Abstract
Objective
Evidence from prospective studies on the consumption of tea and risk of gout is conflicting and limited. We aimed to investigate the potential causal effects of tea intake on gout using Mendelian randomization (MR).
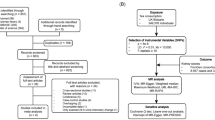
Methods
Genome-wide association studies in UK Biobank included 349 376 individuals and successfully discovered single-nucleotide polymorphisms linked to consumption of one cup of tea per day. Summary statistics from the Chronic Kidney Disease Genetics consortium included 13 179 cases and 750 634 controls for gout. Two-sample MR analyses were used to evaluate the relationship between tea consumption and gout risk. The inverse-variance weighted (IVW) method was used for primary analysis, and sensitivity analyses were also conducted to validate the potential causal effect.
Results
In this study, the genetically predicted increase in tea consumption per cup was associated with a lower risk of gout in the IVW method (OR: 0.90; 95% CI: 0.82–0.98). Similar results were found in weighted median methods (OR: 0.88; 95% CI: 0.78–1.00), while no significant associations were found in MR-Egger (OR: 0.89; 95% CI: 0.71–1.11), weighted mode (OR: 0.80; 95% CI: 0.65–0.99), and simple mode (OR: 1.01; 95% CI: 0.75–1.36). In addition, no evidence of pleiotropy was detected by MR-Egger regression (P=0.95) or MR-PRESSO analysis (P=0.07).
Conclusion
This study provides evidence for the daily consumption of an extra cup of tea to reduce the risk of gout.
Similar content being viewed by others
References
DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2018,392(10159):1859–1922
Li Q, Li X, Wang J, et al. Diagnosis and treatment for hyperuricemia and gout: a systematic review of clinical practice guidelines and consensus statements. BMJ Open, 2019,9(8):e026677
Singh JA, Gaffo A. Gout epidemiology and comorbidities. Semin Arthritis Rheum, 2020,50(3S):S11–S16
Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II: Management. Report of a task force of the EULAR Standing Committee For International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis, 2006,65(10):1312–1324
Bai L, Zhou JB, Zhou T, et al. Incident gout and weight change patterns: A retrospective cohort study of US adults. Arthritis Res Ther, 2021,23(1):69
Rho YH, Lu N, Peloquin CE, et al. Independent impact of gout on the risk of diabetes mellitus among women and men: A population-based, BMI-matched cohort study. Ann Rheum Dis, 2016,75(1):91–95
Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: part II. Arthritis Rheum, 2007,58(1):26–35
Choi HK, Mount DB, Reginato AM. Pathogenesis of gout. Ann Intern Med, 2005,143(7):499–516
Choi HK, Atkinson K, Karlson EW, et al. Purine-rich foods, dairy and protein intake, and the risk of gout in men. New Engl J Med, 2004,350(11):1093–1103
Choi HK, Atkinson K, Karlson EW, et al. Alcohol intake and risk of incident gout in men: a prospective study. Lancet, 2004,363(9417):1277–1281
Choi HK, Atkinson K, Karlson EW, et al. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Arch Intern Med, 2005,165(7):742–748
Choi HK, Curhan G. Beer, liquor, wine, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum, 2004,51(6):1023–1029
Huang HY, Appel LJ, Choi MJ, et al. The effects of vitamin C supplementation on serum concentrations of uric acid: results of a randomized controlled trial. Arthritis Rheum, 2005,52(6):1843–1847
Choi HK, Liu S, Curhan G. Intake of purine-rich foods, protein, dairy products, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum, 2005,52(1):283–289
Choi HK, Ford ES, Li C, et al. Prevalence of the metabolic syndrome in patients with gout: the Third National Health and Nutrition Examination Survey. Arthritis Rheum, 2007,57(1):109–115
Choi HK, Ford ES. Prevalence of the metabolic syndrome in individuals with hyperuricemia. Am J Med, 2007,120:442–447
Choi HK, Curhan G. Coffee, tea, and caffeine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum, 2007,57(5):816–821
Gao X, Curhan G, Forman JP, et al. Vitamin C intake and serum uric acid concentration in men. J Rheumatol, 2008,35(9):1853–1858
Gao X, Qi L, Qiao N, et al. Intake of added sugar and sugar-sweetened drink and serum uric acid concentration in US men and women. Hypertension, 2007,50(2):306–312
Williams PT. Effects of diet, physical activity and performance, and body weight on incident gout in ostensibly healthy, vigorously active men. Am J Clin Nutr, 2008,87(5):1480–1487
Choi JW, Ford ES, Gao X, et al. Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum, 2008,59(1):109–116
Choi HK, Curhan G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. Br Med J, 2008,336(7639):309–312
