Abstract
Objective
This study aims to investigate the effects of hydralazine on inflammation induced by spinal cord injury (SCI) in the central nervous system (CNS) and its mechanism in promoting the structural and functional recovery of the injured CNS.
Methods
A compressive SCI mouse model was utilized for this investigation. Immunofluorescence and quantitative real-time polymerase chain reaction were employed to examine the levels of acrolein, acrolein-induced inflammation-related factors, and macrophages at the injury site and within the CNS. Western blotting was used to evaluate the activity of the phosphoinositide 3-kinase (PI3K)/AKT pathway to study macrophage regulation. The neuropathic pain and motor function recovery were evaluated by glutamic acid decarboxylase 65/67 (GAD65/67), vesicular glutamate transporter 1 (VGLUT1), paw withdrawal response, and Basso Mouse Scale score. Nissl staining and Luxol Fast Blue (LFB) staining were performed to investigate the structural recovery of the injured CNS.
Results
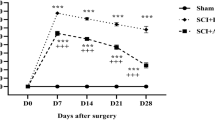
Hydralazine downregulated the levels of acrolein, IL-1β, and TNF-α in the spinal cord. The downregulation of acrolein induced by hydralazine promoted the activation of the PI3K/AKT pathway, leading to M2 macrophage polarization, which protected neurons against SCI-induced inflammation. Additionally, hydralazine promoted the structural recovery of the injured spinal cord area. Mitigating inflammation and oxidative stress by hydralazine in the animal model alleviated neuropathic pain and altered neurotransmitter expression. Furthermore, hydralazine facilitated motor function recovery following SCI. Nissl staining and LFB staining indicated that hydralazine promoted the structural recovery of the injured CNS.
Conclusion
Hydralazine, an acrolein scavenger, significantly mitigated SCI-induced inflammation and oxidative stress in vivo, modulated macrophage activation, and consequently promoted the structural and functional recovery of the injured CNS.
Similar content being viewed by others
Change history
19 April 2024
An Erratum to this paper has been published: https://doi.org/10.1007/s11596-024-2864-4
References
Cui M, Ma X, Sun J, et al. Effects of STAT3 inhibitors on neural functional recovery after spinal cord injury in rats. Biosci Trends, 2017,10(6):460–466
Sterner RC, Sterner RM. Immune response following traumatic spinal cord injury: Pathophysiology and therapies. Front in Immunol, 2022,13:1084101
Allison DJ, Ditor DS. The common inflammatory etiology of depression and cognitive impairment: a therapeutic target. J Neuroinflammation, 2014,11:151
Davies AL, Hayes KC, Dekaban GA. Clinical correlates of elevated serum concentrations of cytokines and autoantibodies in patients with spinal cord injury. Arch Phys Med Rehabil, 2007,88(11):1384–1393
Gibson AE, Buchholz AC, Martin Ginis KA. C-Reactive protein in adults with chronic spinal cord injury: increased chronic inflammation in tetraplegia vs paraplegia. Spinal Cord, 2008,46(9):616–621
Ambrozaitis KV, Kontautas E, Spakauskas B, et al. Pathophysiology of acute spinal cord injury. Medicina (Kaunas), 2006,42(3):255–261
Hall ED. Antioxidant therapies for acute spinal cord injury. Neurotherapeutics, 2011,8(2):152–167
Braughler JM, Hall ED. Central nervous system trauma and stroke. I. Biochemical considerations for oxygen radical formation and lipid peroxidation. Free Radic Biol Med, 1989,6(3):289–301
Juurlink BH, Paterson PG. Review of oxidative stress in brain and spinal cord injury: suggestions for pharmacological and nutritional management strategies. J Spinal Cord Med, 1998,21(4):309–334
Hill RL, Singh IN, Wang JA, et al. Protective effects of phenelzine administration on synaptic and non-synaptic cortical mitochondrial function and lipid peroxidation-mediated oxidative damage following TBI in young adult male rats. Exp Neurol, 2020,330:113322
Lin Y, Chen Z, Tang J, et al. Acrolein contributes to the neuropathic pain and neuron damage after ischemic–reperfusion spinal cord injury. Neuroscience, 2018,384:120–130
Herr SA, Shi L, Gianaris T, et al. Critical role of mitochondrial aldehyde dehydrogenase 2 in acrolein sequestering in rat spinal cord injury. Neural Regen Res, 2022,17(7):1505
Uchida K. Current status of acrolein as a lipid peroxidation product. Trends Cardiovasc Med, 1999,9(5):109–113
