Abstract
Objective
Despite the recent advances in diagnosis and treatment, sepsis continues to lead to high morbidity and mortality. Early diagnosis and prompt treatment are essential to save lives. However, most biomarkers can only help to diagnose sepsis, but cannot predict the development of septic shock in high-risk patients. The present study determined whether the combined measurement of procalcitonin (PCT), thromboelastography (TEG) and platelet (PLT) count can predict the development of septic shock.
Methods
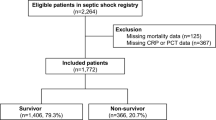
A retrospective study was conducted on 175 septic patients who were admitted to the intensive care unit between January 2017 and February 2021. These patients were divided into two groups: 73 patients who developed septic shock were assigned to the septic shock group, while the remaining 102 patients were assigned to the sepsis group. Then, the demographic, clinical and laboratory data were recorded, and the predictive values of PCT, TEG and PLT count for the development of septic shock were analyzed.
Results
Compared to the sepsis group, the septic shock group had statistically lower PLT count and TEG measurements in the R value, K value, α angle, maximum amplitude, and coagulation index, but had longer prothrombin time (DT), longer activated partial thromboplastin time (APTT), and higher PCT levels. Furthermore, the Sequential Organ Failure Assessment (SOFA) score was higher in the septic shock group. The multivariate logistic regression analysis revealed that PCT, TEG and PLT count were associated with the development of septic shock. The area under the curve analysis revealed that the combined measurement of PCT, TEG and PLT count can be used to predict the development of septic shock with higher accuracy, when compared to individual measurements.
Conclusion
The combined measurement of PCT, TEG and PLT count is a novel approach to predict the development of septic shock in high-risk patients.
Similar content being viewed by others
References
Kumar S, Tripathy S, Jyoti A, et al. Recent advances in biosensors for diagnosis and detection of sepsis: A comprehensive review. Biosens Bioelectron, 2019,124–125:205–215
Kerrigan SW, Devine T, Fitzpatrick G, et al. Early Host Interactions That Drive the Dysregulated Response in Sepsis. Front Immunol, 2019,10:1748
Caraballo C, Jaimes F. Organ Dysfunction in Sepsis: An Ominous Trajectory From Infection To Death. Yale J Biol Med, 2019,92(4):629–640
Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: Guideline-based management. Cleve Clin J Med, 2020,87(1):53–64
Levinson AT, Casserly BP, Levy MM. Reducing mortality in severe sepsis and septic shock. Semin Respir Crit Care Med, 2011,32(2):195–205
Hunton R. Seeking a balanced approach to implementing sepsis guidelines. JAAPA, 2020,33(7):13–17
Gauer RL. Early recognition and management of sepsis in adults: the first six hours. Am Fam Physician, 2013,88(1):44–53
Hotchkiss RS, Moldawer LL, Opal SM, et al. Sepsis and septic shock. Nat Rev Dis Primers, 2016,2:16045
Blanco J, Muriel-Bombin A, Sagredo V, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care, 2008,12(6):R158
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med, 2003,348(16):1546–1554
Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med, 2001,29(7):1303–1310
Hung SK, Lan HM, Han ST, et al. Current Evidence and Limitation of Biomarkers for Detecting Sepsis and Systemic Infection. Biomedicines, 2020,8(11):494
Teggert A, Datta H, Ali Z. Biomarkers for Point-of-Care Diagnosis of Sepsis. Micromachines (Basel), 2020,11(3):286
Bozza FA, Salluh JI, Japiassu AM, et al. Cytokine profiles as markers of disease severity in sepsis: a multiplex analysis. Crit Care, 2007,11(2):R49
Liu D, Su L, Han G, et al. Prognostic Value of Procalcitonin in Adult Patients with Sepsis: A Systematic Review and Meta-Analysis. PLoS One, 2015,10(6):e0129450
Gregoriano C, Heilmann E, Molitor A, et al. Role of procalcitonin use in the management of sepsis. J Thorac Dis, 2020,12(Suppl 1):S5–S15
Becker KL, Snider R, Nylen ES. Procalcitonin in sepsis and systemic inflammation: a harmful biomarker and a therapeutic target. Br J Pharmacol, 2010,159(2):253–264
Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock — Basics of diagnosis, pathophysiology and clinical decision making. Medi Clin North Am, 2020,104(4):573–585
Simmons J, Pittet JF. The coagulopathy of acute sepsis. Curr Opin Anaesthesiol, 2015,28(2):227–236
Ding R, Meng Y, Ma X. The Central Role of the Inflammatory Response in Understanding the Heterogeneity of Sepsis-3. Biomed Res Int, 2018,2018:5086516
Bosmann M, Ward PA. The inflammatory response in sepsis. Trends Immunol, 2013,34(3):129–136
Tsao CM, Ho ST, Wu CC. Coagulation abnormalities in sepsis. Acta Anaesthesiol Taiwan, 2015,53(1):16–22
Muller MC, Meijers JC, Vroom MB, et al. Utility of thromboelastography and/or thromboelastometry in adults with sepsis: a systematic review. Crit Care, 2014,18(1):R30
Muzaffar SN, Baronia AK, Azim A, et al. Thromboelastography for Evaluation of Coagulopathy in Nonbleeding Patients with Sepsis at Intensive Care Unit Admission. Indian J Crit Care Med, 2017,21(5):268–273
Guclu E, Durmaz Y, Karabay O. Effect of severe sepsis on platelet count and their indices. Afr Health Sci, 2013,13(2):333–338
Vardon-Bounes F, Ruiz S, Gratacap MP, et al. Platelets Are Critical Key Players in Sepsis. Int J Mol Sci, 2019,20(14):3494
Gibot S, Bene MC, Noel R, et al. Combination biomarkers to diagnose sepsis in the critically ill patient. Am J Respir Crit Care Med, 2012,186(1):65–71
Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 2016,315(8):775–787
Dewitte A, Lepreux S, Villeneuve J, et al. Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critically [corrected] ill patients? Ann Intensive Care, 2017,7(1):115
Iba T, Levy JH. Inflammation and thrombosis: roles of neutrophils, platelets and endothelial cells and their interactions in thrombus formation during sepsis. J Thromb Haemost, 2018,16(2):231–241
Chang JC. Sepsis and septic shock: endothelial molecular pathogenesis associated with vascular microthrombotic disease. Thromb J, 2019,17:10
Stief TW, Ijagha O, Weiste B, et al. Analysis of hemostasis alterations in sepsis. Blood Coagul Fibrinolysis, 2007,18(2):179–186
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The authors declare that they have no conflicts of interest.
Additional information
The study was supported by grants from the National Natural Science Foundation of China (No. 81903086), and the Shandong Provincial Natural Science Foundation of China (No. ZR2019QH014).
Rights and permissions
About this article
Cite this article
Zhao, Xs., Meng, Zl., Zhang, T. et al. Combining Serum Procalcitonin Level, Thromboelastography, and Platelet Count to Predict Short-term Development of Septic Shock in Intensive Care Unit. CURR MED SCI 43, 86–92 (2023). https://doi.org/10.1007/s11596-022-2689-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-022-2689-y