Nguyen S, Choi HK, Lustig RH, et al. Sugar-sweetened beverages, serum uric acid, and blood pressure in adolescents. J Pediatr, 2009,154(6):807–813
Choi HK, Gao X, Curhan G. Vitamin C intake and the risk of gout in men: a prospective study. Arch Intern Med, 2009,169(5):502–507
Gaeini Z, Bahadoran Z, Mirmiran P, et al. Tea, coffee, caffeine intake and the risk of cardio-metabolic outcomes: findings from a population with low coffee and high tea consumption. Nutr Metab (Lond), 2019,16:28
Choi HK, Willett W, Curhan G. Coffee consumption and risk of incident gout in men: a prospective study. Arthritis Rheum, 2007,56(6):2049–2055
Choi HK, Curhan G. Coffee consumption and risk of incident gout in women: the Nurses’ Health Study. Am J Clin Nutr, 2010,92(4):922–927
Bahorun T, Luximon-Ramma A, Gunness TK, et al. Black tea reduces uric acid and C-reactive protein levels in humans susceptible to cardiovascular diseases. Toxicology, 2010,278(1):68–74
Teng GG, Tan CS, Santosa A, et al. Serum urate levels and consumption of common beverages and alcohol among Chinese in Singapore. Arthritis Care Res (Hoboken), 2013,65(9):1432–1440
Beyl RN Jr, Hughes L, Morgan S. Update on Importance of Diet in Gout. Am J Med, 2016,129(11):1153–1158
Stephen B, Thompson SG. Mendelian Randomization: Methods for Using Genetic Variants in Causal Estimation. London: Chapman and Hall/CRC (2015).
Larsson SC. Mendelian randomization as a tool for causal inference in human nutrition and metabolism. Curr Opin Lipidol, 2021,32(1):1–8
1000 Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, et al. A global reference for human genetic variation. Nature, 2015,526(7571):68–74
Shim H, Chasman DI, Smith JD, et al. A multivariate genome-wide association analysis of 10 LDL subfractions, and their response to statin treatment, in 1868 Caucasians. PLoS One, 2015,10:e0120758
Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol, 2011,40(4):740–752
Tin A, Marten J, Halperin Kuhns VL, et al. Target genes, variants, tissues and transcriptional pathways influencing human serum urate levels. Nat Genet, 2019,51(10):1459–1474
Didelez V, Sheehan N. Mendelian randomization as an instrumental variable approach to causal inference. Stat Methods Med Res, 2007,16(4):309–330
Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol, 2018,47(1):358
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol, 2013,37(7):658–665
Hemani G, Bowden J, Davey Smith G. Evaluating the potential role of pleiotropy in mendelian randomization studies. Hum Mol Genet, 2018,27(R2):R195–R208
Bowden J, Davey Smith G, Haycock PC, et al. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol, 2016,40(4):304–314
Hartwig FP, Davey Smith G. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol, 2017,46(6):1985–1998
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol, 2013,37(7):658–665
Chen Y, Luo L, Hu S, et al. The chemistry, processing, and preclinical anti-hyperuricemia potential of tea: a comprehensive review. Crit Rev Food Sci Nutr, 2023,63(24):7065–7090
da Silva Pinto M. Tea: a new perspective on health benefits. Sci Pireit, 2013,53(2):558–567
Fang J, Sureda A, Silva AS, et al. Trends of tea in cardiovascular health and disease: a critical review. Trends Food Sci Technol, 2019,88:385–396
Chen G, Tan ML, Li KK, et al. Green tea polyphenols decreases uric acid level through xanthine oxidase and renal urate transporters in hyperuricemic mice. J Ethnopharmacol, 2015,175:14–20
Jhang JJ, Lu CC, Yen GC. Epigallocatechin gallate inhibits urate crystals-induced peritoneal inflammation in C57BL/6 mice. Mol Nutr Food Res, 2016,60(10):2297–2303
Han M, Zhao G, Wang Y, et al. Safety and anti-hyperglycemic efficacy of various tea types in mice. Sci Rep, 2016,6:31703
Qiao J, Kong X, Kong A, et al. Pharmacokinetics and biotransformation of tea polyphenols. Curr Drug Metab, 2014,15(1):30–36
Aucamp J, Gaspar A, Hara Y, et al. Inhibition of xanthine oxidase by catechins from tea (Camellia sinensis). Anticancer Res, 1997,17(6D):4381–4385
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The authors declare that they have no conflicts of interest.
Additional information
This work was supported by grants from the Natural Science Foundation of China (No. 82102199) and the General Program of Shanghai Municipal Commission of Health and Family Planning (No. 202040479).
Supplementary data
Rights and permissions
About this article
Cite this article
Wang, Q., Liu, Yn., Zhang, H. et al. Causal Association Between Tea Consumption and Gout: A Mendelian Randomization Study. CURR MED SCI 43, 947–954 (2023). https://doi.org/10.1007/s11596-023-2778-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-023-2778-6