Qi H, Kan K, Sticht C, et al. Acrolein-inducing ferroptosis contributes to impaired peripheral neurogenesis in zebrafish. Front Neurosci, 2023,16:1044213
Bui LC, Manaa A, Xu X, et al. Acrolein, an α, β-unsaturated aldehyde, irreversibly inhibits the acetylation of aromatic amine xenobiotics by human arylamine N-acetyltransferase 1. Drug Metab Dispos, 2013,41(7):1300–1305
Facchinetti F, Amadei F, Geppetti P, et al. Alpha,beta-unsaturated aldehydes in cigarette smoke release inflammatory mediators from human macrophages. Am J Respir Cell Mol Biol, 2007,37(5):617–623
Moretto N, Facchinetti F, Southworth T, et al. alpha,beta-Unsaturated aldehydes contained in cigarette smoke elicit IL-8 release in pulmonary cells through mitogen-activated protein kinases. Am J Physiol Lung Cell Mol Physiol, 2009,296(5):L839–848
Hamann K, Nehrt G, Ouyang H, et al. Hydralazine inhibits compression and acrolein-mediated injuries in ex vivo spinal cord. J Neurochem, 2008,104(3):708–718
Chen Z, Park J, Butler B, et al. Mitigation of sensory and motor deficits by acrolein scavenger phenelzine in a rat model of spinal cord contusive injury. J Neurochem, 2016,138(2):328–338
Kaminskas LM, Pyke SM, Burcham PC. Reactivity of hydrazinophthalazine drugs with the lipid peroxidation products acrolein and crotonaldehyde. Org Biomol Chem, 2004,2(18):2578–2584
Due MR, Park J, Zheng L, et al. Acrolein involvement in sensory and behavioral hypersensitivity following spinal cord injury in the rat. J Neurochem, 2014,128(5):776–786
Hamann K, Durkes A, Ouyang H, et al. Critical role of acrolein in secondary injury following ex vivo spinal cord trauma. J Neurochem, 2008,107(3):712–721
Marques SA, Garcez VF, Del Bel EA, et al. A simple, inexpensive and easily reproducible model of spinal cord injury in mice: morphological and functional assessment. J Neurosci Methods, 2009,177(1):183–193
Liu-Snyder P, Borgens RB, Shi R. Hydralazine rescues PC12 cells from acrolein-mediated death. J Neurosci Res, 2006,84(1):219–227
Liu-Snyder P, McNally H, Shi R, et al. Acrolein-mediated mechanisms of neuronal death. J Neurosci Res, 2006,84(1):209–218
Gillespie ER, Ruitenberg MJ. Neuroinflammation after SCI: current insights and therapeutic potential of intravenous immunoglobulin. J Neurotrauma, 2022,39(3–4):320–332
Hall ED. Inhibition of lipid peroxidation in CNS trauma. J Neurotrauma, 1991,8(Suppl 1):S31–S41
Hall ED, Braughler JM. Free radicals in CNS injury. Res Publ Assoc Res Nerv Ment Dis, 1993,71:81–105
Sousa BC, Pitt AR, Spickett CM. Chemistry and analysis of HNE and other prominent carbonyl-containing lipid oxidation compounds. Free Radical Biol Med, 2017,111:294–308
Jure I, Pietranera L, De Nicola AF, et al. Spinal Cord Injury Impairs Neurogenesis and Induces Glial Reactivity in the Hippocampus. Neurochem Res, 2017,42(8):2178–2190
Fang J, Ou Q, Wu B, et al. TcpC Inhibits M1 but Promotes M2 Macrophage Polarization via Regulation of the MAPK/NF-kappa B and Akt/STAT6 Pathways in Urinary Tract Infection. Cells, 2022,11(17):2674
Zhou X, Chen H, Hu Y, et al. Enhancer of zeste homolog 2 promotes renal fibrosis after acute kidney injury by inducing epithelial-mesenchymal transition and activation of M2 macrophage polarization. Cell Death Dis, 2023,14(4):253
Duseja R, Heir R, Lewitus GM, et al. Astrocytic TNFα regulates the behavioral response to antidepressants. Brain Behav Immun, 2015,44:187–194
Steru L, Chermat R, Thierry B, et al. The tail suspension test: A new method for screening antidepressants in mice. Psychopharmacology, 1985,85(3):367–370
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The authors declared that they have no conflicts of interest to this work.
Additional information
This study was supported by the National Natural Science Foundation of China Young Scientists Fund (No. 81801216, No. 81802143, and No. 81901966) and the China Postdoctoral Foundation (No. 2018M633748).
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1007/s11596-024-2864-4
Supplementary data
About this article
Cite this article
Quan, X., Ma, T., Guo, K. et al. RETRACTED ARTICLE: Hydralazine Promotes Central Nervous System Recovery after Spinal Cord Injury by Suppressing Oxidative Stress and Inflammation through Macrophage Regulation. CURR MED SCI 43, 749–758 (2023). https://doi.org/10.1007/s11596-023-2767-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-023-2767-9