary: MR and clinical findings compared with high-grade serous carcinoma. Jpn J Radiol 39, 357–366 (2021). https://doi.org/10.1007/s11604-020-01072-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-01072-7